Research Article - Journal of Intensive and Critical Care Nursing (2023) Volume 6, Issue 6
Comparison of rapid shallow breathing index and integrative weaning index as weaning predictors among mechanically ventilated patients
Hemanth MS*
Department of Nursing, Banaras Hindu University, Uttar Pradesh, India
- Corresponding Author:
- Hemanth MS
Department of Nursing,
Banaras Hindu University,
Uttar Pradesh,
India
E-mail: hemanthms75@gmail.com
Received: 06-Jun-2023, Manuscript No. AAICCN-23-101561; Editor assigned: 08-Jun-2023, AAICCN-23-101561 (PQ); Reviewed: 22-Jun-2023, QC No. AAICCN-23-101561; Revised: 07-Aug-2023, Manuscript No. AAICCN-23-101561 (R); Published: 14-Aug-2023, DOI:10.35841/aaiccn.6.6.167
Citation: Hemanth MS. Comparison of rapid shallow breathing index and integrative weaning index as weaning predictors among mechanically ventilated patients. J Intensive Crit Care Nurs. 2023;6(6):1-5.
Abstract
Objective: The use of the Rapid Shallow Breathing Index (RSBI) is recommended in ICUs, where it is used as a predictor of Mechanical Ventilation (MV) weaning success. The aim of this study was to compare the performance of the RSBI calculated by the traditional method (described in 1991) with that of the RSBI calculated directly from MV parameters.
Methods: This was a prospective observational study involving patients who had been on MV for more than 24 h and were candidates for weaning. The RSBI was obtained by the same examiner using the two different methods (employing a spirometer and the parameters from the ventilator display) at random. In comparing the values obtained with the two methods, we used the Mann-Whitney test, Pearson's linear correlation test and Bland-Altman plots. The performance of the methods was compared by evaluation of the areas under the ROC curves.
Results: Of the 109 selected patients (60 males; mean age, 62 ± 20 years), 65 were successfully weaned, and 36 died. There were statistically significant differences between the two methods for respiratory rate, tidal volume and RSBI (p<0.001 for all). However, when the two methods were compared, the concordance and the intra-observer variation coefficient were 0.94 (0.92-0.96) and 11.16%, respectively. The area under the ROC curve was similar for both methods (0.81 ± 0.04 vs. 0.82 ± 0.04; p=0.935), which is relevant in the context of this study.
Conclusions: The satisfactory performance of the RSBI as a predictor of weaning success, regardless of the method employed, demonstrates the utility of the method using the mechanical ventilator.
Keywords
Respiration, Artificial, Ventilator weaning, Spirometry, Concordance
Introduction
Weaning is the gradual removal of ventilator assistance and weaning patients off artificial breathing as soon as possible is essential. Prolonged mechanical ventilation is associated with complications such as infections, particularly nosocomial pneumonia [1].
The criteria of readiness for the weaning trial include adequate oxygenation, as indicated by tidal volume >5 mL/kg, vital capacity >10 mL/kg, appropriate inspiratory effort, respiratory rate ≤ 35/min, PaO2 ≥ 60 mm of Hg and PaCO2 ≤ 60 mm of Hg, positive end expiratory pressure ≤ 8 cm H2O, no significant respiratory acidosis (pH ≥ 7.30), maximal inspiratory pressure (MIP) ≤ -20 to -25 cm H2O, O2 saturation > 90% on FiO2 ≤ 0.4 (or PaO2/FIO2 ≥ 200) and Rapid Shallow Breathing Index (RSBI) <105 along with subjective and objective assessments of respiratory and cardiovascular status [2].
The RSBI has been successfully used as a predictor of successful weaning in many studies. This index is calculated by dividing the patient's respiratory rate by tidal volume (RSBI=f/ VT). Khan, et al., identified rapid shallow breathing and diaphragmatic excursion as the best clinical predictors of extubation assurance and re-intubation prevention. He compared ultrasound-based diaphragmatic excursion and RSBI among 90 patients who were on artificial ventilation for more than 48 h in Islamabad, Pakistan [3].
In a systematic review including 43 studies (7929 patients), RSBI was the most common predictor of weaning from mechanical ventilation in 15 studies (2159 patients) [4].
The predictive performance of serial RSBI measurements was higher than that of a single RSBI measurement. However, few other factors that also contribute to extubation success, such as patient’s neurological status, amount of tracheobronchial secretions and ability to clear them, adequacy of cough and requirement of positive end expiratory pressure after extubation, should also be considered in the encoding of RSBI principles. This reason precludes us from using RSBI as the preferred tool for weaning [5].
Applying RSBI alone may be misleading. Patient's condition, concomitant illnesses and duration of stay in the Intensive Care Unit (ICU) should all be well-thought-out while weaning.
Kuo, et al., assessed the predictive value of RSBI in 188 patients with acute respiratory failure (on artificial ventilation for at least 48 h) at the national Taiwan university hospital's medical and surgical ICUs. They opined that RSBI assessed at the end of the spontaneous breathing trial was the best interpreter of successful weaning in critically ill patients compared with RSBI measured at the start of weaning [6].
According to a retrospective study conducted at the Chang Gung memorial hospital in Taiwan among 41 critically sick patients, the RSBI (32.5%), respiratory rate (22%) and minute ventilation (18%) are top three predictors of active extubation [7].
Wu, et al., combined the values of hemoglobin and serum albumin and GCS scores with the RSBI for evaluating the success of weaning. They together are better at predicting outcomes than RSBI alone [8].
An Integrative Weaning Index (IWI) integrates crucial weaning parameters along with the RSBI. The IWI incorporates respiratory system compliance, SaO2 and f/Vt ratio. Nemer, et al., argued that the IWI could predict extubation failure in 90% patients when used as weaning tool [9].
During weaning, the IWI is useful for predicting both successful and unsuccessful weaning outcomes. Consequently, its use as a routine weaning predictor for mechanically ventilated patients is encouraged [10].
Ebrahimabadi, et al., evaluated the ability of the IWI to predict the outcomes of spontaneous breathing trials in mechanically ventilated patients. They found that the IWI, as a more objective predictor, has sufficient accuracy and power for predicting the outcome of the 2-h SBT [11].
Huo, et al., reported that the IWI has the potential to act as a significant predictor of weaning success [12]. Wu, et al., further confirmed that in an adult medical intensive care unit. An integrative index incorporating serum albumin and hemoglobin values and GCS scores predicted extubation outcomes better than the RSBI alone [13]. The current research was conducted in the medical ICU of a tertiary level hospital. The primary researcher/principal investigator is a student of the “nurse practitioner in a critical care program” and the program was introduced in 2017 in India. Nurse practitioner students and individuals employed as faculty work in close association with intensive care physicians to contribute substantially toward providing comprehensive and holistic care to critically ill patients in the ICU.
Aims: The study compared the accuracy of the RSBI for active weaning with that of the IWI. The RSBI was calculated according to the standard formula (RSBI=f/VT). The study was conducted in a single tertiary care center among adult patients who were admitted to medical ICUs for mechanical ventilation.
Materials and Methods
We here attempted to address the following question: “What is the predictability of the RSBI versus the IWI in successful extubation of mechanically ventilated patients in the ICU?’
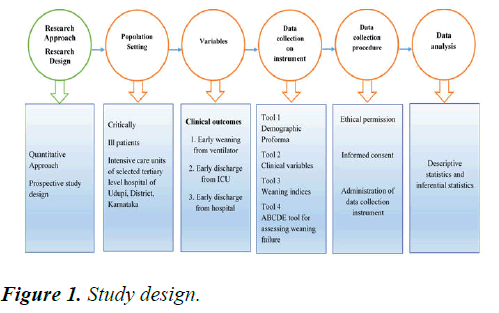
A comparative observational study design was adopted here to identify the relationship between the RSBI and the IWI in predicting successful extubation. The study design adopted is depicted in (Figure 1).
The sample consisted of critically sick patients who were admitted to the ICU and met.
The sampling criteria. A non-probability purposive sampling methodology was used in this study. The data were collected from 115 adult patients admitted to the ICU who were aged 18 years or older and on mechanical ventilation for at least 24 h. Patients who were intubated more than once, those with a tracheostomy tube, those with systolic BP>180 and <90 mmHg and those with neuromuscular disorders were excluded from the study. Administrative permission from the college of nursing and approval from the Institutional Ethics Committee (IEC no. 876/2020) were obtained. The research was registered in Clinical Trials Registry-India (CTRI/2021/02/031137). As the patients were unconscious, written informed consent was collected from a Legally Authorized Representative (LAR) of patient. The LAR’s signature was witnessed. Later, the signature was taken from patients who improved over time.
The following proforma were used to collect data such as demographic profile, clinical variables and weaning indices. The ABCDE tool was used for assessing weaning failure. The content of the proforma was validated by experts and any modifications were made based on the expert's suggestions. Demographic profile consisted of 12 items, namely hospital number, age, gender, chief complaint of the patient, diagnosis, co-morbid conditions, number of days in the ICU, number of days on the ventilator, indication for intubation, type of ICU, availability of the intensivist round the clock and re-intubation within the next 48 h. The checklist on clinical variables consisted of 25 items, namely mechanical ventilator settings such as FiO2, PEEP, tidal volume, respiratory rate, static compliance, minute ventilation and I:E ratio and hemodynamic parameters such as temperature, heart rate, blood pressure, SpO2 and capillary refill before and after the spontaneous breath trial. It also consisted items from the Glasgow coma scale and SOFA and APACHE2 scores. Variables of arterial blood gas such as pH, PCO2, PaO2 HCO3, P/F ratio, serum lactate, sodium and potassium were also included.
The questionnaire on weaning indices consisted of the RSBI and the IWI. The RSBI is a standardized tool developed and validated by Dr. Karl Yang, while the IWI is a standardized tool developed and validated by Sergio N Nemer. The IWI is calculated by static lung compliance multiplied by SaO2 and divided by the RSBI.
The ABCDE tool consisting of five variables was developed by the researcher to gather background information. Variables related to the airway included bronchospasm, pleural effusion, atelectasis and ascites and those related to the brain included delirium, anxiety and depression. Cardiac findings included ECG and 2D echo data. The diaphragm was assessed through ultrasound excursion. Electrolytes including serum sodium, serum potassium, calcium and magnesium were also evaluated.
All the questionnaires were pretested with five ICU patients. The time taken to collect the information from the patient/ family member (relative) and case record was approximately 15 min. No difficulty was faced in obtaining the data from the patient, patient relatives and case records.
The reliability of the checklists was evaluated in 20 patients aged between 18 and 95 years. The interrater reliability method was used to measure reliability. The investigator trained the observer for observing ventilator parameters, hemodynamic parameters, weaning indices and ABCDE assessment results. The reliability score obtained was 0.93.
A pilot study was conducted in 30 ICU patients to assess the feasibility for conducting a study. The data collection procedure used was exactly the same as that used for the main study. Written informed consent was obtained from patients/ caregivers after explaining them about the study in detail. Their questions were answered and clarifications were provided. Patient’s history of presenting complaints and basic information were collected using the demographic proforma and other questionnaires were administered to collect the mechanical ventilator and hemodynamic parameters. Individual results and scores were kept confidential.
Results
Data presented in Tables 1 and 2 shows that 105 (100%) patients had RSBI<105 and were successfully extubated from the mechanical ventilator compared with 96 (92.16%) patients with successful extubation from the mechanical ventilator and an IWI score of >25. Ten patients were re-intubated within 48 h from extubation, five (50%) patients had IWI<24 and 5 (50%) patients had IWI >25 and RSBI <105 (Table 3).
| Sample characteristics | Mean ± SD | Frequency (Percentage) |
|---|---|---|
| Age (years) | 53.18 ± 17.191 | |
| Gender | ||
| Male | 68 (59.1) | |
| Female | 47 (40.9) | |
| Number of days on mechanical ventilation | 3.00 ± 1.314 | |
| Number of days in ICU | 8.04 ± 1.2 | |
| Successful weaning, n (%) | 105 (91.3%) | |
| Weaning failure, n (%) | 10 (8.7%) | |
| SOFA score | 4.18 ± 1.218 | |
| <3 | 6 (5.2%) | |
| >3 | 109 (94.8%) | |
| APACHE II score | 8.37 ± 2.706 | |
| <10 | 104 (90.4%) | |
| >10 | 11 (9.6%) | |
Table 1. Frequency and percentage of clinical characteristics (N=115).
| Variable | Frequency | Percentage |
|---|---|---|
| Ascites | 1 | 10% |
| Delirium | 7 | 70% |
| Anxiety | 8 | 80% |
Table 2. Causes of weaning failure as assessed by ABCDE (N=10).
| Successful extubation from the mechanical ventilator (105) | Frequency | Percentage |
|---|---|---|
| RSBI<105 | 105 | 100% |
| RSBI>106 | 0 | 0% |
| IWI>25 | 96 | 92.16% |
| IWI<24 | 9 | 8.64% |
| Weaning failure within 48 h (10) | Frequency | Percentage |
| RSBI>106 | 0 | 0% |
| IWI<24 | 5 | 50% |
| IWI>25 and RSBI<105 | 5 | 50% |
Table 3. Successful extubation and re-intubation within 48 h (N=115).
Discussion
Of the 115 patients, 58 (50.4%) patients complained of respiratory problems, 54 (47%) were having other comorbidities (such as surgical, obstetric and gynecological problems). All 115 (100%) patients were on mechanical ventilation for more than 48 h. Of them, 80 (69.6%) patients were intubated for respiratory distress. Only 10 (8.7%) patients were re-intubated within 48 h after extubation.
We used two different indices (RSBI vs. IWI) to predict successful extubation. An RSBI score of <105 is considered an indicator for successful extubation. However, in the present study, all the patients had RSBI <105. However, despite have a good RSBI score, 10 patients had weaning failure. A systematic review revealed that RSBI is commonly used as a predictor for weaning outcomes [14]. Goharani, et al., reported that an RSBI value of ≤ 85 breaths/min/L would be more appropriate for patients with chronic obstructive pulmonary disease [15]. Our study population in a multidisciplinary unit was a mixed group including those with trauma, postoperative, sepsis, toxicological issues and various comorbid conditions. RSBI of ≤ 105 breaths/min/L had a sensitivity of only 94.8% to predict successful extubation [16]. A decreased RSBI value could more successfully predict extubation, with the average value being 41.9 breaths/min/L [17]. Another study claimed that RSBI <98 has a higher predictive value and sensitivity [18]. A metaanalysis revealed that RSBI has a moderate sensitivity (pooled sensitivity) and poor specificity in predicting weaning outcomes [19].
In the present study, 96 (92.16%) patients who had IWI>25 were successfully extubated. Of the 10 patients who experienced weaning failure and required re-intubation within 48 h, 5 patients had IWI<24. The IWI was found to be better in predicting successful extubation than the RSBI. The IWI encompasses f/VT, measures of oxygenation and lung compliance (IWI=Cst × SaO2/RR/TV) [20]. The IWI was beneficial in successfully predicting extubation in elderly patients who form a significant portion of the ICU population. An IWI of 28 mL/cm H2O breaths/min/L was a good predictor of weaning success among patients with cirrhosis who were on mechanical ventilation [21]. According to the present study findings, the IWI has a better specificity than the RSBI in predicting weaning and extubation success.
This study was conducted in a single setting with more than 50 ICU beds; however, data from multiple sites could have strengthened the power of samples. The purposive sampling methodology restricts the generalizability of the findings. A larger sample size and a specific patient population could add more vigor to the findings.
Conclusion
The study findings have implications for the practice of nurse practitioners. The job description of the nurse practitioners are not yet uniform across India. The job description of nursing graduates placed in private hospitals is designed according to the needs of the settings. In addition to intensivists, weaning and extubation monitoring privileges may be granted to nurse practitioners with critical care training. For nations with limited resources, such as India, this model might be quite helpful.
References
- Azeredo LM, Nemer SN, Sv Barbas C, et al. The integrative weaning index in elderly icu subjects. Respir Care. 2017;62(3):333-9.
[Crossref] [Google Scholar] [PubMed]
- Baptistella AR, Sarmento FJ, Da Silva KR, et al. Predictive factors of weaning from mechanical ventilation and extubation outcome: A systematic review. J Crit Care.2018a; 48:56-62.
[Crossref] [Google Scholar] [PubMed]
- Baptistella AR, Sarmento FJ, Da Silva KR, et al. Predictive factors of weaning from mechanical ventilation and extubation outcome: A systematic review. J Crit Care. 2018b;48:56-62.
[Crossref] [Google Scholar] [PubMed]
- Ebrahimabadi S, Moghadam AB, Vakili M, et al. Studying the power of the integrative weaning index in predicting the success rate of the spontaneous breathing trial in patients under mechanical ventilation. Indian J Crit Care Med. 2017;21(8):488-93.
[Crossref] [Google Scholar] [PubMed]
- Fadaii A, Amini S, Bagheri B, et al. Assessment of rapid shallow breathing index as a predictor for weaning in respiratory care unit. Tanaffos. 2012;11(3):28-31.
[Crossref] [Google Scholar] [PubMed]
- Figueroa Casas JB, Montoya R, Garcia Blanco J, et al. Effect of using the rapid shallow breathing index as readiness criterion for spontaneous breathing trials in a weaning protocol. Am J Med Sci. 2020;359(2):117-22.
[Crossref] [Google Scholar] [PubMed]
- Ghiasi F, Moghadam KG, Alikiaii B, et al. The prognostic value of rapid shallow breathing index and physiologic dead space for weaning success in intensive care unit patients under mechanical ventilation. J Res Med Sci. 2020.1
[Crossref] [Google Scholar] [PubMed]
- Goharani R, Vahedian Azimi A, Galal IH, et al. A rapid shallow breathing index threshold of 85 best predicts extubation success in chronic obstructive pulmonary disease patients with hypercapnic respiratory failure. J Thorac Dis. 2019;11(4):1223-32.
[Crossref] [Google Scholar] [PubMed]
- Huo Y, Guo S, Zhang K, et al. A clinical study on the ability of the integrative weaning index to predict weaning from mechanical ventilation. Ann Cardiothorac Surg. 2020 ;9:3162-69.
[Crossref] [Google Scholar] [PubMed]
- Karthika M, Al Enezi FA, Pillai Lv, et al. Rapid shallow breathing index. Ann Thorac Med. 2016;11(3):167.
[Crossref] [Google Scholar] [PubMed]
- Khan MT, Munawar K, Hussain SW, et al. Comparing ultrasound-based diaphragmatic excursion with rapid shallow breathing index as a weaning predictor. Cureus. 2018;10(12).
[Crossref] [Google Scholar] [PubMed]
- Kuo PH, Wu HD, Lu BY, et al. Predictive value of rapid shallow breathing index measured at initiation and termination of a 2-hour spontaneous breathing trial for weaning outcome in ICU patients. J Formos Med Assoc. 2016;105(5):390-98.
[Crossref] [Google Scholar] [PubMed]
- Leonov Y, Kisil I, Perlov A, et al. Predictors of successful weaning in patients requiring extremely prolonged mechanical ventilation. Adv Respir. 2020;88(6):477-84.
[Crossref] [Google Scholar] [PubMed]
- Nemer SN, Sv Barbas C, Caldeira JB, et al. Open access a new integrative weaning index of discontinuation from mechanical ventilation. Crit Care. 2009a;1-9.
[Crossref] [Google Scholar] [PubMed]
- Nemer SN, Sv Barbas C, Caldeira JB, et al. Open access a new integrative weaning index of discontinuation from mechanical ventilation. Crit Care. 2009;13(5):152.
[Crossref] [Google Scholar] [PubMed]
- Sahu S, Saluja V, Sharma A, et al. Anaesthesiolo evaluation of the integrative weaning index for predicting the outcome of spontaneous breathing trial in patients with cirrhosis on mechanical ventilation: A pilot study main points. Turk J Anaesthesiol Reanim. 2022;50(2):107.
[Crossref] [Google Scholar] [PubMed]
- Trivedi V, Chaudhuri D, Jinah R, et al. The usefulness of the rapid shallow breathing index in predicting successful extubation: A systematic review and meta-analysis. Chest. 2022;161(1):97–111.
[Crossref] [Google Scholar] [PubMed]
- Tu CS, Chang CH, Chang SC, et al. A decision for predicting successful extubation of patients in intensive care unit. BioMed Res Int. 2018.
[Crossref] [Google Scholar] [PubMed]
- Wu TJ, Shiao JSC, Yu HL, et al. An integrative index for predicting extubation outcomes after successful completion of a spontaneous breathing trial in an adult medical intensive care unit. J Intensive Care Med. 2019;34(8):640-45.
[Crossref] [Google Scholar] [PubMed]
- Zein H, Baratloo A, Negida A, et al. Ventilator weaning and spontaneous breathing trials; an educational review. Emergency. 2016;4(2):65-71.
[Google Scholar] [PubMed]
- Zeng XT, Hu H, Lyu J, et al. risk factors of ventilator associated pneumonia in critically iii patients. Front pharmacol. 2019;10:482.
[Crossref] [Google Scholar] [PubMed]