Review Article - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 1
Valsalva retinopathy: Clinical features and management strategies
Selda Celik Dulger*, Mehmet Yasin Teke
Department of Ophthalmology, University of Health Sciences, Ankara Ulucanlar Eye Training and Research Hospital, Ankara, Turkey
- Corresponding Author:
- Dr. Selda Celik Dulger
Department of Ophthalmology
University of Health Sciences
Ankara Ulucanlar Eye Training and Research Hospital
Ankara Turkey
E-mail: drsldck@gmail.com
Accepted date: 18 December, 2020
Citation: Dulger SC, Teke MY. Valsalva retinopathy: Clinical features and management strategies. J Clin Ophthalmol 2021;5(1):323-324.
Abstract
Valsalva retinopathy is an uncommon disease which presents itself with sudden vision loss secondary to pre-retinal hemorrhage. There are several treatment modalities depending on the size, thickness and anatomical location of hemorrhage, but optimal treatment is still not guided. In this mini review, we evaluated clinical features and treatment options of valsalva retinopathy and proposed guidance on management of valsalva retinopathy.
Keywords
Argon laser hyaloidotomy, Nd:YAG laser hyaloidotomy, Pre-retinal hemorrhage, Valsalva retinopathy, Vitrectomy.
Introduction
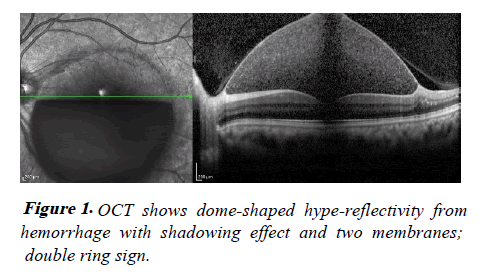
Valsalva retinopathy was first described in 1972 by Thomas Duane to include retinal hemorrhages that are secondary to the increase of intra-thoracic and intra-abdominal pressure with Valsalva maneuver [1]. Retinal hemorrhages mostly occurs subhyaloid, sub internal limiting membrane (ILM) but rarely located in retinal layer and vitreous. If blood is trapped in both spaces, it represents ‘’double ring sign’’. The outer ring represents subhyaloid bleeding and the inner one represents sub-ILM bleeding. Biomicroscopic evaluation reveals domeshaped acute macular hemorrhage, but anatomic level of hemorrhage is not detected ophthalmoscopically. OCT images are very useful in identifying the location of hemorrhages. Shukla et al. showed two distinct membranes on OCT scans, the more reflective and apparent one was determined as ILM and the other shadowy and patchy overlying membrane was determined as posterior hyaloid [2] (Figure 1). Hemorrhages secondary to Valsalva maneuver has a predilection for the macula, in the vast majority of cases, lead severe visual impairment. The most common presenting symptom is sudden vision loss or central scotoma. The severity of the symptoms depends on the thickness, size and anatomic level of the hemorrhage.
Although there are several treatment modalities depending on the size, thickness and anatomical location of hemorrhage, such as observation, neodymium-doped yttrium aluminium garnet (Nd-YAG) hyaloidotomy, argon laser, pneumatic displacement of the hemorrhage and vitrectomy, optimal management is still not guided. In this review, we evaluated alternative management options of valsalva retinopathy in the light of the literature [3].
Literature Review
Treatment in most cases involves only observation, anyway the hemorrhage size smaller than one disc diameter tends to resolve spontaneously in a short period of time. Spontaneous resorption of larger hemorrhages may take longer, sometimes months. In the literature, some authors advocate that up to 3 months of observation is acceptable for spontaneous resolution, while others advocate early intervention is crucial to prevent irreversible retinal damage owing to prolonged contact with hemoglobin and its precursor. Longstanding hemorrhage may result preretinal tractional membrane or proliferative vitreoretinopathy. Resorption of sub-ILM hemorrhage usually tends to take longer than subhyaloid hemorrhage [4,5].
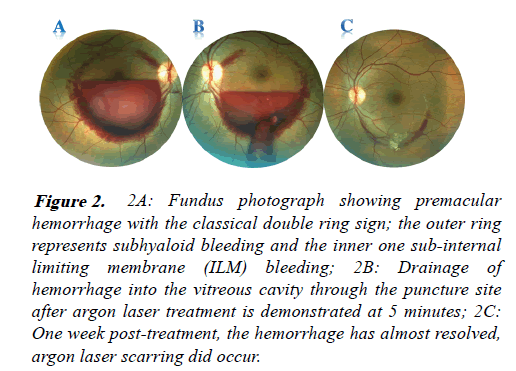
Laser drainage being a simple, quick, inexpensive, office-based procedure accelerate the process by enabling the extensive premacular hemorrhage an opening in to the vitreous cavity and facilitate cleansing blood cells. Nd:YAG laser hyaloidotomy for premacular hemorrhages was first described by Faulborn [6]. Though there are still controversies on the ideal timing for YAG laser hyaloidotomy, several studies suggest that it is more effective within 3 weeks after the onset of hemorrhage. However, it could be performed in older bleedings if there are no sign of clotting and dehemoglobinization. In the literature, YAG laser was successfully performed in two cases with symptoms for more than 45 days. A recent report by us indicated that Nd:YAG laser hyaloidotomy was safe and effective approach for hemorrhage larger than 4 disc diameter (DD). All patients in our study who underwent laser membranotomy had less than 3- week duration of hemorrhage. When the drainage with Nd:YAG laser is impossible, anterior surface of the hematoma may be punctured with argon green laser instead of increasing the energy level of Nd:YAG laser, as in our two cases (Figure 2).
Figure 2:2A: Fundus photograph showing premacular hemorrhage with the classical double ring sign; the outer ring represents subhyaloid bleeding and the inner one sub-internal limiting membrane (ILM) bleeding; 2B: Drainage of hemorrhage into the vitreous cavity through the puncture site after argon laser treatment is demonstrated at 5 minutes; 2C: One week post-treatment, the hemorrhage has almost resolved, argon laser scarring did occur
There are some previous reports regarding premacular drainage by means of only argon laser or combination of Nd:YAG laser. Argon green laser application before YAG laser increases the penetration of Nd:YAG laser spots by making hyaloid and/or ILM more stable and taut [4,7]. In our study, thirteen eyes which had premacular hemorrhage smaller than or equal to 4 DD, were observed for spontaneous resolution and achieved 20/20 visual acuity within 6 months.
Another study reported that hemorrhage larger than 3 DD with no longer 3 weeks may be a good candidate for Nd:YAG laser hyaloidotomy, but potential risks of the treatment should also be considered [8]. It is necessary to pay attention to the size of hemorrhage as well as proximity between the posterior hyaloid and underlying retina on OCT scans to avoid inadvertent retinal damage. In addition, the energy level required to make an opening over the membrane is important in the formation retinal damage. In the literature, there are many reports on the use of Nd:YAG laser in a wide range energy levels. We have achieved successful results at energy level between 1-10 mg at our clinical practice, in line with some previous studies.
Laser drainage has rarely been associated with serious complications such as macular hole formation, epiretinal membrane, retinal detachment and persistent premacular cavity. Epiretinal membrane is relatively common complication due to growth factor by stimulating trapped blood cells between ILM and retinal surface. It has been proposed that this often occurs after the drainage of sub-ILM hemorrhage as laser drainage stimulates gliotic activity at the basal membrane.
In some circumstances, treatment with vitrectomy is more effective and safer than other treatment options, precluding blood and laser-related complications. Especially if there is an insufficient spontaneous resorption or no drainage with Nd:YAG laser due to coagulated blood, vitrectomy can be the best treatment option. Although vitrectomy allows immediate visual recovery and definition of hemorrhage levels, have numerous serious complications such as nuclear sclerosis, retinal break, retinal detachment and endophthalmitis.
Recombinant plasminogen activator and gas have been used successfully to promote displacement of the blood under the hyaloid or ILM.
Discussion and Conclusion
Summary, observation and laser drainage seem to be best treatment approaches for valsalva retinopathy. Size, duration, thickness and anatomical location of the hemorrhage are the most important factors affecting treatment choice regarding observation or intervention. Hemorrhages equal or smaller than 4D can be treated effectively and safely with conservative treatment in accordance with previous reports. Nd:YAG laser and argon laser hyaloidotomy are cost saving, effective and safe outpatient treatment modalities when used for suitable patients with appropriate power settings.
References
- Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298-313.
- Shukla D, Naresh KB, Kim R. Optical coherence tomography findings in valsalva retinopathy. Am J Ophthalmol. 2005;140:134-6.
- Celik Dulger S, Ozdal PC, Teke MY. Valsalva retinopathy: Long-term results and management strategies. Eur J Ophthalmol. 2020;59:3-29.
- Meyer CH, Mennel S, Rodrigues EB, et al. Persistent premacular cavity after membranotomy in valsalva retinopathy evident by optical coherence tomography. Retina. 2006;26:116-8.
- De Maeyer K, Van Ginderdeuren R, Postelmans L, et al. Sub-inner limiting membrane haemorrhage: Causes and treatment with vitrectomy. Br J Ophthalmol. 2007;91:869-72.
- Durukan AH, Kerimoglu H, Erdurman C, et al. Long-term results of Nd:YAG laser treatment for premacular subhyaloid haemorrhage owing to Valsalva retinopathy. Eye. 2008;22:214-8.
- Ulbig MW, Mangouritsas G, Rothbacher HH, et al. Long-term results after drainage of premacularsubhyaloid hemorrhage into the vitreous with a pulsed Nd:YAG laser. Arch Ophthalmol. 1998;116:1465-9.
- Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd:YAG laser membranotomy in valsalva retinopathy. Am J Ophthalmol. 2003; 136: 763-6.