Research Article - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 2
The effect of intracameral ketorolac in cataract surgery for diabetic patients
Hatem M Marey1, Fatma K Genedy2*, Ahmed I Basiony11Faculty of Medicine, Menofia University, Menoufia, Egypt
2Faculty of Medicine, Cairo University, Egypt
- Corresponding Author:
- Dr. Fatma K Genedy
Faculty of Medicine
Cairo University
Egypt
E-mail: fatmakhairy171@yahoo.com
Accepted date: 16 April, 2020
Citation: Marey HM, Genedy FK, Basiony AI. The effect of intracameral ketorolac in cataract surgery for diabetic patients. J Clin Ophthalmol 2020;4(2):245-249.
Abstract
Aim: This study aims to assess the effect of intracameral ketorolac interaoperatively in cataract surgery for diabetic patients. Purpose: This study aims to assess the effect of intracameral ketorolac in cataract surgery for diabetic patients.
Methods: This study was conducted on cataract patients who need phacoemulsification subjected to ophthalmology department of Menoufia university careful history and ophthalmological examination was done including best corrected visual acuity, slit-lamp examination, fundus examination. All patients were dilated preoperatively by topical tropicamid 1% as mydriatc, and were operated under local peribulbar anesthesia and measurement of pupil diameter by squint caliper at the beginning and at the end of surgery and for standerization systemic and topical NSAIDS were prohibited preoperative. We assed the pupil diameter and surgical time intraoperative
Results: The mean pupillary diameter at the end of the operation in first group (non-ketorolac) was 7.18 ± 1.09 mm while in the second (ketorolac) group was 7.98 ± 1.34 mm with p value <0.05 which is statistically significant. On measuring the change that occur to the pupil diameter during surgery in group I it was 1.48 ± 0.77 mean while in group II it was 1.11 ± 0.66 with p value <0.01 which is highly significant also there was significant effect of interacameral ketorolac in decreasing corneal edema. As regard surgical time: In group I the mean surgical time in minutes was 24.73 ± 9.72 while in group II it was 22.77 ± 7.10 which shows that there is decrease in surgical time in ketorolac group but not significant.
Conclusion: Intracameral ketorolac is safe in maintaining pupil dilated especially in poorly dilated pupil.
Keywords
Intracameral, ketorolac, cataract surgery, diabetics
Introduction
Cataract is an important cause of blindness globally and as of 2002, they accounted for approximately 50 % of all surgical cases [1]. Age-related cataracts affect more than 22 million people, and it is estimated that this number will rise to 30 million by 2020 [2]. As a consequence, cataract surgery is the most common surgical procedure performed in the world [3].
Maintaining mydriasis during cataract surgery is essential for ensuring patient safety and the efficiency of the surgical procedure [4,5]. Poorly dilated pupil is one of the most common problems faced by cataract surgeons and is associated with a higher incidence of intraoperative complications such as capsular rupture and vitreous loss [6].
There are many causes of poor mydriasis, for example, diabetes mellitus, senile miosis, intraoperative floppy iris syndrome, pseudo exfoliation syndrome, uveitis with posterior synechiae, and some conditions after ocular surgery [7].
The ability of the pupil to dilate well should be determined in the outpatient clinic. Both topical cycloplegic mydriatics and sympathomimetic agents should be administered to assess dilatation of the pupil. Pharmacological dilatation might break posterior synechiae preoperatively. Even if adequate pupil dilatation is not achieved by this preoperative office regimen, it allows the surgeon to plan an intraoperative pupil management strategy [8].
The goal of managing miotic pupils is to achieve adequate pupil size during surgery to perform phacoemulsification while still maintaining pupillary reactivity, near-normal pupil contour, and excellent visual results [9]. A 5.5 mm or larger pupil allows use of divide and conquer or other phacoemulsification techniques and a capsulorhexis of 4.0-5.0 mm could be easily performed [10].
A small pupil may cause damage to the patient ’ s eye by emulsification of the iris or may cause complications such as sphincteric tears, intraoperative bleeding, zonular dialysis, posterior capsular tear, or nucleus drop. Prolonged surgical time and increased maneuvering may result in postoperative complications such as striate keratopathy, uveitis, secondary glaucoma, irregular pupil, endophthalmitis and cystoid macular edema in addition to atrophic iris, which result in suboptimal surgical outcome and an unsatisfied patient [11].
Several methods have been developed for enlarging miotic pupils during phacoemulsification including iris retractors, multiple sphincterotomies, and pupil stretch techniques [12].
Subjects and methods
This study was conducted at ophthalmology department of Menoufia university informed consent was obtained from all patients.
Sixty diabetic’s patients (36 male, 24 female) all of them was among 20-70 years old, all diagnosed with cataract and need phacoemulsification surgery. Patients who have hypersensitivity to any NSAID or aspirin or to tetracaine, lidocaine, or any fluoroquinolone, presence of clinically significant medical conditions, patients with glaucoma or pseudoexfoliation syndrome were excluded. Use of other NSAIDs rather than the screening ophthalmological NSAIDs within 7 days before surgery, anticoagulants or antiplatelet agents within 14 days before surgery was prohibited. All patients were subjected to history taking including personal history (name, age, gender, occupation, and residence), complaint, present history and past history especially ophthalmic history. They underwent Ophthalmological examination including assessment of the visual acuity, and Slit lamp bio-microscopy examination to determine the type of cataract, fundus examination using Volk 90 D lens.
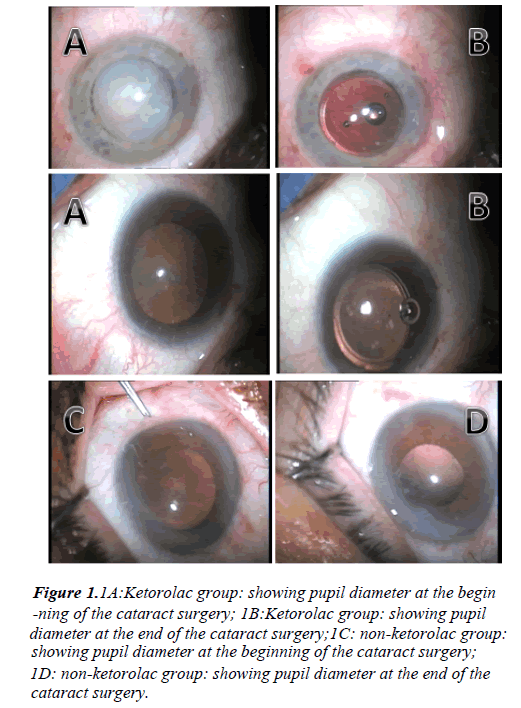
All patients were dilated preoperatively by topical tropicamid 1% (mydriacil®) as mydriatc, and were operated under local peribulbar anesthesia .they were divided into 2 groups. Group I: (non-ketorolac group) nothing was added to the irrigating fluid. Group II: (ketorolac group): ketorolac 0.3% was added to the irrigating fluid. And measurement of pupil diameter measured by squint caliper at the beginning and at the end of surgery (Figure 1).
Figure 1: .1A:Ketorolac group: showing pupil diameter at the begin
-ning of the cataract surgery; 1B:Ketorolac group: showing pupil diameter at the end of the cataract surgery;1C: non-ketorolac group: showing pupil diameter at the beginning of the cataract surgery;
1D: non-ketorolac group: showing pupil diameter at the end of the
cataract surgery.
Follow up protocol: We assed the pupil diameter and surgical time intraoperative and examined patients post operatively for any signs of drug toxicity eg: A.C reaction (cells and flare), corneal edema, at the day of operation and 3 days after the operation.
Results
Sixty eyes of 60 diabetic patients (36 male, 24 female) were included in this study.
Pupil diameter: The pupillary diameter was measured by a caliper at the beginning of the surgery and at the end ,the mean pupillary diameter at the end of the operation in first group was 7.18 ± 1.09 mm while in the second (ketorolac) group was 7.98 ± 1.34 mm with p value <0.05 which is statistically significant. On measuring the change that occur to the pupil diameter during surgery in group I it was 1.48 ± 0.77 while in group II it was 1.11 ± 0.66 with p value<0.01 which is highly significant (Table 1).
| Group I | Group II | Test of sig. | p | |||
|---|---|---|---|---|---|---|
| (n=30) | (n=30) | |||||
| No. | % | No. | % | |||
| Sex | ||||||
| Male | 17 | 56.7 | 19 | 63.3 | c2=0.278 | 0.598 |
| Female | 13 | 43.3 | 11 | 36.7 | ||
| Age | ||||||
| Min-Max | 42.0-90.0 | 45.0-83.0 | t=1.753 | 0.085 | ||
| Mean ± SD | 66.47 ± 10.61 | 61.60 ± 10.89 | ||||
| Median (IQR) | 65.0(59.0-74.0) | 61.0(53.0-69.0) | ||||
Table 1. Comparison between the two studied groups according to demographic data.
As regard surgical time: In group I the mean surgical time in minutes was 24.73 ± 9.72 while in group II it was 22.77 ± 7.10 with p value 0.667 which shows that there is decrease in surgical time in ketorolac group but not significant.
According to corneal edema: In the first day of operation: There was no corneal edema in 56.7% of cases of group I and was no corneal edema in 86.7% of cases of group II. In group I cases with mild corneal edema was 23.3%while in group II it was 10%, and those of moderate corneal edema in group I was 20%while in group II it was 3.3% with p value <0.05 which is statistically significant.
3 days after the operation: there was no corneal edema in 80% of cases of group I and was no corneal edema in 100% of case of group II .and mild corneal edema was 20% in group I while in group II it was 0% with p value <0.05 which is statistically significant (Table 2).
| Group I | Group II | c2 | p | |||
|---|---|---|---|---|---|---|
| (n=30) | (n=30) | |||||
| No. | % | No. | % | |||
| Type of DM | ||||||
| Type 1 | 2 | 6.7 | 1 | 3.3 | 0.351 | FEp=1 |
| Type 2 | 28 | 93.3 | 29 | 96.7 | ||
| Type of cataract | ||||||
| Cortical | 9 | 30 | 11 | 36.7 | 0.3 | 0.584 |
| PSC | 22 | 73.3 | 17 | 56.7 | 1.832 | 0.176 |
| Nucular2 | 1 | 3.3 | 2 | 6.7 | 0.351 | FEp=1.000 |
| Nucular3 | 16 | 53.3 | 10 | 33.3 | 2.443 | 0.118 |
| Mature white cataract | 0 | 0 | 1 | 3.3 | 1.017 | FEp=1.000 |
Table 2. Comparison between the two studied groups according to type of DM and type of cataract.
Discussion
Adequate pupil dilation and maintenance of dilation are necessary for safe and efficient cataract surgery have shown that inadequate mydriasis or intraoperative miosis is associated with numerous complications such as vitreous loss and zonular breaks Preoperative use of non-steroidal anti-inflammatory drugs (NSAIDs) has been shown to prevent intraoperative miosis. When administered preoperatively, multiple daily dosing of the drug typically required however patient compliance can be a problem. It has been shown that even with good patient compliance; topical drops are washed out of the aqueous during surgery, which can substantially limit their effectiveness [13].
In our study there was a great effect for using intracameral ketorolac in dilatation and maintenance of pupillary dilatation from the beginning till the end of the surgery as the mean pupil diameter was 7.98 ± 1.34 with (p value 0.003) which is highly significant (Table 3).
| Pupil diameter | Group I | Group II | Test of sig. | p |
|---|---|---|---|---|
| (n=30) | (n=30) | |||
| At the beginning | ||||
| Min-Max | 6.50-10.50 | 6.75-10.75 | t=1.506 | 0.137 |
| Mean ± SD | 8.67 ± 1.06 | 9.08 ± 1.09 | ||
| Median (IQR) | 8.88(7.7-9.5) | 9.38(8.3-10.0) | ||
| At the end | ||||
| Min-Max | 5.20-9.70 | 5.75-10.00 | t=2.516* | 0.015* |
| Mean ± SD | 7.18 ± 1.09 | 7.98 ± 1.34 | ||
| Median (IQR) | 7.20(6.70-7.7) | 8.25(6.75-9.0) | ||
| Change | ↓1.48 ± 0.77 | ↓1.11 ± 0.66 | U=289.0* | 0.003* |
Table 3. Comparison between the two studied groups according to pupil diameter.
According to pupil diameter: Our results are comparable with results of the study conducted by Hovanesian et al. [14], in which clinical trials comprised 808 patients (403 treatments and 405 placebo). Phenylephrine 1.0%, ketorolac 0.3% was superior to placebo for the maintenance of mydriasis during, and reduction of ocular pain following, cataract surgery. The mean area under the curve (AUC) change from baseline in pupil diameter was 0.08 mm for treatment compared with −0.50 mm for placebo (p < .0001).
Another study done by Walter et al. [15] in which phenylephrine 1.0%-ketorolac 0.3% (Omidria) to the irrigation solution during femtosecond laser-assisted cataract surgery (FLACS) reduces surgical time and the need for pupil expansion devices compared with the irrigation solution containing epinephrine. Data were collected from 200 consecutive patients, 100 in each group. Patient demographics, including a mean baseline pupil size of 7.1 mm, were similar between the groups.
Other study was done by Lindstrom et al. [13] that was done to evaluate effect of interacameral ketorolac, phenylephrine injection for maintenance of pupil diameter was superior to placebo in maintaining intraoperative mydriasis, preventing miosis The weighted mean (standard error) difference (OMS302–placebo) in change in the area under the curve from baseline for pupil diameter was 0.590 ([0.049]; 95% confidence interval 0.494 to 0.686; p<0.0001).
Another study done by Donnenfeld et al. [16] which was done to compare the effect of omidria compared with balanced saline solution, ketorolac on pupil diameter in which p value of ketorolac was 0.004 statistically significant in maintain pupillary diltation.
According to the surgical time: In our study the mean surgical time in minutes , ketorolac group was 22.77+7.10 while in non-ketorolac group was 24.73+9.72 that shows that there is decrease in surgical time with p value 0.667 which is statistically non-significant this is explained by: Different surgeons, different cataract density (Table 4).
| Surgical time | Group I | Group II | U | p |
|---|---|---|---|---|
| (n=30) | (n=30) | |||
| Min-Max | 12.0-50.0 | 14.0-39.0 | 421 | 0.667 |
| Mean ± SD | 24.73 ± 9.72 | 22.77 ± 7.10 | ||
| Median (IQR) | 20.50(17.0-30.0) | 21.0(17.0-27.0) |
Table 4. Comparison between the two studied groups according to surgical time.
This result was comparable with study done by Walter et al. [15 which done to determine whether the addition of phenylephrine 1.0%-ketorolac 0.3% (Omidria) to the irrigation solution during femtosecond laser – assisted cataract surgery (FLACS) reduces surgical time and the need for pupil expansion devices compared with the irrigation solution containing epinephrine. Mean surgical times were significantly reduced in the phenylephrine – ketorolac group versus the epinephrine group (8.1 minutes versus 9.4 minutes) (p=0.007) (Table 5).
| Corneal edema | Group I | Group II | c2 | p | ||
|---|---|---|---|---|---|---|
| (n=30) | (n=30) | |||||
| No. | % | No. | % | |||
| 0 day | ||||||
| No | 17 | 56.7 | 26 | 86.7 | 6.805* | MCp=0.033* |
| Mild | 7 | 23.3 | 3 | 10 | ||
| Moderate | 6 | 20 | 1 | 3.3 | ||
| 3 day | ||||||
| No | 24 | 80 | 30 | 100 | 6.667* | FEp=0.024* |
| Mild | 6 | 20 | 0 | 0 | ||
Table 5. Comparison between the two studied groups according to corneal edema.
Conclusion
According to corneal edema, In the first day of surgery: In our study in ketorolac group 26 case s their corneas were clear, only 3 cases with mild corneal edema with p value 0.033 non ketorolac group 17 cases their corneas were clear while 7 cases with mild corneal edema, 6 cases with moderate edema.
3rd day of surgery: In non-ketorolac group 24 cases their corneas were clear, 6 cases with mild corneal edema, while in ketorolac group the thirty cases their corneas became clear with p value 0.024. So ketorolac is statistically significant in decrease corneal edema.
In our study there was no any systemic are local ocular reaction in the form of (cells, flare) from adding ketorolac ketorolac to the irrigating fluid.
References
- Resnikoff S, Pascolini D, Etya’Ale D, t al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844-51.
- Gollogly HE, Hodge DO, St. Sauver JL, et al. Increasing incidence of cataract surgery: Population-based study. J Cataract Refract Surg. 2013;39:1383-9.
- Trikha S, Turnbull AMJ, Morris RJ, et al. The journey to femtosecond laser-assisted cataract surgery: new beginnings or false dawn? Eye (Lond). 2013;27:461-73.
- Narendran N, Jaycock P, Johnston RL, et al. The Cataract National Dataset electronic multicentre audit of 55 567 operations:risk stratification for posterior capsule rupture and vitreous loss. Eye (Lond). 2009;23:31-7.
- Hashemi H, Seyedian MA, Mohammadpour M. Small pupil and cataract surgery. Curr Opin Ophthalmol. 2015;26:3-9.
- Akman A, Yilmaz G, Oto S, et al. Comparison of various pupil dilatation methods for phacoemulsification in eyes with a small pupil secondary to pseudoexfoliation. Ophthalmology. 2004;111:1693-8.
- Wilczynski M, Wierzchowski T, Synder A, et al. Results of phacoemulsification with Malyugin ring in comparison with manual iris stretching with hooks in eyes with narrow pupil. Eur J Ophthalmol. 2013;23:196-201.
- Schacknow PN, Samples JR. The glaucoma book, a practical, evidence-based approach to patient care. New York: Springer-Verlag 2010.
- Shepherd DM. The pupil stretch technique for miotic pupils in cataract surgery. Ophthalmic Surg. 1993;24:851-2
- Ghoneim AM, Wasfy TE. Results of pupil dilatation using Oasis ring in eyes with narrow pupil during phacoemulsification. Delta J Ophthalmol. 2017;18:143-8.
- Agarwal A, Agarwal A, Jacob S. Phacoemulsification. 4th ed New Delhi, India: Jaypee-Highlights Medical Publishers Inc. 2011; pp. 378.
- De Juan E, Jr Hickingbotham D. Flexible iris retractor. Am J Ophthalmol. 1991;111:776-7.
- Lindstrom RL, Loden JC, Walters TR, et al. Intracameral phenylephrine and ketorolac injection (OMS302) for maintenance of intraoperative pupil diameter and reduction of postoperative pain in intraocular lens replacement with phacoemulsification. Clin Ophthalmology. 2014;1735-44.
- Hovanesian JA, Sheppard JD, Trattler WB, et al. Intracameral phenylephrine and ketorolac during cataract surgery to maintain intraoperative mydriasis and reduce postoperative ocular pain: integrated results from 2 pivotal phase 3 studies. J Cataract Refract Surg. 2015;41:2060-8.
- Walter K, Delwadia N, Coben J. Continuous intracameral phenylephrine–ketorolac irrigation for miosis prevention in femtosecond laser–assisted cataract surgery: Reduction in surgical time and iris manipulation. J Cataract Refract Surg. 2019;45:465-9.
- Donnenfeld ED, Whitaker JS, Jackson MA, et al. Intracameral ketorolac and phenylephrine effect on intraoperative pupil diameter and postoperative pain in cataract surgery. J Cataract Refract Surg. 2017;43:597-605.