Research Article - Journal of Clinical Ophthalmology (2023) Volume 7, Issue 3
Temporary keratoprosthesis combined vitreoretinal surgery and keratoplasty: visual and surgical outcomes
Florence Cabot1*, D Wade Redick1, Nathan Pirakitikulr1, Ann V Quan1, Francesco Pozzo Giuffrida1, Diana Laura1, Nicolas A Yannuzzi1, Harry W Flynn1, Nimesh A Patel2
1Department of Ophthalmology, School of Medicine, Bascom Palmer Eye Institute, University of Miami-Miller, Miami, Florida, United States
2Department of Ophthalmology, Boston University, Boston, Massachusetts, United States
- Corresponding Author:
- Florence Cabot
Department of Ophthalmology,
University of Miami-Miller,
School of Medicine,
Miami,
Florida,
United States
E-mail: fcabot@med.miami.edu
Received: 05-Jan-2023, Manuscript No. AACOVS-23-85486; Editor assigned: 09-Jan-2023, AACOVS-23-85486 (PQ); Reviewed: 23-Jan-2023, QC No. AACOVS-23-85486; Revised: 09-Mar-2023, Manuscript No. AACOVS-23-85486 (R); Published: 17-Mar-2023, DOI:10.35841/aacovs.7.2.645-652
Citation:Cabot F, Redick DW, Pirakitikulr N, et al.. Temporary keratoprosthesis combined vitreoretinal surgery and keratoplasty: visual and surgical outcomes. J Clin Ophthalmol. 2023;7(2): 645-652.
Abstract
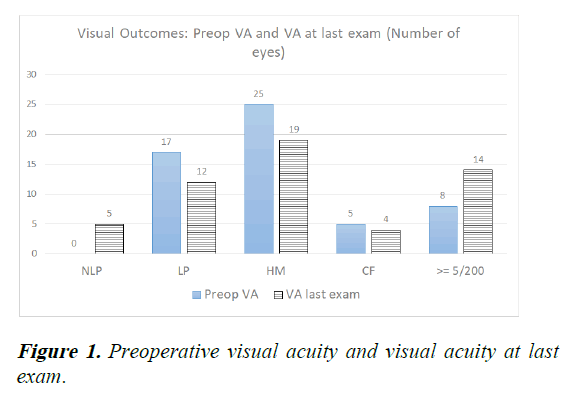
Background: Examine visual and surgical outcomes in combined Pars Plana Vitrectomy and Penetrating Keratoplasty using Temporary Keratoprosthesis (TKpro/PPV/PKP). Methods: Retrospective case series. All cases of TKpro/PPV/PKP performed at the Bascom Palmer eye institute in Miami, FL, from 2013 to 2020 were reviewed. The study included 55 eyes (55 patients). Results: Median follow-up was 18.4 months. Preoperative Visual Acuity (VA) ranged from Light Perception (LP) to 20/200. VA at last exam was ≥ 20/200 in 14 eyes (25%). VA of No Light Perception (NLP) occurred in 5 eyes postoperatively (9.1%). Enucleation was performed in 1 eye (1.8%) postoperatively. Corneal graft remained clear at last exam in 32 eyes (58%). There was no significant difference in percentage of eyes with VA ≥ 5/200 at last exam and rates of improvement in VA between eyes with infection and without infection (p=0.48; p=0.32). Infectious cases were less likely to have a clear graft at last exam (p=0.0019). There was no significant difference in rates of improvement in VA from preoperative between traumatic and non-traumatic cases (p=0.18). Preoperative VA of LP was associated with increased risk of NLP, enucleation or phthisis bulbi at last exam (p=0.0219). Conclusion: In the current study, infectious and non-infectious cases had similar visual outcomes although infectious cases were less likely to have a clear graft at last exam than non-infectious cases. Visual outcomes were similar between traumatic and non-traumatic cases. Preoperative VA of LP was a poor prognostic sign for visual outcomes.
Keywords
Temporary Keratoprosthesis (TKpro), Pars Plana Vitrectomy (PPV), Penetrating keratoplasty, Light Perception (LP), No Light Perception (NLP)
Introduction
A reasonably clear view through the cornea is necessary in order to optimize outcomes from vitreoretinal surgery. The use of a Temporary Keratoprosthesis (TKpro) can achieve this goal for patients with corneal opacification. The use of a TKpro was first described by Dr. Landers in 1981 [1]. There are two main types of TKpros in use today: The Eckardt and the Landers [2]. Prior to the use of a TKpro, other techniques such as open-sky vitrectomy, endoscopic-assisted vitrectomy or a preceding penetrating keratoplasty were utilized in patients with poor corneal clarity. Open-sky vitrectomy carries its own set of risks, such as increased risk of hypotony related complications. A TKpro provides a closed surgical environment as well as the ability to perform bimanual surgery with improved stereopsis in comparison with endoscopic-assisted vitrectomy [3]. A few studies have directly compared endoscopic-assisted vitrectomy with the use of temporary keratoprosthesis in vitreoretinal surgery [4,5]. These studies reported similar outcomes between the two groups. Ayyildiz and Durukan concluded that TKpro assisted vitrectomy should be performed instead of endoscopicassisted when extensive bimanual surgery is required during Pars-Plana Vitrectomy (PPV) with corneal opacification [6]. There have been several previous studies examining the outcomes and prognostic factors of combined penetrating keratoplasty, Temporary Keratoprosthesis and vitreoretinal surgery (TKpro/PPV/PKP). There is high variability in surgical and anatomical outcomes in the reported literature. Furthermore, there has been variability in the literature about variation in outcomes by indication, such as trauma or infection [7-9]. Postoperative complications reported include corneal graft failure, recurrent retinal detachment, hypotony and phthisis bulbi. The majority of the previous studies conclude that the combined procedure is a relatively safe surgical option for patients that need vitreoretinal surgery but have a limited view due to corneal opacification. Anatomical success, defined as re-attachment of the retina and corneal graft survival, occur in the majority of cases reported in the literature. However, improvement in Visual Acuity (VA) postoperatively at last examination is less frequent. Many of the patients undergoing this combined procedure have poor preoperative VA with a guarded visual prognosis [10-12].
Currently, there is limited data on outcomes of combined TKpro/PPV/PKP. More information and data concerning outcomes and associated prognostic factors may be useful in preoperative counselling and decision making. The purpose of the current study is to report the surgical and visual outcomes in a contemporary series as well as to report on prognostic factors of combined TKpro/PPV/PKP.
Materials and Methods
The current study is a retrospective consecutive case series of patients undergoing combined TKpro/PPV/PKP performed at the Bascom Palmer eye institute in Miami, FL, from January 1, 2013 to July 1, 2020. Institutional review board approval was obtained. The procedures followed were in accordance with the ethical standards of the Helsinki declaration of 1975, as revised in 2000. 2 patients were excluded because the follow-up visits were performed by an outside provider. Primary study outcomes were VA at last examination, rate of enucleation/ evisceration and presence of clear cornea at last exam. Other data points that were collected include: Indication for procedure, preoperative VA, preoperative Intraocular Pressure (IOP), tamponade used (if applicable), length of surgery, intraoperative and postoperative complications, rate of retinal reattachment, postoperative VA and IOP, additional procedures performed and graft rejection. Postoperative VA and IOP were recorded at postoperative day 1, week 1, month 1, month 3, year 1 and the last documented visit. Statistical analysis was performed to assess for correlation between prognostic factors and the following outcomes: Improvement in VA from preoperative, percentage of eyes with VA ≥ 5/200 and graft clarity at last exam. The prognostic factors assessed were: Preoperative VA, presence of infection, history of trauma, history of glaucoma, history of diabetes, presence of retinal detachment and surgery length [13-15]. Odds ratio was calculated for the aforementioned factors to assess for statistical relationship with outcomes. A Fisher two tailed statistical analysis was also used to calculate p-value between associated factors and outcomes. Statistical analysis was performed using online GraphPad© software. Statistical significance was set at p-value <0.05.
All surgeries were performed at the Bascom Palmer eye institute in Miami, FL. The following is a generalized description of the core surgical procedures performed. However, there were some minor variations from case to case. A standard vitrectomy setup was employed using 3 trochars. The donor corneal button was prepared using a disposable trephine. A trephine was then used to trephinate the host cornea. The host cornea was then removed. The TKpro was then sutured to the host cornea. The PPV was then performed using either 23-gauge or 25-gauge. Retinal detachment repair was then performed if indicated with tamponade of either C3F8 or silicone oil. For eyes where a Glaucoma Drainage Implant (GDI) was placed, a superior conjunctival flap was made and the implant was then sutured onto the globe. The tube was inserted into the pars plana. The TKpro was then removed. Sixteen 10-0 nylon sutures were then placed in a radial and interrupted fashion to secure the graft in place. The trochar cannula was removed and the sclerotomies were closed with gut suture [16].
Results
A total of 55 eyes (55 patients) were included in the current study. Mean age ± standard deviation (range) was 57.8 ± 21.7 years (7-89) and mean follow-up ± standard deviation (range) was 18 ± 16 months (0.5-78). 26 eyes (47.3%) had a follow up of at least one year at final examination. 13 eyes (23.6%) had a follow up of at least 2 years and 7 eyes (12.7%) had a follow up of at least 4 years at last examination. The most common indication for cornea transplant was failed cornea transplant (26 eyes, 47.3%). Table 1 for full list of indications for corneal transplantation. The most common indications for PPV were retinal detachment (29 eyes, 52.7%) and endophthalmitis (11 eyes, 20%). Table 2 for full list of indications for PPV.
| Indication | Number of eyes (%) |
|---|---|
| Failed corneal transplant | 27 (49.1%) |
| Primary graft failure | 14 (25.4%) |
| GDI | 9 (16.4%) |
| SO | 3 (5.5%) |
| Prior HSV infection | 1 (1.8%) |
| Post-surgical decompensation | 10 (18.2%) |
| Pseudophakic bullous keratopathy | 3 (5.5%) |
| Aphakic bullous keratopathy | 1 (1.8%) |
| Active infection | 8 (14.5%) |
| Corneal scarring | 7 (12.7%) |
| Prior ruptured globe | 5 (9.1%) |
| Silicone oil | 1 (1.8%) |
| Keratoprosthesis removal | 2 (3.6%) |
| Corneal blood staining | 1 (1.8%) |
Note: Table 1 shows the indications for corneal transplantation. GDI refers to failure of corneal graft in setting of glaucoma drainage implant device. Failed corneal transplant due to SO refers to failed grafts in the setting of intraocular silicone presence in the anterior chamber. HSV: Herpes Simplex Virus.
Table 1. Indications for corneal transplantation.
| Indication for PPV | Number of eyes (%) |
|---|---|
| Retinal detachment | 29 (52.7%) |
| Endophthalmitis | 11 (20.0%) |
| Glaucoma tube repositioning | 5 (9.1%) |
| Vitreous prolapse into anterior chamber | 4 (7.3%) |
| Vitreous hemorrhage | 2 (3.6%) |
| Retained lens fragments | 1 (1.8%) |
| Epiretinal membrane | 1 (1.8%) |
| Suprachoroidal hemorrhage | 1 (1.8%) |
| Silicone oil removal | 1 (1.8%) |
Note: Table 2 illustrates the different indications for pars plana vitrectomy and number of eyes. PPV: Pars Plana Vitrectomy.
Table 2. Indication for Pars Plana Vitrectomy (PPV).
10 eyes (18.2%) had indications that were related to trauma. 12 eyes (21.8%) had indications related to infection: 11 eyes had endophthalmitis and 1 eye had a corneal ulcer requiring therapeutic PKP with a retinal detachment. Table 3 for breakdown of suspected causes of endophthalmitis.
| Source | Number of eyes |
|---|---|
| Post-corneal transplant | 5 |
| Corneal ulcer | 4 |
| Post-cataract extraction | 1 |
| Post-intravitreal injection | 1 |
Note: Table 3 illustrates the suspected sources of endophthalmitis for the 11 eyes that had an indication of endophthalmitis for TKpro/PPV/PKP.
Table 3. Suspected sources of endophthalmitis.
Preoperatively, 7 eyes (12.7%) were phakic, 26 eyes (47.3%) were pseudophakic and 22 eyes (40%) were aphakic. 46 eyes (83.6%) had a history of prior intraocular surgery in that eye, including 18 eyes (32.7%) with a history of prior retinal detachment repair. 3 eyes (5.5%) were noted to have Proliferative Vitreoretinopathy (PVR) on exam preoperatively.
Preoperative VA ranged from LP to 20/200. Postoperative VA at last exam ranged from NLP to 20/30 (Figure 1). No intraoperative complications were noted. 14 eyes (25%) had VA at last exam of 20/200 or better. VA of NLP at last exam was noted in 5 eyes (9.1%). Figure 1 for range of postoperative VA. Phthisis bulbi was the final outcome for 2 eyes (3.6%) as determined by the treating physician. Enucleation was the final outcome for 1 eye (1.8%).
The retina was reattached intraoperatively in 24 out of 29 eyes with retinal detachments (82.7%), which were all diagnosed prior to surgery. The tamponades used during PPV were silicone oil (20 eyes, 57.1%), air (12 eyes, 34.3%) and C3F8 (2 eyes, 5.7%). Of the eyes with silicone oil tamponade, 1000 cs silicone oil was used in 18 eyes and 5000 cs silicone oil was used in 2 eyes. Three eyes had silicone oil exchanged during a subsequent procedure and 1 eye had silicone oil removed postoperatively. Silicone oil was noted to be in anterior chamber at final visit in one eye. Silicone oil was suspected to be present in the subretinal space in one eye at final visit.
At last examination, the corneal graft remained clear in 32 eyes (58.2%). The following postoperative complications were noted: Recurrent retinal detachment (6 eyes, 10.9%), hypotony (4 eyes, 7.3%), corneal graft rejection (1 eye, 1.8%) and suprachoroidal hemorrhage (1 eye, 1.82%). 11 eyes underwent additional surgery after the TKpro/PPV/PKP. 4 eyes underwent subsequent PPV for repair of retinal detachment in the postoperative period. The other 2 eyes that had retinal detachment postoperatively were not operated on due to poor visual potential. Insertion of Boston type I keratoprosthesis was performed in the eye that experienced graft rejection postoperatively. 2 eyes underwent insertion of GDI for uncontrolled IOP postoperatively. 1 eye underwent silicone oil removal and 1 eye underwent external drainage of choroidal hemorrhage postoperatively. 0 eyes underwent additional PKP. At last exam, the retina was attached in 22 out of 29 eyes (75.9%) with a history of retinal detachment. 1 eye (1.8%) was noted to have PVR postoperatively. Average time to NLP after surgery was 11.72 months ± 7.91 months (95% CI) for eyes with VA of NLP at last examination.
Preoperative VA of LP was associated with increased risk of NLP, enucleation or phthisis bulbi at last exam, which was statistically significant (OR=7.71, p=0.0219). Preoperative VA of count fingers or better trended towards improvement in VA at last examination although not statistically significant (OR=3.2, p=0.1056). History of trauma trended towards being a poor prognostic factor for improvement in VA at last exam although this was not statistically significant (OR=5.56, p=0.13). There was no correlation between time to trauma and percentage of eyes with VA of at least 5/200 at last exam (p=1.00). There was no difference in rate of clear graft at last examination between eyes with a history of trauma and those without a history of trauma (OR=1.10, p=1.00). Infectious related cases were less likely to have a clear cornea at last examination than non-infectious cases. Out of 12 eyes with indications related to infection only 2 had a clear cornea at last exam while out of 43 eyes without infection 30 eyes had a clear cornea at last exam (OR=0.087, p=0.0019). Table 4 for breakdown of number of eyes with clear cornea in infectious vs. non-infectious cases. There was no significant difference in percentage of eyes that had improvement in VA at last exam between infectious and non-infectious cases (p=0.508). There was also no difference in percentage of eyes with VA at last exam ≥ 5/200 between infectious and non-infectious cases (OR=1.65, p=0.477). Indication for PPV of glaucoma tube repositioning trended towards improvement in VA at last exam but this was not statistically significant (OR=7.33, p=0.072). Prior graft failure as an indication for surgery was associated with lack of improvement in VA at last exam which was statistically significant (OR=0.16, p=0.0027). A surgery time of greater than 2 hours was associated with improvement in VA at last exam from preoperative VA (OR=3.31, p=0.007). Table 5 for prognostic factors.
| Preop VA | Last exam: NLP/phthisis/enuc. (# of eyes) |
Other (# of eyes) |
Odds ratio | p value |
|---|---|---|---|---|
| LP | 5 | 12 | 7.71 | 0.022 |
| >= HM | 2 | 37 | ||
| Preop VA | VA at last exam improved from preop (# eyes) | VA at last exam did not improve from preop (# eyes) | Odds ratio | p-value |
| LP | 9 | 8 | 2.16 | 0.24 |
| HM or better | 13 | 25 | ||
| Worse than CF | 14 | 28 | 0.31 | 0.11 |
| CF or better | 8 | 5 | ||
| Indication for surgery | VA at last exam improved from preop (# of eyes) | VA at last exam did not improve from preop (# eyes) | Odds ratio | p-value |
| Infection | 6 | 5 | 2.10 | 0.32 |
| No infection | 16 | 28 | ||
| Trauma | 1 | 7 | 0.18 | 0.13 |
| No trauma | 21 | 26 | ||
| Infection or trauma | 7 | 12 | 0.82 | 0.78 |
| No infection/trauma | 15 | 21 | ||
| Indication for PPV | VA at last exam improved from preop (# of eyes) | VA at last exam did not improve from preop (# eyes) | Odds ratio | p-value |
| Retinal detachment | 8 | 18 | 0.51 | 0.28 |
| No retinal detachment | 14 | 16 | ||
| GDI repositioning | 4 | 1 | 7.33 | 0.07 |
| No GDI repositioning | 18 | 33 | ||
| Surgery length | VA at last exam improved from preop (# of eyes) | VA at last exam did not improve from preop (# eyes) |
Odds ratio | p-value |
| Surgery <= 2 hr | 2 | 15 | 0.12 | 0.01 |
| Surgery >2 hr | 20 | 18 | ||
| Indication for surgery | Last VA: 5/200< (# eyes) | Last VA: ≥ 5/200 (# eyes) | Odds ratio | p value |
| Infection | 8 | 4 | 1.65 | 0.4768 |
| Non-infection | 33 | 10 | ||
| Indication for surgery | Last exam: K graft clear (# eyes) |
Last exam: K graft not clear (# eyes) | Odds ratio | p value |
| Trauma | 6 | 4 | 1.10 | 1 |
| No trauma | 26 | 19 | ||
| Infection | 2 | 10 | 0.09 | 0.0019 |
| No infection | 30 | 13 | ||
| Time trauma surgery | Last VA: >= 5/200 | Last VA: <5/200 | Odds ratio | p value |
| <1 mo | 1 | 1 | 3.00 | 1 |
| >= 1 mo | 2 | 6 | ||
Note: Table 4 summarizes VA outcomes and associated factors of patients undergoing combined TKpro/PPV/PKP. Odds ratio and p-values were calculated to assess for association of improvement in VA at last exam, corneal graft clarity at last exam and percentage of eyes with at least 5/200 VA at last exam with the following factors: Preoperative VA, indication for surgery, indication for PPV, and surgery length. Odds ratio and p-values were calculated to assess for association of improvement in VA at last exam with the following factors: Preoperative VA, indication for surgery, indication for PPV and surgery length. P-value was calculated using Fisher two tailed analysis. VA: Visual Acuity; NLP: No Light Perception; Enuc: Enucleation, K graft refers to corneal graft. PPV: Pars Plana Vitrectomy.
Table 4. Outcomes and associated factors.
| Study | # eyes | Infection (# of eyes) |
Mean f/u | Last VA range | % >= 5/200 (last exam) |
Graft clear (last exam) |
Retina attached Intraop. |
|---|---|---|---|---|---|---|---|
| Roters, et al. | 34 | 0 | 30 mo | 20/500 to NLP | 0% | 65% | 94% |
| Khouri, et al. | 24 | 1 | 3 year | 20/100 to NLP | 8.30% | 79% | 92% |
| Lee, et al. | 11 | 6 | 1.8 year | 20/25 to NLP | 9% | 27% | 81% |
| Nowomiejska, et al. | 12 | 0 | 1 year | CF to NLP | 0% | 25% | 92% |
| Karpan, et al. | 20 | 0 | 18 mo | 20/20 to NLP | 65% | 40% | 90% |
| Alvarez, et al. | 100 | 9 | 2 year | N/A | n/a | 49% | 84% |
| Current study | 55 | 12 | 16 mo | NLP to 20/30 | 25% | 55% | 83% |
Note: Table 5 summarizes the findings of the previous studies on outcomes of combined TKpro/PPV/PKP. This table only includes studies with more than 10 eyes and studies that were performed during the last two decades. Last VA range shows the range of postoperative VA at last follow up. %>= 5/200 shows the percentage of eyes that had VA at last exam of 5/200 or better. Graft clear shows the percentage of eyes with a clear corneal graft noted on last exam. Retina attached shows the percentage of eyes where the retina was able to be reattached intraoperatively for eyes with retinal detachment.
Table 5. Summary of previous studies on outcomes of combined TKpro/PPV/PKP.
Discussion
Limited data is currently available regarding outcomes and prognostic factors of combined TKpro/PPV/PKP with relatively small sample sizes. Table 5 summarizes the previous literature regarding outcomes of this combined procedure. The current study of 55 eyes is a larger sample size than many of the previous studies. The current study also had a relatively longer mean follow up in comparison with previous studies. The current study had an average follow up of 16 months and 13% of eyes with follow up ≥ 4 years at final examination.
Previous studies have reported a wide range in visual outcomes. For instance, previous studies have reported a rate of improvement in VA at last exam from preoperatively ranging from 40%-84% of eyes [17]. The current study reports that 32.7% of eyes had improvement in VA at last examination from preoperative. One possibility for this discrepancy is that the current study included all indications for the combined procedure, including severe infections and trauma. The current study was also performed at a large, tertiary referral center. 46 out of 55 eyes (83.6%) had a history of prior ocular surgery.
In the current study, there was no significant variation in visual outcomes with regard to indication of surgery. There was no significant difference in visual outcomes between infectious and non-infectious cases. There was also no significant difference in rates of improvement in VA postoperatively between eyes with a retinal detachment and those without retinal detachment. This supports the notion that the combined procedure can be used for a variety of indications. There were some trends in visual outcomes by indication. Eyes without a history of trauma trended towards having higher rates of improvement in VA at last exam from preoperative although this was not statistically significant (p=0.13). The indication for PPV of GDI repositioning trended towards an association with improvement in VA (p=0.07). The PPV was performed solely for GDI positioning into the pars plana in 5 of 8 eyes where a GDI was placed into the pars plana. 3 of the 8 eyes also had co-existing retinal pathology for which the PPV was indicated: 1 retinal detachment, 1 vitreous prolapse into the anterior chamber and 1 epiretinal membrane. The majority of these 8 eyes have a much better preoperative visual prognosis and have better visual potential with less retinal pathology in comparison with other eyes that required PPV for vitreoretinal diseases such as endophthalmitis. Although the majority of eyes did not show an improvement in VA at last examination from preoperative, a significant percentage of eyes did have functional vision at last exam. 25% of eyes had a VA at last exam of at least 20/200. Previous studies have reported a final outcome of phthisis bulbi ranging from 13% to 22% of eyes and VA of NLP ranging from 4%-15%. In the current study, phthisis bulbi was noted 3.6% of eyes and 9% of eyes had a VA of NLP at last examination. These outcomes are important in preoperative counselling of patients undergoing this combined procedure. In the current study, almost 10% of eyes had VA of NLP at last exam. In some cases, the combined TKPro/PPV/PKP may serve the role of a globe salvage procedure rather than visual rehabilitation. Setting realistic expectations for the patient preoperatively is paramount [18].
Previous studies report a rate of graft failure postoperatively ranging from 21%-80%. In the current study, corneal grafts remained clear at final examination in 58.2% of eyes. There was no significant difference in rate of corneal graft clarity at last exam between eyes with an indication related to trauma and those without a history of trauma; however, infectious related cases were less likely to have a clear cornea at last examination than non-infectious cases (p=0.0019).
Retina outcomes in the current study were also similar to what has been previously reported in the literature. Previous studies have reported a rate of retinal reattachment from 84% to 94%. The current study reports a rate of retinal reattachment intraoperatively of 83%.
Both the current study and the previous literature support that TKpro/PPV/PKP is associated with relatively low intraoperative complication rates, which are similar to that of other complex eye surgeries. The rate of postoperative complications in the current study was comparable to the rates of complication of endoscopic assisted vitrectomy reported by Ayyildiz, et al. Suprachoroidal hemorrhage was noted in 1 eye postoperatively in the current study. We report a rate of postoperative retinal detachment after the combined procedure to be approximately 10%. Previous studies in the literature have reported a rate of retinal detachment postoperatively ranging from 10% to 38%. The authors conclude that the combined TKpro/PPV/PKP is a relatively safe procedure with complication rates similar to other complex eye surgeries.
Few studies have reported statistically significant prognostic factors associated withoutcomes of combined TKpro/PPV/ PKP. In the current study, prior graft failure as an indication for surgery was associated with lack of improvement in VA at last exam from preoperative, which was statistically significant (OR=0.16, p=0.0027). In the current study, preoperative VA of LP was associated with poor visual outcomes which was statistically significant (p=0.0219). This finding is likely due to the fact that patients with worse preoperative VA are more likely to have a more advanced disease state. In the current study length of surgery greater than 2 hours was associated with improvement in VA at last exam from preoperative (p=0.0065). One possible contributing factor for this finding is that all surgeries involving GDI repositioning were greater than 2 hours. Another possible explanation is that some of the retinal detachments were deemed inoperable during the surgery which may have led to shorter surgery times.
A variety of ocular pathology and indications for surgery were included in the current study. This is likely contributing to the fact that many of the factors assessed did not show statistically significant association with outcomes. This study is also limited by being performed at a single tertiary referral center with many different surgeons, including surgeons in training performing minor steps of the surgery. Although this sample size of 55 eyes is larger than many of the previous studies, it is still a relatively small sample size. Another limitation is that the VA was not measured in a uniform, standardized fashion. Lastly, the variation in follow up is a limitation of this study. The current study had a relatively longer mean follow up time in comparison with previous studies that investigated outcomes at 6 months and 1 year postoperatively; however, two eyes included in this study had less than one month of follow up at final visit.
Conclusion
In summary, combined TKPro/PPV/PKP can be performed in patients with corneal opacification while allowing for bimanual vitreoretinal surgery. In the current study, preoperative VA of LP was associated with poor visual outcomes. Visual outcomes were similar between infectious and non-infectious cases although corneal graft clarity at last exam was lower in the infectious group. Visual outcomes and corneal graft clarity were similar between traumatic and non-traumatic cases. Combined TKpro/PPV/PKP can be performed for a variety of indications and is associated with relatively low rates of complications in the current study.
Acknowledgement
The authors would like to thank and acknowledge the work and life of Dr. Maurice B. Landers III, MD, who passed away on July 11, 2021. He was a pioneer in the field of vitreoretinal surgery. His accomplishments and contributions to the field are numerous. His pioneering work with the temporary keratoprosthesis is included in his lengthy list of accomplishments and has helped further the field of vitreoretinal surgery.
References
- Landers MB, Foulks GN, Landers DM, et al. Temporary keratoprosthesis for use during pars plana vitrectomy. Am J Ophthalmol. 1981;91(5):615-9.
[Crossref] [Google Scholar] [PubMed]
- Prakhunhungsit S, Yannuzzi NA, Berrocal AM. Vitrectomy using the Eckardt temporary keratoprosthesis. Am J Ophthalmol Case Rep. 2020;19:100709.
[Crossref] [Google Scholar] [PubMed]
- Kapran Z, Ozkaya A, Erdogan G, et al. Wide field landers keratoprothesis in various combined corneal and vitreoretinal problems: Twelve month results. Ophthalmic Surg Lasers Imaging Retina. 2017;48(3):237-41.
[Crossref] [Google Scholar] [PubMed]
- Ayyildiz O, Hakan Durukan A. Comparison of endoscopic-assisted and temporary keratoprosthesis-assisted vitrectomy in combat ocular trauma: experience at a tertiary eye center in Turkey. J Int Med Res. 2018;46(7):2708-16.
[Crossref] [Google Scholar] [PubMed]
- Chun DW, Colyer MH, Wroblewski KJ. Visual and anatomic outcomes of vitrectomy with temporary keratoprosthesis or endoscopy in ocular trauma with opaque cornea. Ophthalmic Surg Lasers Imaging. 2012;43(4):302-10.
[Crossref] [Google Scholar] [PubMed]
- Nowomiejska K, Haszcz D. Wide field landers temporary keratoprosthesis in severe ocular trauma: Functional and anatomical results after one year. J Ophthalmol. 2015;2015:163675.
[Crossref] [Google Scholar] [PubMed]
- Khouri AS, Vaccaro A, Zarbin MA, et al. Clinical results with the use of a temporary keratoprosthesis in combined penetrating keratoplasty and vitreoretinal surgery. Eur J Ophthalmol 2010;20(5):885-91.
[Crossref] [Google Scholar] [PubMed]
- Bove Alvarez M, ArumI CG, DistEfano L, et al. Comparative study of penetrating keratoplasty and vitreoretinal surgery with Eckardt temporary keratoprosthesis in ocular trauma versus non-trauma patients. Graefes Arch Clin Exp Ophthalmol. 2019;257(11):2547-58.
[Crossref] [Google Scholar] [PubMed]
- Mayali H, Kayıkcloglu O, Altinısik M, et al. Clinical results in patients with combined penetrating keratoplasty and vitreoretinal surgery using landers wide field temporary keratoprosthesis. Turk J Ophthalmol. 2019;49(5):270-6.
[Crossref] [Google Scholar] [PubMed]
- Lee DS, Heo JW, Choi HJ, et al. Combined corneal allotransplantation and vitreoretinal surgery using an Eckardt temporary keratoprosthesis: Analysis for factors determining corneal allograft survival. Clin Ophthalmol. 2014;8:449-54.
[Crossref] [Google Scholar] [PubMed]
- Chen HJ, Wang CG, Dou HL, et al. Anatomical outcome of vitreoretinal surgery using temporary keratoprosthesis and replacement of the trephined corneal button for severe open globe injuries: One year result. J Ophthalmol. 2014;2014:794039.
[Crossref] [Google Scholar] [PubMed]
- Gelender H, Vaiser A, Snyder WB, et al. Temporary keratoprosthesis for combined penetrating keratoplasty, pars plana vitrectomy and repair of retinal detachment. Ophthalmology. 1988;95(7):897-901.
[Crossref] [Google Scholar] [PubMed]
- Roters S, Szurman P, Hermes S, et al. Outcome of combined penetrating keratoplasty with vitreoretinal surgery for management of severe ocular injuries. Retina. 2003;23(1):48-56.
[Crossref] [Google Scholar] [PubMed]
- Schepens CL. Clinical and research aspects of subtotal open-sky vitrectomy. XXXVII Edward Jackson memorial lecture. Am J Ophthalmol 1981;91(2):143-71.
[Crossref] [Google Scholar] [PubMed]
- Garcia-Valenzuela E, Blair NP, Shapiro MJ, et al. Outcome of vitreoretinal surgery and penetrating keratoplasty using temporary keratoprosthesis. Retina. 1999;19(5):424-9.
[Crossref] [Google Scholar] [PubMed]
- Yan H, Cui J, Zhang J, et al. Penetrating keratoplasty combined with vitreoretinal surgery for severe ocular injury with blood stained cornea and no light perception. Ophthalmologica. 2006;220(3):186-9.
[Crossref] [Google Scholar] [PubMed]
- Dong X, Wang W, Xie L, et al. Long term outcome of combined penetrating keratoplasty and vitreoretinal surgery using temporary keratoprosthesis. Eye. 2006;20(1):59-63.
[Crossref] [Google Scholar] [PubMed]
- Omari A, Khan N, Tausif H, et al. Temporary keratoprosthesis with penetrating keratoplasty in conjunction with pars plana vitrectomy for repair of retinal detachments in patients with anterior and posterior segment pathology. Retin Cases Brief Rep. 2023; 17(2):176-80.
[Crossref] [Google Scholar] [PubMed]