Research Article - Journal of Clinical Ophthalmology (2018) Volume 2, Issue 2
Retropupillary iris claw intraocular lens implantation in penetrating keratoplasty patients.
Reshma Raj*, Vasanthi Kotian and Vijay Pai
Department of K.S. Hegde Charitable Hospital, Nithyanandanagar, Derlaketta, Mangalore, India
- *Corresponding Author:
- Reshma Raj
KS Hegde Medical Academy Thaliparamba, Kannur Kerala, India
E-mail: dr.reshraj@gmail.com
Tel: 00919995622881
Accepted date: October 03, 2018
Citation: Raj R, Kotian V, Pai V. Retropupillary iris claw intraocular lens implantation in penetrating keratoplasty patients. J Clin Ophthalmol 2018;2(2):92-95.
DOI: 10.35841/clinical-ophthalmology.2.2.92-95
Visit for more related articles at Journal of Clinical OphthalmologyAbstract
Objective-To evaluate the visual outcome and assess the complication rate after implantation of a retropupillary iris-claw Intraocular Lens (IOL) during Penetrating Keratoplasty (PKP). Method-A descriptive study on 15 eyes of 15 patients underwent penetrating keratoplasty along with retropupillary iris claw intraocular lens implantation. Reasons for penetrating keratoplasty included pseudophakic bullous keratopathy, aphakic bullous keratopathy, and leukomatous corneal opacity. Mean follow up was 3 months for Visual Acuity (VA), Intraocular Pressure (IOP), graft clarity and any complications. RESULT-Of 15 eyes, visual acuity improvement was seen in 11 (74%) eyes and remained unchanged in 4 (26%) eyes. Post operatively elevated IOP was seen in 8 (53%) eyes, which was managed medically. Improvement in graft clarity was noted in 7 (46%) eyes 1 week following the surgery. Conclusion-The results demonstrate that penetrating keratoplasty combined with retropupillary Iris claw lens is an easy and effective method for the correction of aphakia in patients with no capsule support.
Keywords
Penetrating keratoplasty, Intraocular lens, Aphakia, Keratopathy
Introduction
The iris claw IOL attached to the anterior iris was developed by Worst in 1972 [1]. He has provided a technique to correct aphakia in the absence of capsular support and without direct angle compromise. However, significant complication is damage to endothelium [2], particularly in patients with narrow anterior chambers and in corneal transplantation. The technique was modifies by Brasse and Neuhann [3] by clipping the lens to the posterior iris, thereby protecting the endothelium, with the A contant altered accordingly to 117.0 [4].
Intraocular lens implantation in eyes with pseudophakic or aphakic corneal edema and insufficient posterior capsular support is a surgical challenge [4]. The iris claw lens is fixated to the iris without sutures which is a faster procedure when compared to scleral fixating lens in combined penetrating keratoplasty [4,5]. The iris claw lens has the advantage that it can be fixated to the iris without sutures because the peripheral iris is incarcerated between the claws. Since an implantation of iris claw lenses only takes a few minutes, the hypotonic open sky phase can be shortened compared to combined surgery with the scleral fixation technique in cases of combined penetrating keratoplasty [5,6].
The purpose of this study is to evaluate the visual outcome and assess the complication rate after implantation of a retropupillary iris-claw Intraocular Lens (IOL) during Penetrating Keratoplasty (PKP).
Method
This study was conducted during July 2016 to July 2017 at K. S. Hegde Hospital, Mangalore. Our study included 15 eyes of 15 patients and all patients were operated by a single surgeon. Patients included were pseudophakic bullous keratopathy due to Anterior Chamber Intraocular Lens (ACIOL), aphakic bullous keratopathy, leucomatous corneal opacity with lack of posterior capsular support.
Patients underwent the following combined procedures:
1. Penetrating keratoplasty.
2. Anterior vitrectomy-if required.
3. Release of PAS- if needed.
4. PMMA iris claw lens fixation before graft suturing.
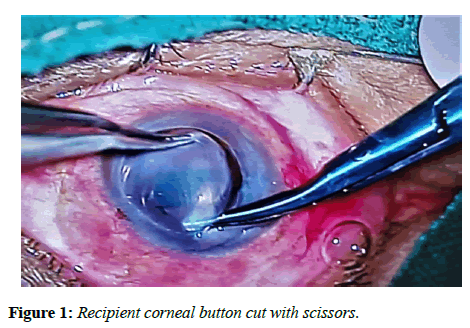
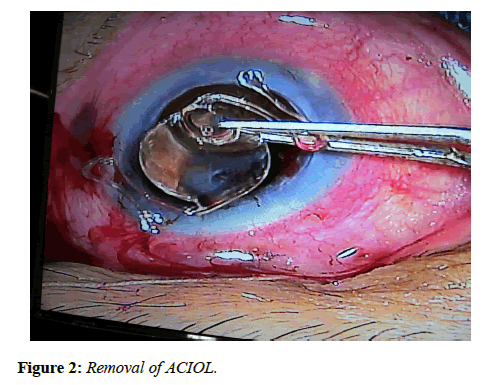
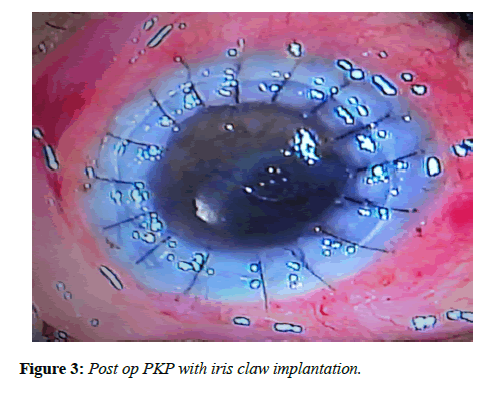
All patients underwent corneal trephination with trephine. After making side ports, the recipient corneal button was cut out with scissors (Figure 1). Removal of angle supported IOL implanted previously (Figure 2) was followed by anterior vitrectomy for few cases. The retropupillary iris claw lens was then enclaved with convex side down by an open sky approach on the mid peripheral iris. The donor’s corneal button was then sutured to recipient bed with 10-0 nylon sutures. Post-operatively, patients were examined on the 1st , 7th, and 30th post-operative days, and then 3 months in the follow-up period (Figure 3). Best Corrected Visual Acuity (BCVA) and Intraocular Pressure (IOP) were noted and compared to preoperative data. The graft clarity was assessed by slit-lamp examination.
Study design
This is a cross-sectional, non-interventional, descriptive and hospital based study. The collected information is summarized by using frequency and percentage.
Statistical analysis
The results were statistically analysed. Statistical analysis was performed on SPSS version 17.0 for Windows. Descriptive statistics such as frequency and percentage for qualitative data and mean with standard deviation for quantitative data were used.
Results
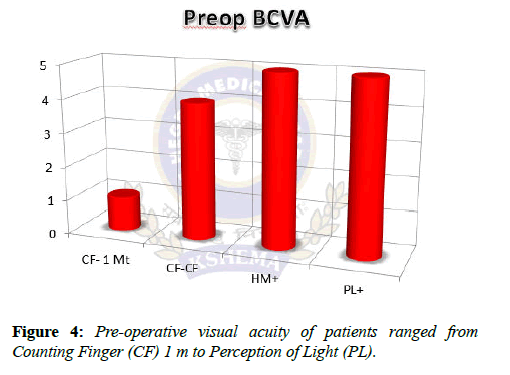
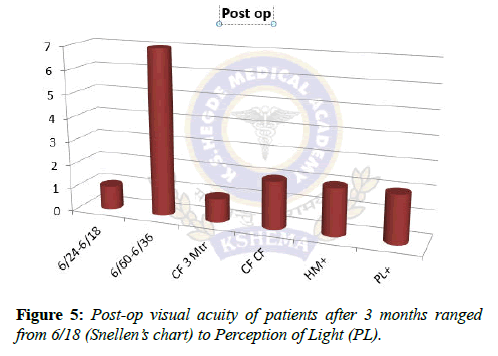
The mean age of patients was 55.3 (range of 45 to 65 yrs.) 80% of patients were males and 20% females. Of 15 patients, 8 were diagnosed with pseudophakic bullous keratopathy, 4 with aphakic bullous keratopathy and 3 with leukomatous corneal opacity. Pre-op Visual acuity (Figure 4) in our study ranged from perception of light to counting finger 1 m. Post-op visual acuity (Figure 5) ranged from perception of light to 6/18.
Regarding IOP, 75% of aphakic bullous keratopathy had raised IOP, when compared with 50% of PBK and 30% of leucomatous corneal opacities (Table 1).
| IOP | PBK | ABK | LEUCO OPACITY |
|---|---|---|---|
| <21 mmHg | 4 | 1 | 2 |
| 22-30 mmHg | 4 | 3 | 1 |
Table 1: Intraocular pressure range.
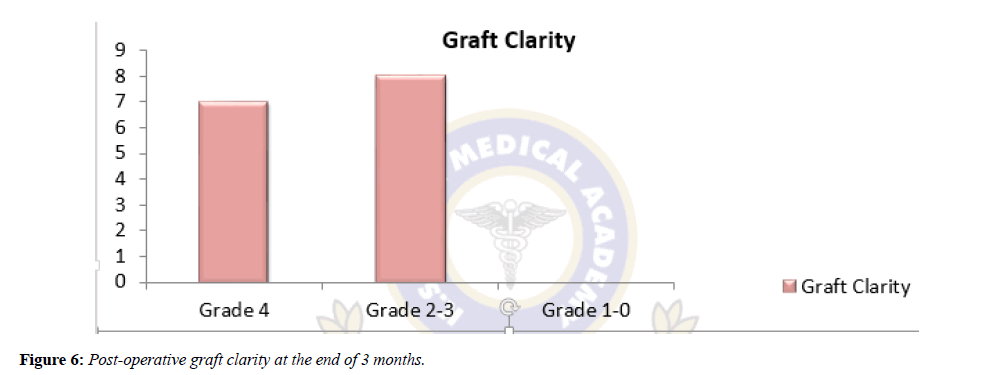
Graft clarity (Figure 6 & Table 2) [7] was also assessed at the end of 3 months. In this 46.6% of patients had grade 4 graft clarity.
| Graft Clarity | Impression |
|---|---|
| Grade 4 | Optically clear with excellent view of iris details. |
| Grades 2-3 | Mid to corneal significant corneal haze with or without good view of iris details. |
| Grade 0 | Opaque grafts with poor view of iris and anterior segment details. |
Table 2: Grading of Graft clarity.
Discussion
Secondary IOL implantation in the absence of adequate posterior capsular support is a challenge. The modern ACIOLs with flexible haptics, though technically easier to place and easily available, can lead to significant complications including angle trauma with hyphaema, clefts, secondary glaucoma, uveitis and corneal endothelial decompansation from progressive endothelial trauma. This is important in case of a corneal graft where corneal endothelium is already compromised and there is a risk of graft rejection. In a study conducted by Marques et al. [8] ACIOL related inflammation has been the main indication for IOL exchange in more than 50% of cases. In our study, at the end of 3 months, visual acuity improvement was seen in 11 (74%) eyes and remained unchanged in 4 (26%) eyes. This was in accordance with the study done by Rufer et al. [9]. However combined surgery limited the refractive results with the unpredictable mire changes, which are likely postoperatively. The causes of poor vision were cystoid macular odema and macular scar noted in 2 cases each. Elevated IOP was observed in 8 cases. Similarly, raised IOP was found in 1 out of 31 patients by Schallenberg et al. [10]. In another study done by Jare et al. [11] 3 out of 108 eyes had raised IOP in the first week postoperatively which were managed with Nd: YAG peripheral iridectomy. Intraocular lens was stable and no significant decentrations were noted. One eye presented with hyphema in the first postoperative week, which was cleared without further treatment.
Conclusion
In our study, we found that there was a definite improvement in visual acuity and a decreased complication rate in this combined procedure. Thus, retropupillary iris claw lens implantation combined with penetrating keratoplasty is a simple and safe alternative to achieve pseudophakia in eyes with corneal edema and inadequate posterior capsular support.
Limitations
Although this study showed that retropupillary Iris claw lens is better alternative, it was limited by its modest sample size. Thus, studies with larger sample size should be conducted in the future to validate our findings. Another limitation was shorter duration in post-operative evaluation; atleast 1 year of assessment would be required to validate the study. Comparison study can also be done with regard to scleral fixation lens, as it is another alternative to treat aphakia.
Ethical Clearance
An Informed Consent was taken from all the participants. The Ethical Clearance was obtained from Institutional Ethics Committee, K. S. Hegde Medical Academy.
References
- Worst JG. Iris claw lens. J Am Intraocul Implant Soc 1980;6:166-7.
- Menezo JL, Cisneros AL, Rodriguez-Salvodar V. Endothelial study of iris claw phakic lens: Four year follow-up. J Cataract Refract Surg. 1998;24:1039-49.
- Brasse K, Neuhann TH. Posterior chamber verisyse lens implantation to correct aphakia without capsular support. Video J Cataract Refract Surg. 2004;20.
- Rijneveld WJ, Beekhuis WH, Hassman EF, et al. Iris claw lens: Anterior and posterior iris surface fixation in the absence of capsular support during penetrating keratoplasty. J Refract Corneal Surg. 1994;10:14-9.
- Rüfer F, Saeger M, Nölle B, et al. Implantation of retropupillar iris claw lenses with and without combined penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol. 2009;247:457-62.
- Kanellopoulos AJ. Penetrating keratoplasty and artisan iris-fixated intraocular lens implantation in the management of aphakic bullous keratopathy. Cornea. 2004;23:220-4.
- Shanbhag N, Cholera PP, Sahana N, et al. evaluation of graft clarity post-penetrating keratoplasty. Int J Sci Study. 2017;5:90-6.
- Faria M, Pinto FN, Medeiros PJ, et al. Retropupillary iris claw intraocular lens implantation in aphakia for dislocated intraocular lens (Corrigendum). Int Med Case Rep J. 2016;9:261-5.
- Rüfer F, Saeger M, Nölle B, et al. Implantation of retropupillar iris claw lenses with and without combined penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol. 2008;247:457-62.
- Schallenberg M, Dekowski D, Hahn A, et al. Aphakia correction with retropupillary fixated iris-claw lens (Artisan) long-term results. Clin Ophthalmol. 2014;8:137-41.
- Jare NM, Kesari AG, Gadkari SS, et al. The posterior iris-claw lens outcome study: 6-month follow-up. Indian J Ophthalmol 2016;64:878-8.