Original Article - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 4
Refractive and visual outcomes of two different aspheric monofocal intraocular lenses with differing tinting and spherical aberration values
Hung-Yuan Lin1,2,3, Ya-Jung Chuang4*, Ting-Yu Lin5, Pi-Jung Lin6
1 Universal Eye Center, Zhong-Li, Taiwan, Republic of China
2 Department of Optometry, Central Taiwan University of Science and Technology, Taichung City, Taiwan, Republic ofChina
3 Ophthalmology Department Shanghai Ruidong Hospital, Shanghai, China
4 Universal Eye Center, Long-Tan, Taiwan, Republic of China
5 Department of Chemistry, Barnard College, Columbia University, New York, USA
6 Universal Eye Center, Taipei, Taiwan, Republic of China
- Corresponding Author:
- Dr. Ya-Jung Chuang
Universal Eye Center
Long-Tan
Taiwan
Republic of China
E-mail: rannyposh@gmail.com
Accepted date: April 7, 2020
Citation: Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.
Abstract
Purpose: To compare refractive and visual outcomes of two diffractive monofocal intraocular lenses (IOLs) with different tinting and spherical aberration values.
Study design: Retrospective case series.
Methods: The right eye of consecutive patients who had undergone bilateral implantation of SZ-1 (NIDEK Co. Ltd., Gamagori, Japan) or ZCB00 (Johnson and Johnson Inc. New Brunswick, NJ, USA) IOLs was evaluated. Refractive outcomes, changes in visual acuity, ocular spherical aberration, and changes in photopic and mesopic contrast sensitivity were analyzed.
Results: Thirty-three eyes received the SZ-1 IOL (SZ-1 group, while 29 eyes received the ZCB00 IOL (ZCB00 group). The mean preoperative manifest refraction spherical equivalent (MRSE) was −1.48 ± 4.74 D and −0.34 ± 1.50 in the SZ-1 group and ZCB00 group, respectively. At 3 months, the mean MRSE was −0.87 ± 1.08 D and −0.65 ± 0.76, respectively (p=0.25). At 3 months postoperatively, the mean best spectacle-corrected visual acuity was 0.14 ± 0.20 LogMAR and 0.11 ± 0.17 LogMAR, respectively (p=0.67). At the same time point, ocular spherical aberration was statistically significantly different (0.01 ± 0.23 μm vs. −0.51 ± 0.51 μm, respectively; p<0.0001).
Postoperatively, the mean photopic and scotopic contrast sensitivity did not differ between the groups (p=0.57).
Conclusion: Postoperative refractive outcomes and visual acuity following the implantation of these aspheric IOLs were similar. The different asphericity and yellow tinting of the SZ-1 IOL did not affect postoperative visual performance.
Keywords
Intraocular lenses, Aspheric monofocal, Visual outcomes.
Introduction
Advances in biomaterials and optical engineering have led to the introduction of foldable, aspheric Intraocular Lenses (IOLs) [1]. These IOLs have resulted in improved visual quality compared with older generation spherical IOLs [2]. The optical designs of monofocal aspheric IOLs are continually being refined to improve functional vision postoperatively. In general, a higher spherical aberration decreases the Strehl ratio resulting in lower optical quality [3]. Additionally, IOLs produced by different manufacturers are composed of varying materials that affect light transmittance and, potentially, visual function. In general, different aspheric IOLs are used when post refractive visual performance is unaffected because aspheric IOL designs are based on homogreneous refractive materials [4].
The availability of numerous IOLs means that many do not undergo extensive clinical investigation after marketing approval, with peer-reviewed publications being limited to the most commonly used IOLs. Hence, there are limited data available to surgeons for the selection of the most appropriate IOLs. In the current study, we compared the refractive and functional visual outcomes of two different aspheric monofocal acrylic IOLs with differing tinting and spherical aberration values.
Materials and Methods
This retrospective comparative study evaluated consecutive patients with senile cataract who underwent bilateral implantation of the SZ-1 (NIDEK Co. Ltd., Gamagori, Japan) or ZCB00 (Johnson and Johnson Inc. New Brunswick, NJ, USA) IOL. Patients with anterior segment disease, high or special ametropia, corneal irregular astigmatism, and pterygium were excluded from this study. As all examination devices were based on eye gaze, we further excluded individuals with severe refractive medium opacity, macular degeneration, retinal diseases, nystagmus, and poor cooperation, which can affect measurement accuracy. Data sets were excluded if data for any of the parameters were not available. The right eye of each patient was selected for inclusion in the study. All the patients had undergone surgery from January 2017 to October 2017, and brand of IOLs select at random from a list of all who had surgery. The institutional review board of Antai Tian-Sheng Memorial Hospital, Taiwan, Republic of China approved the present study (18-085-B), and the informed consent was obtained from all participants.
Table 1 presents the characteristics of both IOLs. Sixty-two eyes of 62 patients underwent IOL implantation. Thirty-three eyes of 33 patients received the SZ-1 IOL (SZ-1 group), while 29 eyes of 29 patients received the ZCB00 IOL (ZCB00 group). All the patients included in the study had senile cataract, with spherical manifest refractive error ranging from +4.25 to −17.50 D and astigmatism up to −2.25 D. Patients were excluded if they had undergone previous ocular surgery, had a history of trauma, ocular disease other than cataract, zonular weakness or were receiving medications that may affect vision.
| Characteristic | SZ-1 | ZCB00 |
|---|---|---|
| Material | Yellow-tinted hydrophobic soft acrylic | Ultraviolet (UV) blocking hydrophobic acrylic |
| Optic design | Biconvex, anterior aspheric surface, square optic edge | Biconvex, anterior aspheric surface, square optic edge |
| Optic diameter | 6.0 mm | 6.0 mm |
| Haptic material | Yellow-tinted hydrophobic soft acrylic | UV-blocking hydrophobic acrylic |
| Target residual ocular spherical aberration | 0.1 μm | 0 μm |
Table 1. Characteristics of the two aspheric hydrophobic intraocular lenses.
Preoperative ophthalmic examination included measurement of distance uncorrected visual acuity (UCVA; LogMAR), manifest refraction, best spectacle-corrected visual acuity (BCVA; LogMAR), slit-lamp examination, corneal topography and aberrometry (6-mm pupil) using the OPD-Scan III (NIDEK Co. Ltd., Gamagori, Japan), keratometry and pupillometry using the OPD-Scan III, optical biometry (AL-Scan; NIDEK Co. Ltd., Gamagori, Japan), contrast sensitivity under photopic and scotopic conditions (CGT-2000; Takagi Seiko Co., Ltd., Nagano-ken, Japan), and dilated fundus examination. Postoperative follow-up visits were performed at 1 day, 1 month, and 3 months. These measurements (with the exception of dilated funduscopy unless warranted) were also performed at the 1-month and 3-month visits. Total ocular (not corneal) spherical aberration measurements are reported for a 6 mm pupil to the 6th Zernike order. The area under log contrast sensitivity function (AULCSF) was calculated for both groups.
An experienced surgeon (HYL) performed all the cataract surgeries under local anesthesia. A self-sealing 2.2 mm temporal incision was performed followed by injection of viscoelastic, capsulorhexis, phacoemulsification, irrigation/aspiration, and injection of viscoelastic into the capsular bag. The IOL was implanted into the capsular bag followed by aspiration of the viscoelastic. The User Group for Laser Interference Biometryoptimized IOL constants was used to determine the power of each IOL. In cases with an axial length <21.5 mm, the Hoffer Q formula was used. In eyes with an axial length ≥ 21.5 mm, the SRK/T formula was used. The personalized anterior chamber depth and constants were obtained from the User Group for Laser Interference Biometry website (http://ocusoft.de/scripts2/ ciolc.php). The constants were optimized for the AL-Scan. An A constant of 119.6 was used for all the calculations. In the SZ-1 group, three eyes were targeted for postoperative myopia (−2.00 D, −2.50 D, and −3.00 D), while the remaining eyes were targeted for postoperative emmetropia. In the ZCB00 group, two eyes were targeted for −2.00 D of myopia (−2.00 D each), while the remaining eyes were targeted for postoperative emmetropia.
Refractive outcomes, changes in visual acuity, changes in ocular spherical aberration, and changes in photopic and mesopic contrast sensitivity were analyzed. The Student’s t test was used to compare mean values and the Wilcoxon rank-sum test was used to compare medians. The 95% Confidence Intervals (CI) is presented as appropriate. A p<0.05 denoted statistical significance. Data for 1 day, 1 month, and 3 months after IOL implantation for the treatment of cataract are presented.
Results and Observations
Preoperatively, the mean manifest refraction spherical equivalent (MRSE) in the SZ-1 group was −1.48 ± 4.74 D, the mean sphere was −0.92 ± 4.29 D, and the mean cylinder was −0.98 ± 0.52 D. In the ZCB00 group, these values were −0.34 ± 1.50 D, 0.21 ± 1.52 D, and −0.97 ± 0.60 D, respectively.
The mean age of patients in the SZ-1 and ZCB00 groups was 66.75 ± 7.36 years and 67.38 ± 6.15 years, respectively (p>0.05). Preoperatively, there were no statistical differences between the groups in age, gender distribution, spherical aberration, and visual acuity (p<0.05, all comparisons).
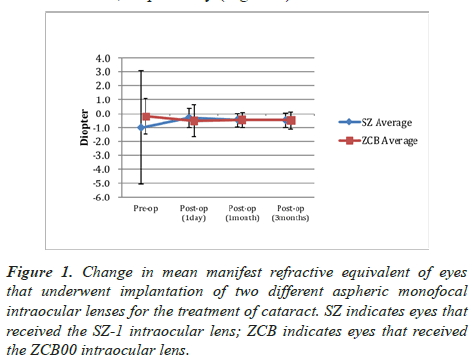
In the SZ-1 group, the mean postoperative MRSE at 1 month and 3 months was −0.88 ± 1.01 D and −0.87 ± 1.08 D, respectively. In the ZCB00 group, these values were −0.54 ± 0.67 D and −0.65 ± 0.76 D, respectively (Figure 1).
The mean change in MRSE from the baseline (preoperatively) to 3 months (postoperatively) was 0.50 ± 0.48 D (95% CI: 0.32–0.68) and 0.80 ± 1.28 D (95% CI: 0.27–1.33), respectively (p=0.25) (Figure 1). The corresponding median values were 0.38 D and 0.38 D, respectively.
At 3 months postoperatively, the mean difference in MRSE from the intended target value was −0.47 ± 0.52 D and −0.47 ± 0.61 D, respectively (p=0.97). The corresponding median values were −0.38 D (95% CI: −0.25-−0.69) and −0.38 D (95% CI: −0.22-−0.73), respectively. At 3 months, all eyes in the SZ-1 group and 96% in the ZCB00 group were ± 1.50 D of the intended MRSE. At 3 months postoperatively, 84% of eyes in both groups were within 1 D of the targeted MRSE and 60% of the SZ-1 group and 68% of the ZCB00 group were within 0.50 D (p>0.05, all between-group comparisons).
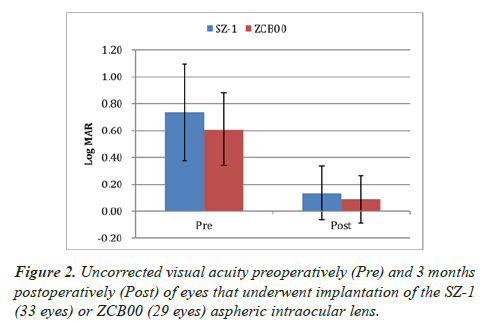
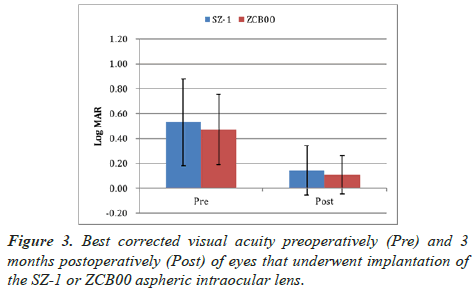
The mean UCVA at 3 months postoperatively in the SZ-1 group and ZCB00 group was 0.13 ± 0.20 LogMAR and 0.09 ± 0.18 LogMAR (p=0.37) (Figure 2). The corresponding median values were 0.05 LogMAR (95% CI: 0.21–0.06) and 0.00 LogMAR (95% CI: 0.16–0.01), respectively. At the same timepoint, the mean BCVA was 0.14 ± 0.20 LogMAR and 0.11 ± 0.17 LogMAR, respectively (p=0.67) (Figure 3). The corresponding median values were 0.05 LogMAR (95% CI: 0.22–0.07) and 0.05 LogMAR (95% CI: 0.17–0.04), respectively.
Three months postoperatively, ocular spherical aberration was statistically significantly different (0.01 ± 0.23 μm vs. −0.51 ± 0.51 μm, respectively (p<0.0001). The corresponding median values were 0.06 μm (95% CI: 0.19-−0.00) and −0.57 μm (95% CI: −0.29-−0.72), respectively.
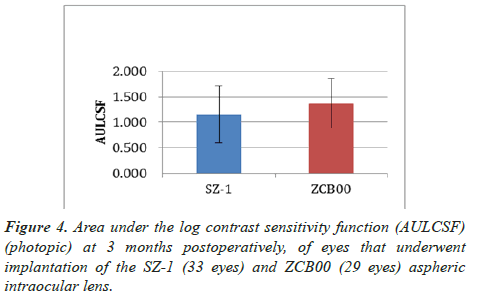
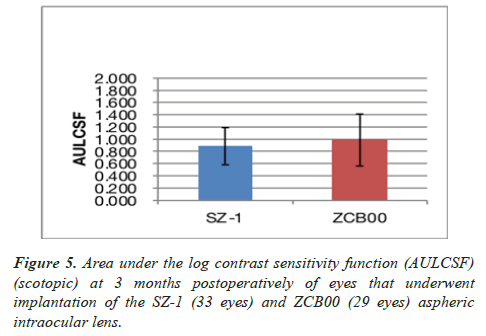
At 3 months postoperatively, the mean photopic AULCSF was 1.15 ± 0.55 and 1.37 ± 0.49, respectively (p=0.41) (Figure 4). The corresponding median values were 1.30 (95% CI: 1.61– 0.69) and 1.52 (95% CI: 1.74–1.00), respectively. At the same time point, the mean scotopic AULCSF was 0.89 ± 0.30 and 0.99 ± 0.43, respectively (p=0.57) (Figure 5). The corresponding median values were 0.81 (95% CI: 1.12–0.65) and 1.22 (95% CI: 1.31–0.66), respectively.
Discussion
To our knowledge, this is the first study comparing the yellowtinted aspheric SZ-1 IOL with the ZCB00 aspheric IOL in a Chinese population. Such comparative studies assist in defining the selection criteria for aspheric IOLs. The aspheric SZ-1 IOL is relatively new compared with the ZCB00. Furthermore, the addition of yellow tinting in the SZ-1 may affect visual performance. The ZCB00 was one of the first aspheric IOLs introduced for cataract surgery and has been extensively studied.
The results of the present study showed that the refractive and visual outcomes were similar among patients who received the SZ-1 or ZCB00 IOL. For example, the mean MRSE at 3 months did not differ clinically (or statistically) between the groups. Additionally, at 3 months postoperatively, 57% and 58% of eyes in the SZ-1 and ZCB00 group had a UCVA of 20/20. Moreover, the mean postoperative BCVA did not differ clinically (or statistically) between the groups. Of note, at 1 month and 3 months, the mean postoperative MRSE in the SZ-1 group was −0.88 ± 1.01 D and −0.87 ± 1.08 D, respectively. In the ZCB00 group, these values were −0.54 ± 0.67 D and -0.65 ± 0.76 D, respectively (Figure 1). However, these differences were not statistically significant. Notably, the SZ-1 group indicated more consistent MRSE at all the examined postoperative time points.
In the present study, the refractive accuracy between the groups was not statistically different. In both groups, 60%–68% of eyes were within 0.50 D of the intended target. This finding is consistent with those reported by Kretz et al. in a study involving the implantation of the ZCB00 lens in a similar population with a higher preoperative spherical equivalent. Kretz et al. reported that 67.6% of examined eyes were within 0.50 D of the intended target [3].
At 3 months postoperatively, the UCVA in the SZ-1 and ZCB00 groups was 0.13 ± 0.20 LogMAR (20/25+) and 0.08 ± 0.18 LogMAR (20/25+), respectively. These results are consistent with those reported in previous studies investigating the implantation of ZCB00 in a similar population (i.e., sample size and mean postoperative MRSE) to that of the ZCB00 group in our study [5]. That study reported that, 6 months postoperative, the UCVA was 0.03 ± 0.11 LogMAR (20/20−).
Studies of aspheric IOLs have consistently shown improved contrast sensitivity and decreased scotopic symptoms compared with spherical IOLs [2,5-9], demonstrating the better optical performance of aspheric IOLs versus spherical IOLs. A recent optical bench comparison of aspheric and spherical IOLs reported statistically higher modulation transfer functions that favored the former design. This difference was even more prominent at larger apertures indicating better performance with larger pupils under mesopic conditions [6]. Studies of contrast sensitivity comparing aspheric with spherical IOLs have reported better visual performance under mesopic conditions with the former lens [7-9]. Furthermore, a study of aspheric IOL implantation in one eye and spherical IOL implantation in the fellow eye reported better overall visual performance in eyes receiving aspheric IOLs [7].
In the current study, the difference in postoperative ocular spherical aberration between the groups was statistically significant. This result was expected due the differing magnitude of spherical aberration between IOLs (i.e., −0.13 μm for the SZ-1 and −0.27 μm for the ZCB00). These spherical aberration values were within the range for normal un-operated eyes in this ethnic population [10-12]. In the present study, the difference in spherical aberration between the groups did not exhibit a statistically or clinically significant effect on photopic and mesopic contrast sensitivity. A study involving a similar ethnic population did not report differences in patient satisfaction after implantation of different aspheric IOLs that resulted in differing magnitudes of spherical aberration postoperatively [13].
Furthermore, the observed similar postoperative contrast sensitivity between the groups indicates that the addition of chromophores in the SZ-1 IOL did not affect visual performance. The blue-blocking chromophore in the SZ-1 filters the shortwavelength light to reduce the risk of macular degeneration [14]. The contrast sensitivity results of the present study concur with those reported in previous studies [9]. A study [9] investigating the same aspheric IOLs with and without a blueblocking chromophore reported similar postoperative photopic and mesopic contrast sensitivity. Notably, a previous study has reported higher mesopic contrast sensitivity in patients with diabetic retinopathy who received spherical IOLs with a blueblocking chromophore versus the same IOL model without chromophore [15].
Limitation of the Study
A limitation of the present study is only total aberrations of the study eyes were calculated. Furthermore, detailed knowledge regarding internal aberrations is essential to obtain precise wavefront measurements. This will be the subject of future investigations.
Conclusion
In summary, the results of this study confirm that the outcomes of SZ-1 and ZCB00 IOL implantation for the treatment of senile cataract are similar. For example, the UCVA and BCVA were not statistically different between the groups. Moreover, the differing asphericity and yellow tinting of the SZ-1 did not affect postoperative visual performance. The differing spherical aberration values observed between these IOLs can be used to address the varying visual demands of patients.
Statement of Ethics
Institutional approval from the Institutional Review Board of Antai Tian-Sheng Memorial Hospital was obtained (18-085-B).
References
- Holladay JT, Piers PA, Koranyi G, et al. A new intraocular design to reduce spherical aberration in pseudophakic eyes. J Refract Surg. 2002;18:683-91.
- Yagci R, Uzun F, Acer S, et al. Comparison of visual quality between aspheric and spherical IOLs. Eur J Ophthalmol. 2014;24:688-92.
- Lombardo M, Lombardo G. Wave aberration of human eyes and new descriptors of image optical quality and visual performance. J Cataract Refract Surg. 2010;36:313-31.
- Barbero S, Marcos S. Analytical tools for customized design of monofocal intraocular lenses. Optics Express. 2007;15:8576-1.
- Kretz FT, Tandogan T, Khoramnia R, et al. High order aberration and straylight evaluation after cataract surgery with implantation of an aspheric, aberration correcting monofocal intraocular lens. Int J Ophthalmol. 2015;8:736-41.
- Pedrotti E, Carones F, Aiello F, et al. Comparative analysis of visual outcomes with 4 intraocular lenses: Monofocal, multifocal, and extended range of vision. J Cataract Refract Surg. 2018;44:156-67.
- Tandogan T, Auffarth GU, Choi CY, et al. In vitro comparative optical bench analysis of a spherical and aspheric optic design of the same IOL model. BMC Ophthalmol. 2017;7:9.
- Kohnen T, Klaproth OK, Bühren J. Effect of intraocular lens asphericity on quality of vision after cataract removal: an intraindividual comparison. Ophthalmology. 2009;116:1697-706.
- Schuster AK, Tesarz J, Vossmerbaeumer U. The impact on vision of aspheric to spherical monofocal intraocular lenses in cataract surgery: a systematic review with meta-analysis. Ophthalmology. 2013;120:2166-75.
- Küchle M. Comparison of visual function with aspheric yellow, aspheric clear and spherical clear intraocular lenses. J Emmetropia. 2013;4:123-30.
- Zhao PF, Li SM, Lu J, et al. Effects of higher-order aberrations on contrast sensitivity in normal eyes of a large myopic population. Int J Ophthalmol. 2017;10:1407-11.
- 12. Lim KL, Fam HB. Ethnic differences in higher-order aberrations: Spherical aberration in the South East Asian Chinese eye. J Cataract Refract Surg. 2009;35:2144-8.
- Wei RH, Lim L, Chan WK, et al. Higher order ocular aberrations in eyes with myopia in a Chinese population. J Refract Surg. 2006;22:695-702.
- Xu ZQ, Song XH, Li WZ, et al. Clinical study inpatient-reported outcomes after binocular implantation of aspheric intraocular lens of different negative spherical aberrations. Asian Pac J Trop Med. 2017;10:710-3.
- Rodríguez-Galietero A, Montés-Micó R, Muñoz G, et al. Blue-light filtering intraocular lens in patients with diabetes: contrast sensitivity and chromatic discrimination. Cataract Refract Surg. 2005;3:2088-92.