Research Article - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 7
Postoperative outcomes of open conjunctival Ab-externo XEN implantation with tenonectomy.
Nicholas A Johnson1,2*, James C Liu2,3, Ang Li2,4, Leon W Herndon2
1Department of Ophthalmology, Duke University School of Medicine, Durham, NC, USA
2Department of Ophthalmology, Duke Eye Center, Duke University, Durham, NC, USA
3Department of Ophthalmology and Visual Sciences, Washington University School of Medicine, St. Louis, MO, USA
4Cole Eye Institute: Cleveland Clinic, Cleveland, OH, USA
- Corresponding Author:
- Dr. Nicholas A. Johnson
Department of Ophthalmology
Duke University
Durham, NC
USA
E-mail: nicholas.johnson@duke.edu
Accepted date: 19 January, 2022
Citation: Johnson NA, Liu JC, Li A, et al. Postoperative outcomes of open conjunctival Ab-externo XEN implantation with tenonectomy. J Clin Ophthalmol 2021;5(7):504-509.
Abstract
Purpose: The goal of this study is to detertmine the efficacy and safety of ab-externo XEN implantation with tenonectomy.
Patients and methods: Patients who underwent ab-externo implantation by a single surgeon (LWH) between February 2019 and December 2020 were included in this retrospective cohort study. Intraocular Pressure (IOP) and glaucoma medication use were collected at postoperative day 1, month 1, month 3, month 6, and month 12. Baseline IOP and medications were compared to postoperative IOP and medications at each time point. Odds of success stratified by patient race and combined vs. standalone procedures were compared at time of last follow-up.
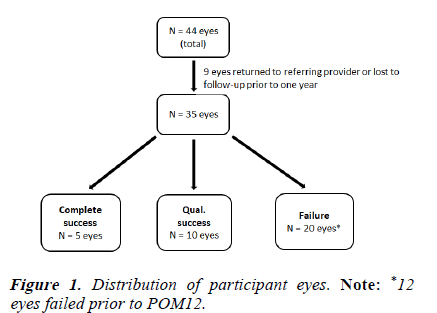
Results: Forty-four eyes of 38 patients were included in this study. Baseline IOP was 20.6 ± 7.2 mmHg. Baseline medication use was 2.5 ± 1.2 medications. Twenty-three eyes had one year follow-up data. Twelve eyes failed prior to POM12. Those that reached POM12 had a mean IOP at POM12 of 14.2 ± 4.0 mmHg (p<0.001) and mean medication use of 1.2 ± 1.4 medications (p<0.001). There were 5 complete successes, 10 qualified successes, and 20 failures at POM12. The odds of failure for whites compared to blacks at POM12 was 2.63 (95% CI=0.63, 11). The odds of failure for solo XEN implantation compared to XEN combined with cataract surgery was 0.93 (95% CI=0.23, 3.82).
Conclusions: Ab-externo XEN implantation with tenonectomy appears to be a safe and effective means of achieveing IOP control and reducing glaucoma medication burden. Success rates using this technique are comparable to previous studies which utilize an ab-interno approach.
Keywords
Minimally Invasive Glaucoma Surgery (MIGS), XEN gel stent, Ab-externo, Tenonectomy..
Introduction
Glaucoma represents a leading cause of blindness worldwide [1]. At present, intraocular Pressure (IOP) is the most significant modifiable risk factor for preventing glaucomatous damage. Management of IOP is achieved by a variety of mechanisms including medical, laser, and surgical therapies [1].
Traditional glaucoma surgeries, such as trabeculectomy and aqueous shunts, have been mainstays of treatment for several decades. Trabeculectomy is a type of glaucoma surgery that involves removal of the trabecular meshwork in order to create a new pathway for aqueous fluid drainage. Aqueous shunt surgery involves implantation of a glaucoma drainage device in order to increase fluid drainage and maintain IOP control. While these techniques have proved effective at lowering IOP, they are not without complications. Aqueous drainage to the front of the eye following these procedures occurs through the subconjunctival space, creating a pocket of fluid commonly referred to as a “bleb.” Common complications of both trabeculectomy and aqueous shunt surgery include low IOP (hypotony), accumulation of fluid in the suprachoroidal space (choroidal effusion), bleb leakage or failure, and blood collection in the front of the eye (hyphema) [2,3]. To minimize the risk of complications, Minimally Invasive Glaucoma Surgery (MIGS) has gained popularity in recent years. MIGS is a group of glaucoma procedures that aim to lower IOP while minimizing tissue trauma via mechanisms such as microstenting or reshaping of the trabecular meshwork. These procedures are intended to offer certain advantages over traditional glaucoma surgery, such as decreased risk of complications and improved visual recovery in the postoperative period [4].
The XEN gel stent (Allergan Inc., Dublin, Ireland) is one such example of a MIGS microstent. The device features a 6 mm long tube with a 45 μm diameter lumen that creates a transscleral channel between the anterior chamber and the subconjunctival space, allowing for continuous aqueous drainage and subsequent IOP lowering [5]. Because clinical trials of the XEN were conducted using an ab-interno surgical approach, the device is currently indicated for ab-interno implantation by the Food and Drug Administration (FDA). However, some surgeons have found comparable success using an ab-externo approach. The potential advantages of an ab- externo approach include better surgical exposure, more reliable subconjunctival placement, and the opportunity for a tenonectomy in order to decrease distal tube plugging.
Previous research suggests that both the ab-interno and abexterno approaches yield similar success in terms of IOP lowering effect and reduction in glaucoma medication burden. However, the amount of evidence regarding the overall efficacy of ab-externo XEN implantation is limited due to the relatively small sample size of previous studies. The current retrospective study aims to add to the growing body of evidence surrounding this technique by evaluating the efficacy of ab-externo XEN implantation with tenonectomy.
Methodology
This retrospective cohort study was approved by the Duke Internal Review Board (Duke University, Durham, NC, USA). All data were acquired via chart review of patient records at a tertiary care center which were confidentially stored within the hospital electronic medical record system. Patient data were deidentified for the purposes of analysis. Investigators did not recontact patients to obtain additional information for the purposes of the study. The data acquisition, storage, and analysis were conducted in accordance with the tenants of the Declaration of Helsinki.
Inclusion/exclusion criteria
Patients who underwent ab-externo XEN implantation with tenonectomy by a single surgeon (LWH) operating with glaucoma fellowship trainees from February 2019 to December 2020 were included in the study. Patients with a history of subconjunctival procedures such as trabeculectomy or aqueous shunt surgery were excluded. There were no exclusion criteria for patients based on the type or severity of glaucoma.
Surgical procedure
A 7-0 vicryl suture is placed through the peripheral cornea and used to rotate the eye down to isolate the supero-temporal or nasal quadrant where lidocaine 2% with epinephrine is injected into the subconjunctival space. Vannas scissors are used to make a small peritomy at the limbus roughly 8 mm in length. Bipolar cautery is used to prepare the scleral bed. An injection of 0.2 ml of Mitomycin-C (MMC) 0.4 mg/ml is applied by sub-Tenon’s irrigation posteriorly as a bolus push with an unneedled TB syringe [6]. After 1-3 minutes (determined based on tissue characteristics), the tissues are irrigated with Balanced Salt Solution (BSS). The XEN stent is inspected and directed through the sclera 2 mm posterior to the limbus. Once the anterior chamber is entered, the stent is advanced until approximately 2 mm of stent is visible in the anterior chamber. A tenonectomy is created to help prevent distal occlusion of the XEN. Finally, the conjunctiva is closed with two wing 9-0 vicryl sutures.
Data analysis
Primary outcomes of interest were postoperative IOP and number of glaucoma medications at postoperative months 1, 3, 6, and 12. Complete success was defined as IOP reduction >20% from baseline without the need for glaucoma medications. Qualified success was defined as IOP reduction >20% from baseline with the help of glaucoma medications, needling, or 5-Fluorouracil (5-FU). Failure was defined as IOP reduction <20%, operative revision of the surgery, the need for additional IOP lowering surgery or loss of light perception. Student’s t-tests were conducted to compare baseline IOP and medication use to postoperative IOP and medication use at each time point. Complications such as hypotony, hyphema, bleb leak, and choroidal effusion were documented at the time in which they occurred in the patients’ charts.
Secondary analyses were conducted to compare success rates by patient race (black vs. white) and combined procedures (XEN+cataract surgery vs. XEN alone). Odds ratios for success at time of last follow-up were compared.
All statistical analysis was performed using Microsoft Excel 2021 version 16.49
Results
Forty-four eyes of 38 patients underwent ab-externo XEN implantation during the study period. Twelve eyes reached failure before the one-year period. The remaining eyes did not have one-year data and were either lost to follow-up or sent back to their referring eye care provider after early postoperative visits. Twenty-three eyes of 21 patients had oneyear follow-up data (Figure 1). Baseline demographic characteristics are included in Table 1.
| Number of patients, n (%) | 38 (100) |
| Female gender, n (%) | 22 (57.9) |
| White race, n (%) | 25 (65.8) |
| Age, years | 75.4 ± 10.4 |
| Baseline IOP, mmHg | 20.6 ± 7.2 |
| Number of medications, n | 2.5 ± 1.2 |
| Combined surgery, n (%) | 15 (39.5) |
| MMC time, min | 1.7 ± 0.8 |
| MMC dose, mcg | 80 |
Note: Values denoted as mean ± standard deviation, unless otherwise stated.
Abbreviations: IOP: Intraocular pressure; MMC: Mitomycin C
Table 1. Baseline demographic data.
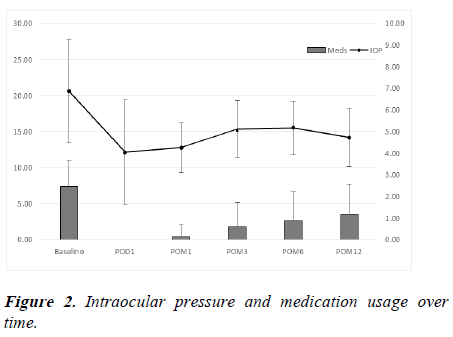
The mean IOP at baseline was 20.6 ± 7.2 mmHg. The average number of medications at baseline was 2.5 ± 1.2 drops. There was an average IOP reduction of 31.1% and average medication reduction of 52% at 1 year (Table 2). Mean IOP differed significantly from baseline mean IOP at each followup time point (p<0.001) (Figure 2).
| Baseline | POD1 | POM1 | POM3 | POM6 | POM12 | |
|---|---|---|---|---|---|---|
| Patients (n) | 44 | 43 | 42 | 38 | 24 | 23 |
| IOP (% reduction) | 20.6 ± 7.2 | 12.2 ± 7.2 (40.8) | 12.8 ± 3.4 (37.9) | 15.3 ± 4.0 (25.7) | 15.4 ± 3.7 (25.2) | 14.2 ± 4.0 (31.1) |
| Meds (% reduction) | 2.5 ± 1.2 | 0 ± 0 (100) | 0.1 ± 0.6 (96) | 0.6 ± 1.1 (76) | 0.8 ± 1.3 (68) | 1.2 ± 1.4 (52) |
Note: Values denoted as mean ± standard deviation, unless otherwise stated.
Abbreviations: IOP: Intraocular pressure; POD: Postoperative day; POM: Postoperative month
Table 2. Intraocular pressure and medication usage follow-up.
At 1 year of follow-up, there were a total of 5 complete successes (14%), 10 qualified successes (29%), and 20 failures (57%). Of the 20 failures, 12 eyes failed prior to 1 year. Eleven eyes required additional incisional surgery (usually due to an insufficient IOP reduction), 8 eyes failed to achieve IOP reduction >20% from baseline at 1 year, and 1 eye had snuff out of vision after surgery. Notable complications included 2 bleb leaks, 2 hyphemas, 1 choroidal effusion, and 1 case of snuff out. Eight eyes required needling plus 5-FU and 3 eyes required 5-FU alone (Table 3).
| Complication | Patients (n) |
|---|---|
| Bleb leak | 2 |
| Hyphema | 2 |
| Choroidal effusion | 1 |
| Loss of light perception (“snuff out”) | 1 |
Table 3. List of notable complications.
Secondary analysis by race revealed that of the 20 eyes which failed, 15 eyes belonged to white patients and 5 eyes belonged to black patients. The odds of failure for white patients compared to black patients at 1 year was 2.63 (95% CI=0.63, 11). Analysis by type of procedure revealed that of 20 failures, 13 eyes underwent solo XEN implantation while 7 eyes were combined with cataract surgery. The odds ratio of failure for eyes which underwent solo XEN implantation compared to eyes combined with cataract surgery was 0.93 (95% CI=0.23, 3.82).
Discussion
There is a growing body of evidence to support the use of abexterno XEN implantation for treatment of glaucoma. Case reports have shown efficacy of ab-externo XEN implantation in patients with unique surgical history, such as refractory glaucoma following keratoplasty [7,8]. However, this technique has also demonstrated comparable effectiveness in a more generalized glaucoma patient population when compared to traditional ab-interno implantation. Two recent studies have compared postoperative results of ab-interno versus ab-externo implantation. A study by Ucar, et al. compared 43 eyes which underwent ab-externo implantation against 44 eyes which underwent ab-interno implantation and found that both groups achieved significant IOP lowering and reduction in glaucoma medications for up to one year of follow-up. The authors also noted a significantly decreased need for postoperative bleb needling in the ab-externo group [9]. Another study by Tan, et al. which compared 50 ab-interno eyes to 30 ab-externo eyes found no difference in IOP lowering, medication use reduction, or need for postoperative needling or additional surgery between the two groups [10].
Previous studies examining the efficacy of this technique have been relatively small in sample size. The goal of this retrospective study was to add to the expanding literature about the efficacy of this technique. The results of the current study suggest that ab-externo XEN implantation achieves favorable IOP lowering effect and reduction in glaucoma medication burden up to one year in this population of patients. Although rates of complete and qualified success at one year were modest, these results demonstrate similar efficacy compared to an ab-interno technique. In this study, the average IOP decreased by 31% from baseline at POM12, while average number of glaucoma medications decased by 52% from baseline at POM12. Previous studies by Torregrosa, et al. and Tan, et al. observed an average IOP decrease by 29% and 42% from baseline at POM12, respectively, using an ab-interno approach [11,12]. A recent review by Fea and colleagues summarizes findings of several recent XEN studies, most of which demonstrate IOP lowering efficacy that is on par with the aforementioned studies [13]. This trend is also observed for number of glaucoma medications, in which the average number of medications often decreases by one to three medications at the one-year follow-up period [13]. Our own sample, which saw an average decrease from 2.5 ± 1.2 medications at baseline to 1.2 ± 1.4 medications at one year, demonstrated comparable efficacy by this metric.
Although the ab-externo technique successfully lowered IOP and decreased medication burden, there was a significant rate of failure (57%) at one year. Eleven of the 20 failures at POM12 required additional surgery to achieve adequate IOP control. The most common indications for additional surgery included bleb revision for bleb leak or encapsulated bleb (4 cases), as well as the need for traditional glaucoma surgery, most commonly in the form of trabeculectomy (6 cases). Rates of complete success (14%) and qualified success (29%) at one year are comparable to success rates found in previous XEN studies employing an ab-interno approach. In sample of 199 eyes, Heidinger, et al. observed a complete success rate of 15.4% and a qualified success rate of 25% at 12 months [14]. The authors defined qualified success as IOP reduction ≤20% of baseline with an IOP <18 mmHg with glaucoma medications. In a study of 13 eyes that underwent either XEN implantation alone or XEN + phacoemulsification by Galal, et al. 42% of eyes had IOP reduction >20% without medications at one year, while 67% had IOP reduction >20% with medications [15]. Several additional studies quote similar rates of success in patients receiving ab-interno XEN implantation [13]. It is important to note that studies regularly differ in their definitions of success and failure. Thus, movements towards a standardized definition of success or failure may be beneficial for the purposes of generalizing these findings.
The utility of tenonectomy during ab-externo XEN implantation has not been previously described in the literature. In pediatric populations, tenonectomy during standard trabeculectomy has been shown to support better IOP control and reduced number of glaucoma medications [16]. However, previous studies in adults have noted no difference in glaucoma management between patients who receive tenonectomy with trabeculectomy and those who do not [17]. The goal of performing tenonectomy in the current study was to prevent distal occlusion of the XEN by Tenon’s capsule during the postoperative period and decrease the need for bleb needling if tenonectomy is performed. Eight of 44 eyes in the current study required postoperative needling (18%), which is lower than previous studies which did not utilize tenonectomy [18]. This suggests that tenonectomy may decrease the need for postoperative needling, though the sample size of this study limits the generalizability of this conclusion. Additional studies comparing success rates with and without tenonectomy are needed to determine whether this technique significantly reduces risk of complications or the need for bleb needling. The decision to perform a tenonectomy may be left to surgeon’s preference, as results demonstrate that overall success may be achieved with or without the use of this technique.
The utility of bleb needling in fibrotic blebs following XEN implantation has been previously described. Needling has been shown to restore filtration and maintain durable IOP-lowering potential in the post-operative period [19,20]. Certain factors which have been shown to predict increased success after needling include being on two types of medications or fewer medications previously, solo XEN procedure, and patients with higher IOP difference after day 1 of needling [19]. Complications associated with needling include partial amputation of the XEN, hypotony, choroidal detachment, and failure to achieve adequate IOP control [20]. Of the 8 eyes which required needling in our cohort, 3 eyes (37.5%) eventually reached failure due to need for additional surgery. However, none of these eyes experienced direct complications from bleb needling. Thus, although the utility of needling in cases where tenonectomy and conjunctival dissection has been performed may only modestly improve chance of success, it appears to be a safe procedure with minimal risk of complication.
This study is the first to attempt to describe race differences with regards to the XEN using an ab-externo approach. Race differences in conjunctival histology between black and white patients have been cited in previous studies. It has been proposed that black patients tend to have increased number of conjunctival macrophages and fibroblasts [21], while white patients tend to have increased number of conjunctival mast cells [21,22]. However, the clinical implications of these findings are not fully understood. In our sample, secondary analysis of race differences showed increased odds of failure in white patients compared to black patients at one year (OR=2.63 (95% CI=0.63, 11)). These results suggests that black patients may have an increased chance of success when receiving ab-externo XEN implantation compared to white patients. While race differences in conjunctival histology may exist, the results of this study conflict with previous assertions that black patients may be more prone to scarring and thus are at increased risk of failure in filtration surgeries. Indeed, one significant limitation of our study may be that the bias of black patients being more prone to failure may have caused a selection bias in this cohort. The small sample size of the current study necessitates further exploration of this trend.
There is currently a debate in the literature about whether the XEN is more efficacious when combined with cataract surgery. In the current sample, analysis of standalone XEN compared to combination XEN+cataract surgery demonstrated marginally decreased odds of failure when XEN was performed as a solo procedure compared to combined procedures at one year (OR=0.93 (95% CI=0.23, 3.82)). Previous research surrounding this topic has yielded mixed results. Most previous studies which compare solo XEN to combination XEN procedures have found that both solo and combination procedures achieve good IOP lowering effect and medication reduction, with no significant differences in success rates between the two [14,23,24]. However, in a study by Fea, et al. comparing solo XEN to combination XEN, the XEN solo group achieved higher success rates compared to the combo group if a success cutoff of IOP decrease ≤14 mmHg was used [25]. Similarly, in a study by Widder, et al. pseudophakic eyes undergoing solo XEN procedures had higher success rates compared to phakic eyes undergoing combo procedures [26]. Still, the majority of studies have found no significant difference in efficacy or success rates of solo XEN versus combination XEN procedures, which was similar to our experience.
Conclusion
The use of ab-externo XEN implantation with tenonectomy appears to be a safe and effective means for achieving IOP control and reducing glaucoma medication burden in the current sample of patients. The overall efficacy and rates of complications in this cohort are comparable to other studies of patients receiving ab-interno XEN implantation. As with other MIGS procedures, both ab-interno and ab-externo XEN implantation are reasonable options for achieving IOP control in glaucoma patients.
References
- Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: A review. Jama. 2014; 311:1901-11.
- Kaplowitz K, Bussel II, Honkanen R, et al. Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol. 2016; 100:594-600.
- Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012; 153:804-14.
- Saheb H, Ahmed II. Micro-invasive glaucoma surgery: Current perspectives and future directions. Curr Opin Ophthalmol. 2012; 23:96-104.
- Chaudhary A, Salinas L, Guidotti J, et al. XEN Gel Implant: A new surgical approach in glaucoma. Expert Rev Med Devices. 2018; 15:47-59.
- Quist MS, Brown N, Bicket AK, et al. The short-term effect of subtenon sponge application versus subtenon irrigation of mitomycin-C on the outcomes of trabeculectomy with ex-press glaucoma filtration device: A randomized trial. J Glaucoma. 2018; 27:148-56.
- Tan SY, Din NM, Khialdin SM, et al. Ab-externo implantation of xen gel stent for refractory steroid-induced glaucoma after lamellar keratoplasty. Cureus. 2021; 13:e13320.
- Fu L, Baker ML, Carley F, et al. Subconjunctival ab externo gel stent implantation for refractory glaucoma after high-risk penetrating keratoplasty. Cureus. 2020; 12:e8873.
- Ucar F, Cetinkaya S. Xen implantation in patients with primary open-angle glaucoma: Comparison of two different techniques. Int Ophthalmol. 2020; 40:2487-94.
- Tan NE, Tracer N, Terraciano A, et al. Comparison of safety and efficacy between ab interno and ab externo approaches to xen gel stent placement. Clin Ophthalmo. 2021; 15:299-305.
- Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, et al. Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 2016; 91:415-21.
- Tan SZ, Walkden A, Au L. One-year result of XEN45 implant for glaucoma: Efficacy, safety, and postoperative management. Eye. 2018; 32:324-32.
- Fea AM, Durr GM, Marolo P, et al. XEN® gel stent: A comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020; 14:1805-32.
- Heidinger A, Schwab C, Lindner E, et al. A retrospective study of 199 Xen45 stent implantations from 2014 to 2016. J Glaucoma. 2019; 28:75-9.
- Galal A, Bilgic A, Eltanamly R, et al. XEN glaucoma implant with mitomycin C 1 year follow-up: Result and complications. J Ophthalmol. 2017.
- Awadein A, El Sayed YM. Excision of tenon capsule in pediatric trabeculectomy: A controlled study. J Glaucoma. 2016; 25:39-44.
- Miller KN, Blasini M, Shields MB, et al. A comparison of total and partial tenonectomy with trabeculectomy. Am J Ophthalmol. 1991; 111:323-6.
- Buffault J, Baudouin C, Labbé A. XEN® gel stent for management of chronic open angle glaucoma: A review of the literature. J Fr Ophtalmol. 2019; 42:e37-46.
- José P, Teixeira FJ, Barão RC, et al. Needling after XEN gel implant: What’s the efficacy? A 1-year analysis. Eur J Ophthalmol. 2020.
- Midha N, Gillmann K, Chaudhary A, et al. Efficacy of needling revision after XEN gel stent implantation: A prospective study. J Glaucoma. 2020; 29:11-4.
- Broadway D, Grierson I, Hitchings R. Racial differences in the results of glaucoma filtration surgery: Are racial differences in the conjunctival cell profile important? Br J Ophthalmol. 1994; 78:466-75.
- McMillan TA, Stewart WC, Hennis HL, et al. Histologic differences in the conjunctiva of black and white glaucoma patients. Ophthalmic Surg. 1992; 23:762-5.
- Hengerer FH, Kohnen T, Mueller M, et al. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017; 26:1130-6.
- Reitsamer H, Sng C, Vera V, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019; 257:983-96.
- Fea AM, Bron AM, Economou MA, et al. European study of the efficacy of a cross-linked gel stent for the treatment of glaucoma. J Cataract Refract Surg. 2020; 46:441-50.
- Widder RA, Dietlein TS, Dinslage S, et al. The XEN45 Gel Stent as a minimally invasive procedure in glaucoma surgery: Success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol. 2018; 256:765-71.