Research Article - Journal of Clinical Ophthalmology (2019) Volume 3, Issue 2
One-year evaluation of the performance of the Trulign toric intraocular lens implanted in eyes using intraoperative aberrometry to determine sphere, cylinder and position.
P Dee G Stephenson*
Stephenson Eye Associates, 200 Palermo Place, Venice, FL, USA
- Corresponding Author:
- Dee G Stephenson, MD
Stephenson Eye Associates 200
Palermo Place Venice, FL 34285, USA
E-mail: eyedrdee@aol.com
Accepted date: November 21, 2019
Citation: Stephenson PDG. One-year evaluation of the performance of the Trulign toric intraocular lens implanted in eyes using intraoperative aberrometry to determine sphere, cylinder and position. J Clin Ophthalmol. 2019;3(2):162-165.
Abstract
Objective: To evaluate the performance of the Trulign toric intraocular lens (IOL) positioned with intraoperative aberrometry in eyes with one year of follow-up.
Design: Masked, retrospective data analysis.
Participants: All patients implanted with a Trulign toric IOL between June 2013 and September 2014.
Methods: All eligible patients underwent phacoemulsification cataract surgery by the same surgeon and were implanted with a Trulign toric IOL (1.25 D, 2.00 D, or 2.75 D). Preoperatively, astigmatism correction was determined by a toric calculator. Intraoperative aberrometry provided real-time data validation and determined final spherical and cylinder power as well as axis of placement. Data were entered in a registry. Postoperatively, uncorrected distance (UDVA), intermediate (UIVA), and near (UNVA) visual acuities (VA), postoperative residual refractive astigmatism (RRA), and best-corrected distance VA (CDVA), were evaluated.
Results: A total of 115 eyes were available for the 1 year visit. All eyes achieved 20/40 or better CDVA. Uncorrected visual acuity of ≥ 20/25 was achieved by 83% of eyes at distance, 95% at intermediate and 81% at near. Mean UDVA was LogMAR 0.06 ± 0.09, UIVA was -0.01 ± 0.09 and UNVA was 0.07 ± 0.08. RRA was ≤ 0.5 D in 98% of eyes and ≤ 1.0 D in 98% of eyes.
Conclusion: The Trulign toric IOL provided good functional vision at distance, intermediate and near with minimal RRA after cataract surgery with guidance provided by intraoperative wavefront aberrometry.
Keywords
Residual refractive astigmatism, Refractive error, Premium intraocular lens, Presbyopia.
Introduction
Patients have developed high expectations for their visual acuity (VA) after cataract surgery. In response, surgeons have become adept at the biometric measures and calculations necessary to reduce spherical refractive error after intraocular lens (IOL) implantation. Even so, a large cohort study found that emmetropia was achieved in only about half the surgical cases. A major factor contributing to this postoperative refractive surprise was residual corneal astigmatism [1].
Preoperative keratometric stigmatism >1.0 diopter (D) occurs in one-third and >1.5 D in 6%-18% of eyes undergoing cataract surgery [2-4]. Astigmatism has a subjective blurring effect similar to spherical defocus of the same magnitude [5]. Even 1.0 D of astigmatic error can compromise reading vision and the ability to drive at night [6]. The presence of uncorrected astigmatism also negatively affects quality of life [7].
A systematic review of VA reported improved uncorrected distance visual acuity (UDVA) in patients implanted with toric IOLs following cataract surgery [8]. Compared to incisional procedures used to correct astigmatism (limbal relaxing incisions, LASIK), toric IOLs avoid issues with variable healing of the incision, wound gape and the possibility of corneal denervation, perforation or infection [9].
The pivotal trial of the Trulign toric IOL reported that the IOL achieved all efficacy endpoints at 6 months postoperative [10]. To our knowledge, there are no published studies of this IOL with >6 months follow-up. The purpose of this retrospective study was to assess astigmatic and VA outcomes after 1 year in eyes implanted with the Trulign toric IOL in a routine clinical setting.
Materials and Methods
The current research project meets the conditions for exemption from Institutional Review Board (IRB) review (Western Institutional Review Board, Puyallup, WA, USA). Data were entered into the AnalyzOR, the ORA System’ s secure database. Patient identifiers were masked before data analysis. All eyes were implanted by a single surgeon (PDGS) with the Trulign toric IOL. This is a consecutive series of the first eyes implanted by PDGS with the Trulign toric IOL over a 16-month period (approximately 100 eyes).
Intraocular lens
The Trulign toric IOL is a silicone modified plate IOL with polyimide haptics. The optic has a 5 mm diameter with an overall lens diameter of 11.5 mm. Axis markings are on the anterior, aspheric surface of the lens and toric correction is on the posterior surface. Three lenses are available in the BL1UT (cylinder power) toric series based on cylinder power at the IOL plane: BL1UT125 (1.25 D), BLT1UT200 (2.00 D) or BL1UT275 (2.75 D).
Preoperative assessment
Preoperative assessment included ocular coherence tomography of the macula (Topcon Medical Systems Inc, Oakland, NJ) and corneal topography (Cassini, The Hague, The Netherlands). Lens power was calculated using the IOLMaster 500 (Carl Zeiss Meditec, Dublin, CA, USA) and the proprietary online Trulign Toric Calculator (Bausch +Lomb, Irvine, CA.
Surgical procedure
Standard microincision phacoemulsification (Stellaris system, Bausch+Lomb, Rochester, NY, USA) was performed through a 1.8 mm incision. A 5.25 mm circular capsulorhexis, created with a femtosecond laser, (Lensar Inc, Orlando, FL) allowed free movement of the IOL optic. A capsular tension ring was inserted in all eyes. After phacoemulsification of the crystalline lens, the capsule was polished, the phaco incision extended to 2.8 mm and the toric IOL inserted and aligned. Viscoelastic was removed and the IOL checked to ensure alignment.
Wave front aberrometry
During surgery, intraoperative aberrometry (ORA System, Alcon Labs Inc, Fort Worth, TX) was used to verify the lens choice. Patients were targeted for a postoperative spherical equivalent of plano in the dominant eye and -0.5 D in the nondominant eye.
Postoperative assessment
The primary endpoint was RRA determined by manifest refraction. Secondary endpoints were best-corrected distance visual acuity (CDVA), and UDVA, uncorrected intermediate (UI) and uncorrected near (UN) VA. The Optec 6500 Vision Tester (Stereo Optical Co, Chicago, IL) was used for VA measurements at distance, near (40 cm) and intermediate (80 cm). Safety assessments were CDVA of 20/40 or better and adverse events.
Results
A total of 116 eyes of 76 patients were implanted with a Trulign toric IOL (Table 1). Data were available for 100 eyes at the 1 month visit, 63 eyes at 3 months and 115 eyes at the 1 year visit.
| Mean ± SD | Range | |
|---|---|---|
| Age | 70 | 56-88 |
| Gender | 34 Male 42 Female | - |
| Final visit (days postoperative) | 553 ± 170 | 394-958 |
| Preoperative K flat | 43 ± 2.0 | 36-47 |
| Preoperative K steep | 44 ± 1.9 | 38-48 |
| Axial length (mm) | 23.8 ± 0.97 | 21.6-26.2 |
| Preoperative astigmatism (diopters) | 1.11 ± 0.75 | 0.22-3.62 |
*SD: Standard Deviation; mm: Millimeter
Table 1. Patient demographics.
Mean postoperative follow-up was 553 ± 170 days (range 304-958 days). The distribution of IOLs was BL1UT125 (n=35), BL1UT200 (n=46) and BL1UT275 (n=35). In 40.0% of eyes (46/115), intraoperative aberrometry confirmed the surgeon ’ s calculations. The position or power of the IOL changed intraoperatively in 60.0% (69/115) of cases. Of these, 20 cases were planned for implantation of a non-toric IOL and were changed to implantation of a BL1UT IOL based on intraoperative aberrometry.
Visual outcomes
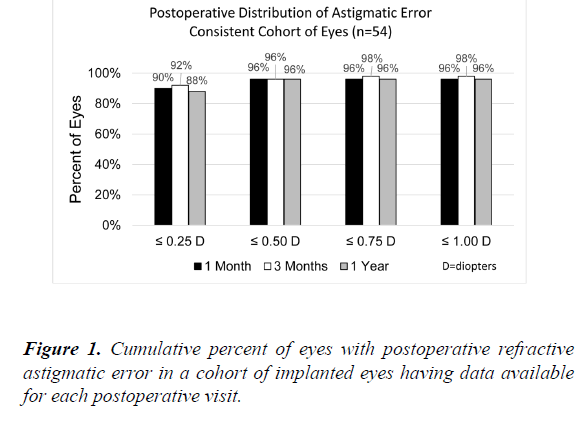
The distribution of RRA at each follow-up visit is shown in Table 2. A cohort of 54 eyes with data available from each postoperative visit demonstrated a consistent distribution of RRA error over time (Figure 1). Mean RRA in this group was 0.10 D ± 0.25 at 1 month, 0.07 D ± 0.23 at 3 months and 0.11 D ± 0.34 at 1 year postoperative.
| Percent of Eyes | |||
|---|---|---|---|
| Residual Cylinder (D=diopters) | 1 Month (n=100) | 3 Months (n=63) | 1 Year (n=115) |
| ≤ 0.25 D | 92% | 95% | 94% |
| ≤ 0.50 D | 97% | 97% | 98% |
| ≤ 0.75 D | 98% | 98% | 98% |
| ≤ 1.00 D | 99% | 100% | 98% |
| Mean Residual Cylinder | 0.08 D ± 0.21 | 0.04 D ± 0.16 | 0.07 D ± 0.26 |
Table 2. Distribution of postoperative residual refractive cylinder.
The distribution of UDVA at each postoperative visit is shown in Table 3. The cumulative distributions of CDVA, UDVA, UIVA, and UNVA are shown in Table 4.
| Percent of Eyes | |||
|---|---|---|---|
| Cumulative Snellen Equivalents | 1 Month (n=100) | 3 Months (n=63) |
1 Year (n=115) |
| 20/20 or better | 42% | 57% | 50% |
| 20/25 or better | 75% | 79% | 83% |
| 20/30 or better | 87% | 95% | 96% |
| 20/40 or better | 100% | 100% | 100% |
Table 3. Distribution of uncorrected distance visual acuities over time.
| Percent of Eyes (n=115) | ||||
|---|---|---|---|---|
| Snellen | Uncorrected Distance Visual Acuity | Uncorrected Intermediate Visual Acuity | Uncorrected Near Visual Acuity | Best-corrected Distance Visual Acuity |
| 20/15 or better | 8% | 25% | 7% | 11% |
| 20/20 or better | 50% | 80% | 42% | 98% |
| 20/25 or better | 83% | 95% | 81% | 100% |
| 20/30 or better | 96% | 100% | 97% | 100% |
| 20/40 or better | 100% | 100% | 100% | 100% |
| Mean Visual Acuity | 20/23 | 20/20 | 20/23 | 20/19 |
Table 4. Cumulative distribution of visual acuity at distance, intermediate and near at final visit.
Safety
None of the implanted IOLs had to be realigned postoperatively due to rotation. All eyes had CDVA of 20/20 or better and UDVA of 20/40 or better 1 year postoperative. There were no complications or adverse events in this series of cases.
Discussion
This study assessed outcomes for RRA and VA in eyes implanted with the Trulign toric IOL. Over 90% of implanted eyes achieved an RRA within ± 0.25 D from the 1 month to the 1 year visits. Study eyes also consistently achieved good, functional uncorrected visual acuity at distance, intermediate and near through the 1 year postoperative visit.
Residual refractive cylinder
The levels of RRA were very low. Residual refractive astigmatism was ≤ 0.25 D in almost all eyes (92%) at 1 month and was maintained through the final 1 year visit (94%). Consistency was demonstrated by the almost identical percentages of eyes with RRA ≤ 0.5 D and ≤ 1.0 D at 1, 3 and 12 months postoperative in the consistent cohort of 54 eyes. A 1 month study of eyes implanted with the Trulign toric IOL (n=40 eyes), in which intraoperative aberrometry was used, reported similar results. Postoperative astigmatism was ≤ 0.50 D in 97.5% of eyes and ≤ 1.0 D in 100% of eyes [11]. In the Trulign toric IOL pivotal clinical trial (n=138), 78.4% of eyes were within ± 0.5 D and 95.5% were within ± 1.0 D of predicted postoperative refractive astigmatism at the final visit of 4-6 months. In this randomized, controlled trial, postoperative residual refractive astigmatism was significantly lower compared to eyes implanted with the Crystalens IOL; a lens similar to the Trulign toric IOL but lacking the toric surface [10].
The improved results in the current study and the study by Epitropoulos [11] compared to the Trulign toric IOL pivotal clinical trial may be related to the use of intraoperative aberrometry in these two studies. In the current study, adjustments were made to the IOL in 60% of cases based on the information provided by intraoperative aberrometry. A paired-eye study of toric IOL implantation showed significantly more eyes implanted using intraoperative aberrometry had ≤ 0.5 D of astigmatism compared to eyes implanted using standard biometry along with a toric calculator [12].
Achievement of ≤ 0.5 D RRA was generally more successful in the current study than 1 year studies of other toric IOLs. The 1 year pivotal clinical trial of an acrylic toric IOL demonstrated that 53.3% of patients implanted with the AcrySof toric IOL (Alcon Labs, Inc. Fort Worth, TX) had RRA measuring ≤ 0.5 D and 88.0% had RRA measuring ≤ 1.0 D [13]. A 2013 review of toric IOL studies, predominantly the AcrySof toric IOL, reported that across studies, the percent of eyes with RRA ≤ 1.0 D ranged from 50% to 100% and the range for those ≤ 0.5 D was 25% to 100% [14]. Only 2 of these studies included data from at least a 1 year follow-up. Kim et al reported 86.7% of eyes implanted with an AcrySof IOL (n=30) had RRA ≤ 0.5 D and 100% were ≤ 1.0 D [15]. Ruhswurm et al followed 37 eyes implanted with the Staar toric IOL (Staar Surgical, Monrovia, CA) for 20 months and found 49% of eyes with RRA ± 0.5 D and 78% within ± 1.0 D [16].
Visual acuity
All eyes in the current study had an UDVA of 20/40 or better. Uncorrected visual acuity of 20/30 or better was achieved by over 96% of eyes at distance, intermediate, and near. Similar results were reported from a 1 month study of the Trulign toric IOL. Visual acuity of 20/25 or better was reported in 95% of eyes at distance and at intermediate. Near VA of 20/40 or better was achieved by 92.5% of eyes [11]. The Trulign pivotal trial reported 97.8% of eyes achieved a UDVA of 20/40 or better, 97.8% achieved 20/40 or better UIVA and 70.1% achieved 20/40 or better UNVA [10].
One-year results from the AcrySof randomized, controlled trial noted 77.7% of eyes achieved a CDVA of 20/20 or better and 40.7% of eyes achieved an UDVA of 20/20 or better [13]. In the review of toric IOLs by Visser, 5% to 40% of eyes implanted with toric IOLs achieved an UDVA of 20/20 or better [14]. A systematic review of toric IOLs calculated that 67.5% of eyes implanted with toric IOLs achieved a visual acuity of 20/20 or better [17]. As all the toric IOLs reviewed were non-accommodating, monofocal IOLs, no VA measures were taken at intermediate or near.
Strengths of the current trial are the extended follow-up of 1 year and the assessment of RRA and VA, the two most important outcomes to patients, in a ‘ real world ’ clinical practice. A limitation is the retrospective nature of the study. Precise measurement of IOL rotation is not part of the standard follow-up visit in this practice. However, the consistency of both RRA and VA measures suggest that the IOL is stable up to 1 year postoperative. This is in line with the pivotal clinical trial, in which Trulign IOL rotation usually occurred early after surgery. At 4-6 months 96.1% of IOLs had rotated<5° [10]. In addition, all eyes in this study were implanted with a capsular tension ring to improve stability [18].
Conclusion
The Trulign toric IOL, implanted with power and placement guidance provided by intraoperative aberrometry, provided good visual acuity outcomes at distance, intermediate, and near with minimal residual refractive astigmatism. The results were stable over postoperative year 1.
Acknowledgements
This study was supported by an independent grant from Bausch+Lomb, Inc.
References
- Behndig A, Montan P, Stenevi U, et al. Aiming for emmetropia after cataract surgery: Swedish National Cataract Register study. J Cataract Refract Surg. 2012;38:1181-6.
- Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36:1479-85.
- Hill WE. Prevalence of corneal astigmatism prior to cataract surgery. http://www.doctor-hill.com/physicians/docs/Astigmatism.pdf. [accessed 4/2/2017]
- Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70-5.
- Atchison DA, Guo H, Charman WN, et al. Blur limits for defocus, astigmatism and trefoil. Vision Res. 2009;49:2393-403.
- Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refract Surg. 2011;37:454-60.
- Savage H, Rothstein M, Davuluri G, et al. Myopic astigmatism and presbyopia trial. Am J Ophthalmol. 2003;135:628-32.
- Agresta B, Knorz MC, Donatti C, et al. Visual acuity improvements after implantation of toric intraocular lenses in cataract patients with astigmatism: a systematic review. BMC Ophthalmol. 2012;12:41.
- Netto MV, Mohan RR, Ambrosio R Jr, et al. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea. 2005;24:509 –22.
- Pepose JS, Hayashida J, Hovanesian J, et al. Safety and effectiveness of a new toric presbyopia-correcting posterior chamber silicone intraocular lens. J Cataract Refract Surg. 2015;41:295-305.
- Epitropoulos AT. Visual and refractive outcomes of a toric presbyopia-correcting intraocular lens. J Ophthalmol. 2016;2016:7458210.
- Woodcock MG, Lehmann R, Cionni RJ, et al. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser: One-month results. J Cataract Refract Surg. 2016;42:817-25.
- Holland E, Lane S, Horn JD, et al. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117:2104-11.
- Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: Historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39:624-37.
- Kim MH, Chung TY, Chung ES. Long-term efficacy and rotational stability of AcrySof toric intraocular lens implantation in cataract surgery. Korean J Ophthalmol. 2010;24:207-12.
- Ruhswurm I, Scholz U, Zehetmayer M, et al. Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg. 2000;26:1022-7.
- Kessel L, Andresen J, Tendal B, et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and meta-analysis. Ophthalmology. 2016;123:275-86.
- Alió JL, Elkady B, Ortiz D, et al. Microincision multifocal intraocular lens with and without a capsular tension ring: optical quality and clinical outcomes. J Cataract Refract Surg. 2008;34:1468-75.