Research Article - Journal of Advanced Surgical Research (2017) Volume 1, Issue 1
Neoadjuvant chemotherapy (NCH) followed by abdominal radical trachelectomy (ART) in cervical cancer: long term follow up results of the Buenos Aires experience
Alejandro Soderini1*, Alejandro Aragona2, Evangelina Bonavía1, Horacio Moschen1, Martin Mendez1, Rosa Garrido2, Diana Martinez2, Nicasio Cuneo1
1Oncologic Hospital of Buenos Aires Marie Curie, the University of Buenos Aires, Argentina
2Gynecologic Oncology Unit, Oncologic Hospital of Buenos Aires “Marie Curie”, Argentina
- *Corresponding Author:
- Alejandro Soderini
Oncologic Hospital of Buenos Aires Marie Curie
The University of Buenos Aires
Argentina
Tel: 5491157420830
E-mail: alejandro.soderini@yahoo.com.ar
Accepted date: January 09, 2017
Abstract
Objectives: To analyze the long term follow up results of NCH followed by art in stages ib1 >2 cm and <4 cm squamous cervical carcinomas.
Methods: Prospective trial over 27 pts. submitted to an art between 10/04-10/15. In five cases stages ib1, (tumor >2 & <4 cm), underwent platinum based NCH. They were staged under figo´s staging system. MRI scan and hysteroscopy were performed before and after NCH as presurgical staging studies. Patients were included by the intention to treat. The surgery was performed 1 month after the last cycle of NCH. The art was sparing the uterine arteries and hypogastric plexus and was performed always by the same surgical team. Long term follow up results and survival rates were analyzed.
Results: Median age: 27, 5 years old. The art could be successfully performed in 4/5 cases. Toxicity: hematologic, grade 1; alopecia, grade 2. MRI and hysteroscopy confirmed the tumor response after NCH. Three women got pregnant, one of them, twice. Pregnancies were spontaneously conceived. Three deliveries by cesarean section at 35, 5 weeks were done, obtaining 3 healthy new-borns. One case of abortion. Neither complications were observed during the prenatal controls nor at and after the surgery. No case of corioamnionitis was registered. No neonatal adverse effects occurred related to the chemotherapy scheme given. OS and DFs: 100%. Follow-up: 8- 72 months. The follow up after births was 8 and 30 months, free of disease.
Conclusions: NCH followed by art, is obstetrically and oncologically safe. It could be taken into account for selected patients with stages ib1 with tumors between 2-4 cm.
Keywords
Cervical cancer, Neoadjuvant Chemotherapy, Radical Trachelectomy, Nerve sparing, Fertility sparing
Introduction
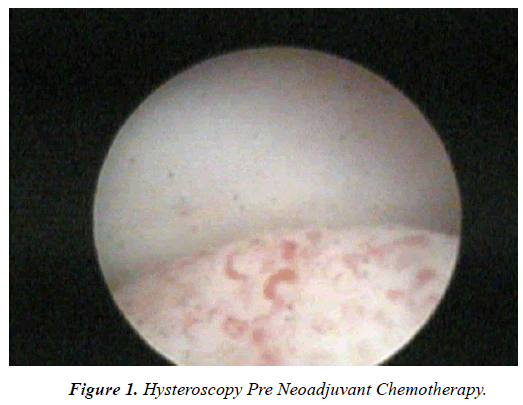
Cervical cancer is one of the most common types of cancer in women under the age of 40 with survival rates around 90% in for stageIb1 [1]. In recent decades, women are having their first child at later ages for different social and cultural reasons, and therefore the diagnosis of cervical cancer in women of child bearing age presents a dilemma not only in terms of disease control and management, quality of life, and sexual life, but also in terms of fertility, a landmark in any woman´s life. The standard treatment in the early stages of the disease is radical hysterectomy, which leads to infertility. Although conisation of the cervix is a widely used traditional method, it is limited only to stages Ia1 (Figure 1).
The so called radical trachelectomy technique was introduced in the last decades that are the removal of the cervix with the parametria and the vaginal cuff, enabling preservation of the body of the uterus and later pregnancy and birth. The technique became an acceptable approach for cervix cancer management. To date a recurrence rate of 4.1% and a death rate of 2.8% have been reported in vaginal radical trachelectomy, similar to the results observed with radical hysterectomy [2], and encouraging obstetric results.
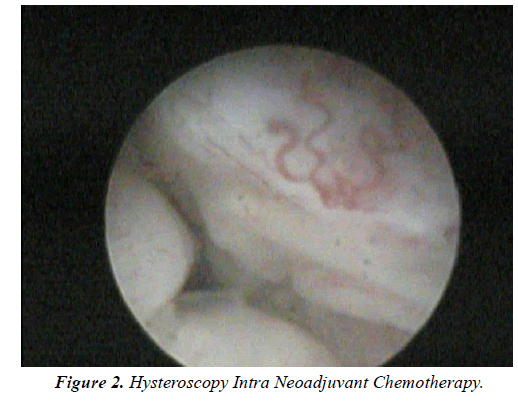
Radical trachelectomy may be performed using two different approaches; the vaginal approach, with laparoscopic lymphadenectomy, first reported and promoted by Dargent et al. [3] and used by many schools and the abdominal approach reported by Ungar et al. (Figure 2) [4].
To perform the vaginal approach, the ascending branch of the uterine artery is preserved only the lower cervicovaginal branches are ligated, whereas in the abdominal approach the uterine artery is sectioned for a better exposure of the operating field, and therefore accurately remove the parametria. Blood for the uterus is mainly supplied by the ovarian arteries. Some authors have reported the use of uterine artery anastomosis after sectioning and mobilization [5].
In the case of women undergoing the abdominal approach, the pregnancy rate is lower than in those treated with the vaginal approach [6-10]. Some authors point out that the preservation of the uterine artery or its ascending branch is a factor, which might play important role in future obstetric results [11].
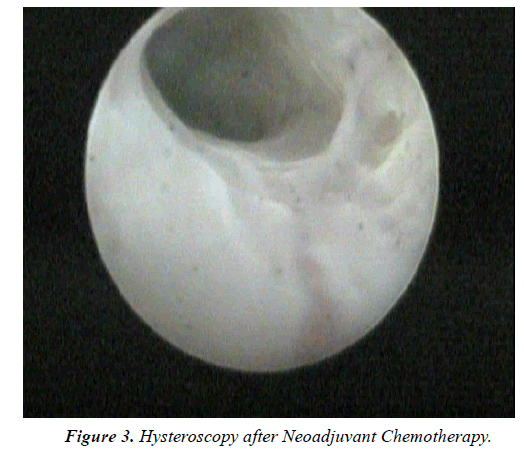
There are a small number of women with cervical cancer stage Ib1, with tumor size between 2-4 cm in diameter (Bulky Ib1), capable of a fertility sparing procedure; however, it is known that exists a higher risk of recurrence when tumor size is over 2 cm [12]. For these cases of bulky Ib1 tumors, neoadjuvant chemotherapy could be an option previous surgical procedure, in order to obtain free pathological margins at the specimen and make possible the surgical procedure (Figure 3).
The objective of this paper is to analyze the long term follow up of the oncologic and fertility results of using Neoadjuvant Chemotherapy followed by abdominal radical trachelectomy (ART), sparing the uterine arteries and the pelvic autonomic plexus (hypogstic plexus), in stages Ib1 with tumor size >2 cm and <4 cm squamous cervical carcinomas.
Materials and Methods
This is a prospective trial over 27 patients submitted to an Abdominal Radical Trachelectomy between 10/04-10/15, in which five cases stages Ib1, with tumor size >2 cm and <4 cm, underwent platinum based Neoadjuvant Chemotherapy prior the surgical procedure.
Condition and inclusion criteria
• Women of child bearing potential wanting to become pregnant (with or without children at the time of diagnosis).
• Tumors staged according to FIGO studies and clinical criteria (1994-2009): Ia2-Ib1 [13].
• In cases of stages Ib1, with tumor size >2 & <4 cm, underwent platinum based Neoadjuvant Chemotherapy.
• Chemotherapy toxicity was measure according the Common Criteria Toxicity system of the Gynecology Oncology Group.
• Ancillary tests:
The tumor size assessment was evaluated by:
- Transvaginal ultrasound;
- magnetic resonance imaging (MRI) and hysteroscopy have been routinely performed as presurgical tests for an adequate tumor size and regional status assessment as well as endocervical involvement, respectively, so as to accurately establish whether the upper section border might be free from disease.
- Pre and postsurgical Color Doppler ultrasound of the uterine arteries, and their myometrial and subendometrial branches.
• Signing of an informed consent.
• Possibility of follow up.
• Patients were included by the intention to treat.
Neoadjuvant chemotherapy was given, according to the following schedule:
Cis-platinum 50 mg/ m2/day 2-3
Paclitaxel 175 mg/ m2/day 1
5-fluororacil (5FU) 800 mg/ m2/day 1-2-3
Four cycles, every 21 days, performing the surgery one month after the last cycle of NCH.
Surgical technique
The Abdominal Radical Trachelectomy was sparing the uterine arteries and hypogastric plexus. No type of cerclage was done as a step of the technique. The surgical procedure was performed always by the same surgical team.
The long term follow up of the oncologic and fertility results as well as the survival rates were analyzed. Survival curves were estimated according to the Kaplan Meier method.
Results
The median age was 27.5 years old.
The average of tumor size was 3.38 cm (2.5-4 cm; SD ± 0.7).
Neoadjuvant chemotherapy
There were observed three complete pathological responses (3/5-60%) and two partial ones >50% (2/5- 40%) of the central tumor (Table 1). The ART could be successfully performed in 4/5 cases. The other procedure was aborted because of an intraoperative metastatic positive lymph node at the anterior parametrium. Neoadjuvant toxicity: Hematologic, grade 1-2; Alopecia, grade 2. MRI and Hysteroscopy confirmed the tumor response after NCH. The postoperative color Doppler of uterine arteries confirmed the blood flow was preserved in all cases.
| Pathological Response To NCH. Central Tumor |
Number of Cases N=5 |
|---|---|
| Complete | 3 (60%) |
| Partial >50% | 2 (40%) |
Table 1. Pathological Response to NCH of Central Tumor.
Pregnancies
Three women got pregnant, one of them, twice. Pregnancies were spontaneously conceived. Three deliveries by cesarean section at 35.5 weeks were done, obtaining 3 healthy newborns. One case of abortion at the ninth week of pregnancy. Neither complications were observed during the prenatal controls nor at and after the surgery. No cases of corioamnionitis, miscarriage or prematurity were registered. No neonatal adverse effects occurred related to the chemotherapy scheme given. So, in summary there were four pregnancies in three women. It is important to point out that, of the whole group underwent an abdominal radical trachelectomy (n=27), the only ones who got pregnant were the cases who received neoadjuvant chemotherapy.
Survival rates
Overall Survival and Disease Free Survival rates were: 100%. Follow-up: 8-72 months. The follow up after births was 8 and 30 months, free of disease. In Table 2 are summarized the results characteristics.
| NCH followed by art | results |
|---|---|
| Population (n) | n=5 CASES |
| Age | 27.5 YEARS OLD |
| Stage | Ib 1 (2-4 cm) |
| Initial Tumor Size | 3,38 cm (-+ 0,7) |
| Neoadjuvant Chemotherapy (Platinum Based) |
YES 4 cycles every 21 days. |
| Type of Surgery Performed (1 month after NCH) |
ART sparing the uterine arteries and hypogastric plexus. |
| Pregnancies Deliveries Abortion Miscarriage Prematurity Corioamninitis |
4 3 ( cesarean sections) 1 0 0 0 |
| Overall survival | 100% |
| Disease free interval | 100% |
| Follow- up | 8-72 months |
| Follow up after births | 8- 30 months |
Table 2. Neoadjuvant chemotherapy (NCH) followed by abdominal radical trachelectomy (ART): summary of results.
Discussion
In the last decades, important efforts have been made in the field of gynecological cancer therapies favoring not only an increase in survival rates but also the preservation of fertility, as clearly shown in the management of endometrial, ovarian and cervical cancer [10,14-16]. It is estimated that in the Americas 68,000 women develop cervical cancer, and that 25,000 women die of the disease each year [17]. In developing countries, such as ours, cervical cancer is one of the most common types of cancer causing death in women. Although statistics in Argentina are not so accurate, a mortality rate of 4.46/100,000 women with some variations related to geographical location and age have been reported. As for women of child bearing potential (until 45 years of age) the rate ranges from 0.4 (20-24 years) to 9.4/100,000 women (40-45 years) [17]. This shows that some patients might need conventional therapies in order to preserve their fertility for many women have postponed pregnancy.
Going back to our case series, we should also point out that teenage pregnancy is an issue in our reality. Therefore, the condition may occur at an earlier age, and it is vital to think about therapeutic options preserving fertility, being the egg cryopreservation another one of them.
There are being described less radical treatments, from conization to radical trachelectomies, as intent of sparing fertility, with similar oncological results than the traditional radical ones [10,12].
Cervical conization is one of the conventional therapies available, but is indicated in stages Ia1 or Ia2, in the absence of lymphovascular space and accompanied by laparoscopic or extraperitoneal lymphadenectomy [18].
Rob et al. [19] reported their experience with conization or simple trachelectomy in stages Ia2-Ib1 under 2 cm using the sentinel node technique and previous laparoscopic lymphadenectomy (7 days) which had to be negative. A larger number of cases and longer follow up may validate this procedure, which seems to be a good therapeutic option. Radical trachelectomy has been performed for more than 15 years. Different authors have supported this technique due to the oncologic and obstetric results obtained [10,12].
The Radical Trachelectomies have been described are: The Vaginal Radical Trachelectomy (VRT) with pelvic lymphadenectomy (Mitra-type extraperitoneal or translaparoscopic procedure); and the Abdominal Radical Trachelectomy (ART). The ARTs may be also performed laparoscopically or with robotics [20].
Vaginal Radical Trachelectomy has been widely reported with more than 600 cases, with a recurrence rate of 4.1% and a death rate of 2.5 % [10,12]. The pregnancy rate after the procedure ranges between 16.7 and 100% [9,10,12,21-24].
Abdominal Radical Trachelectomy derives from the conventional radical hysterectomy performed in cervical cancer patients which allows a good removal of the parametrium with good safety margins. In many centers in the world, the abdominal approach is more widely used for radical procedures. For this reason it is easier to learn and the learning curve is not so long. Moreover, the pregnancy rate after this procedure is lower as compared to the vaginal approach, and ranges between 6.7 and 33% [5-8].
Ungar et al. [8] in their series including 30 abdominal procedures have not reported cases of relapse with an average follow up of 47 months, and report a case of unilateral ureteral lesion as a complication which was conventionally managed without any sequelae.
The technique described by Lazlo Ungar et al. [4] sacrifices the uterine artery from its origin as in the radical hysterectomy, and some authors consider that this may account for the lower obstetric success rate since perfusion after the procedure is uncertain [11].
Klemm at al. showed that after VRT no major changes in the uterine artery resistance index were observed [25].
Wan at al. [11], presented two techniques, in two patients, with the intention of preserving the uterine artery. No major complications have been reported.
We describe our technique, which we consider an adaptation of the C1 radical hysterectomy [26-29] and which allows an adequate resection of the cervix with good lateral and lower margins as shown by the pathology studies, sparing the uterine arteries and the hypogastric plexus. We compared, in other study [30], radicality in our specimens with a historical control group of radical hysterectomies with preservation of the pelvic autonomic plexus. Although we know that historical groups are not the best option for ideal comparisons, at least in our case this was a useful parameter. The comparison showed no significant differences, radicality was perfectly spared, and so was the oncology safety result [30]. So, any ART with nerve sparing, could be also called as C1 radical trachelectomy, although it is not a conventional nomenclature, yet. This in turn would preserve good blood flow and endometrial development, favoring pregnancy and avoiding the autonomic complications of radical hysterectomy [30-35].
Staging, as reported, was based on clinical practices and the FIGO criteria; however, for an adequate case choice, it would be useful to assess the tumor with magnetic resonance imaging, as in some centers [2], in order to get closer to the borders of the lesion and lower the chances of positive superior margins. Also, adding hysteroscopy during the staging phase in these particular cases might be helpful; however, this has not been reported. In fact, we continue thinking it is a useful tool to assess endocervical involvement, as well as upper section border involvement. Moreover, in the patient undergoing neoadjuvant chemotherapy, we were able to assess the response at the level of the endocervix, which changed from complete involvement to an objective response over 50%. Operating time has not become much longer, and blood loss has not increased either as compared to radical hysterectomy.
About pregnancies, it is important to remark, that in the three women who got pregnant; one of them, twice, their pregnancies were spontaneously conceived. Three deliveries by programmed cesarean section at 35.5 weeks were done, obtaining 3 healthy newborns. Neither complications were observed during the prenatal controls nor at and after the surgery. No case of corioamnionitis, miscarriage and prematurity were registered.
Two of these patients had already had children, stated they had not yet fulfilled their fertility, and chose trachelectomy as a therapeutic option. Following this line of thought in relation to less radical therapies, we should underline the role of neoadjuvant chemotherapy, and the response rate obtained, which enabled the performance of this conservative therapy. No neonatal adversal effects were shown associated to the chemotherapy scheme given. The Toxicity was acceptable, grade 2 for allopecia and grade 1-2 for hematologic one.
The overall survival and disease free survival rates were: 100%. Follow-up: 8-72 months. The follow up after births was 8 and 30 months, free of disease.
The results observed, showed us the feasibility and safety related to the oncological and fertility outcomes of the whole treatment strategy, neoadjuvant chemotherapy followed by the abdominal radical trachelectomy technique we used.
These cases, it simply confirms the reports published by Sardi, being the first who introduced the neoadjuvant chemotherapy to the primary treatment for cervical cancer and supported the idea of a possible more conservative surgical procedure for stages Ib1 so they showed to have a significant less rate of local recurrence compared to standart ones for similar stage. It is very important to point out the importance of nodal status, tumor size, lymphovascular space involment and free of disease margins at surgical specimen as high risk prognostic factors. There are a remarkable decreases of them at the pathological findings in rensponder patients to neoadjuvant chemotherapy [36-38].
Around fifteen years after, Sardi´s observations were reconfirmed in two several metaanalisis [39-40].
Landoni et al. [41] and Maneo et al. [42], analyzed the results obtained after neoadjuvant chemotherapy and the possibility of being followed by a less radical surgery in some particular cases. Although these results, we would like to remember, that, in one case of our series, we must abort the strategy of ART because of the presence of a metastatic lymphnode at the anterior parametrium with complete pathological response of the central tumor during the staging laparotomy. So, we think before planning a fertility sparing procedure, it is mandatory a surgical staging and a much better development of the sentinel node detection with ultrastaging and molecular studies, specially to detect a parametrial metastasis, as was mention by Diaz et al. [43].
Lanowska, also reported very good oncological, fertility and neonatal results using neoadjuvant chemotherapy followed by vaginal radical trachelectomy [44]. These results are very similar to our findings, using the abdominal approach for the surgical procedure, in this and previous reports [30]. Robova [45] suggest that patients with microscopic disease after NCH are the best candidates for a fertility sparing procedure.
Pareja et al. [46], in a recent review, showed that fertility preservation rate was 82.7%, 85.1%, 89%; and 91.1% for Abdominal Radical Trachelectomy (ART) (tumors larger than >2 cm), ART (all sizes), Neoadjuvant Chemotherapy followed by surgery and vaginal radical thrachelectomy (VRT) (all sizes); respectively. The global pregnancy rate was 16.2%, 24% and 30.7% for ART, VRT, and NACT followed by surgery; respectively. The recurrence rate was 3.8%, 4.2%, 6%, 7.6% and 17% for ART (all sizes), VRT (all sizes), ART (tumors>2 cm), NACT followed by surgery, and VRT (tumors>2 cm). The author concluded that these outcomes must be considered when offering a fertility sparing technique to patients with a tumor larger than 2 cm.
Plante [47] published that patients underwent neoadjuvant chemotherapy followed by fertility sparing procedure seems to have better fertility and obstetrical outcomes in patients with tumor size between 2-4 cm. In fact, in our series, of the whole group of 27 women summited to an abdominal radical trachelectomy, the only ones that got pregnant were the patients who received neoadjuvant chemotherapy.
So, in accordance with all these evidence, we can conclude that Neoadjuvant Chemotherapy followed by Abdominal Radical Trachelectomy, is obstetrically and oncologically safe. It could be taken into account for selected patients with stages Ib1 with tumors of 2-4 cm in diameter. This report and other publications [48,49] show that more and more conservative management of cervical cancer leads to similar oncology results as radical therapies”. The choice between different fertility preservation techniques should be based on the experience of the team, discussion with the patient or couple, and, above all, objective oncological data to balance the best chance for cure with optimum fertility results for each procedure [49].
References
- http://www.SEER.cancer.gov/statfacts
- Plante M, Renaud M, Francois H, et al. Vaginal radical trachelectomy: An oncologicall safe fertility-preserving surgery. An update series of 72 cases and review of the literature. Gynecol Oncol.2004;94:614-23.
- Dargent D, Brun JL, Roy M, et al. Pregnancy following radical trachelectomy for invasive cervical cancer. Gynecol Oncol.1994;52:105.
- Ungar L, Del Priore G, Boyle DB. Abdominal radical trachelectomy: Follow up of the first 20 cases. Gynecol Oncol. 2002;84:489.
- Smith JR, Boyle DCM, Corless DJ, et al. Abdominal radical trachelectomy: a new surgical technique for the conservative management of cervical carcinoma. Br J Obstet Gynecol.1997;104:1196-200.
- Rodriguez M, Guimares O, Rose PG. Radical abdominal trachelectomy and pelvic lymphadenectomy with uterine conservation and subsequent pregnancy in the treatmet of early invasive cervical cáncer. Am J Obstet Gynecol. 2001;185:370-74.
- Palfalvi L, Ungar L, Boyle DC, et al. Announcement of healthy baby boy born following abdominal radical Trachelectomy. Int J GynecolCancer. 2003;13:250.
- Ungar L, Palfalvi L, Hogg R, et al. Abdominal radical trachelectomy: A fertility preservingoption for women with early cervical cancer. BJOG. 2005;112:366-69.
- Roy M, Plante M. Pregnancy after radical vaginal trachelectomy for early-stage cervical cancer. Am J Obstet Gynecol. 1998;179:1491-96.
- Plante M, Renaud MC, Hoskins I, et al. Vaginal radical trachelectomy: A valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancy and review of the literature. Gynecol Oncol 2005;98:3-10.
- Wan X, Yan Q, Xi X, et al. Abdominal radical trachelectomy: two new surgical techniques for the conservation of uterine arteries. Int J Gynecol cancer 2006;16:1698-1704.
- Coskum Salman M, Ozgul N, Yce K. Widespread recurrence 7 years after radical abdominal trachelectomyfor early cervical adenocarcinoma. Case Rep Obstetr Gynecol. 2015:517496.
- Pecorelli S. FIGO Committee on Gynecologic Oncology. A Revised Staging for carcinoma of the vulva, cervix and endometrium. Int J Gynecol Obstet. 2009;105:103-4.
- Plante M. Fertility preservation in the management of the gynecological cancer. Curr Opin Oncol. 2000;12:497-507.
- Renaud MC,Plante M, Roy M. Fertility preservation in the management of endometrial cancer. CME J Gynecol Oncol.2003;8:121-7.
- Morice P, Camatte S, Wicart-Poque F, et al. Fertility preservation in the management of epithelial ovarian cancer. CME J Gynecol Oncol. 2003;8:107-16.
- Rocc D. Uterus cancer mortalityin Argentina.http://www.msal.gov.ar/htm/site/pdf/mortalidad.cancer.utero12.pdf
- Benedet JI, Hacker NF, Ngan HYS. Staging classifications and clinical practice guidelines of gynecologic cancer FIGO Committee on Gynecologic Oncology and IGSC Guidelines Committee. Second edition. November 2003.
- Rob L, Charvat M, Robova H, et al. Less radical fertility-sparing surgery than radical trachelectomy in early cervical cancer. Int J Gynecol Cancer. 2007;17:304-10.
- Clinical Guidelines for diagnosis, treatment and monitoring of female genital cancer. 2nd Edition. Argentine Association of Gynecologic Oncology 2013.
- Shepherd JH, Mould T, Oram DH. Radical trachelectomy inearly stage carcinoma of cervix: outcome as judged by recurrence and fertility rates. BJOG. 2001;108:882-85.
- Burnett AF, Roman LD, O MearaAT, et al. Radical vaginal trachelectomy and pelvic linphadenectomy for preservation of fertility in early cervical carcinoma. Gynecol Oncol. 2003;88:419-23.
- Schlaerth JB, Spirtos NM, Schaerth AC. Radical trachelectpmy and pelvic linphadenectomy with uterine preservation in the treatment of cervical cancer. Am J Obstet Gynecol.2003;188:29-34.
- Covens A, Shaw P, Murphy J, et al. Is radical trachelectomy a safe alternative for patients whit stage IA-B carcinoma of the cervix? Cancer.1999;86:2273-79.
- Klemm P, Tozzi R, Kfhler C, et al. Does radical trachelectomy influence uterine blood supply? Gynecol Oncol,2005;96:283-6.
- Cibula D, Abu Rustum NR, Benedetti-Panici P, et al. New classification system of radical hysterectomy: An Emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol Oncol. 2011;122:264-8.
- Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9:297-303.
- Soderini AH. Is the nerve sparinga new standard in radical hysterectomy (NSRH) for cervical cancer (CC)? International Gynecological Cancer Society 12th Biennial Meeting; October 25, 2008; Bangkok, Thailand.
- Soderini AH, Cuneo NA, Aragona AM. Nerve-sparing radical surgery in cervical cancer. Colposcopía. 2010;21:80-85.
- Soderini A, Aragona A, Bonavía E, etal. The abdominal radical trachelectomy sparing the uterine arteries (a.r.t.- s.u.a) & the pelvic autonomic plexus (p.p.a.p.) in cervical cancer (cc): oncological & fertility outcomes of this novel surgical technique: IGCS-0105 Cervical Cancer. Int J Gynecol Cancer. 2015;25:40-1.
- Soderini AH. Final results of the pelvic nerve-sparing hysterectomy. Ph.D. Thesis, University of Buenos Aires. October 2012.
- Soderini AH, Sardi J, Giaroli A, et al. Nerve sparing radical hysterectomy for cervical cancer. Preliminary results. Int. J. Gynecol Cancer. 2006;16:695-763.
- Trimbos JB, Maas CP, Deruiter MC, et al. A nerve-sparing radical hysterectomy : guidelines and feasibility in Western patients.Int. J. Gynecol Cancer. 2001;11:180-86.
- Hoeckel M, Horn LC, Hentschel B, et al. Total mesometrial resection: high resolution nerve-sparing radical hysterectomy based on developmentally defined surgical anatomy. Int J Gynecol Cancer. 2003;13:791-803.
- Abu-Rustum N, Sonoda Y, Black D, et al. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma: A Technique and review of the literature. Gynecol Oncol. 2006;103:807–13.
- Sardi J, Giaroli A, Sananes C, et al. Is subradical Treatment for carcinoma of the cervix logical? Gynecol Oncol. 1989;32:360-64.
- Ferreyra M, Soderini AH, Sardi J, et al. Subradical treatment for carcinoma of the cervix Ib, dogma or utopia?. European School of Oncology in the First Latin-American Educational Convention. Buenos Aires, November 12-14,1995.
- Sardi J, Giaroli A, Sananes C, et al. Long term follow up of the first randomized trial using neoadjuvant chemotherapy in squamous carcinoma of the cervix: the final results. Gynecol Oncol. 1997;67:61-9.
- Rydzewska L, Tierney J, Vale CL, et al. Neoadjuvant chemotherapy plus surgery vs surgery for cervical cancer. Cochrane Database Syst Rev.2012;12:CD007406.
- Kim HS, Sardi JE, Katsumata N, et al. Efficacy of neoadjuvant chemotherapy in patients with FIGO stage IB1 to IIA cervical cancer: an international collaborative meta-analysis. Eur J Surg Oncol. 2013;39:115-24.
- Landoni F, Parma G, Peiretti M, et al. Chemo-conization in early cervical cancer. Gynecol Oncol. 2007;107:125-6.
- Maneo A, Chiari S, Bonazzi C, et al. Neoadjuvant chemotherapy and conservative surgery for stage IB1 cervical cancer. Gynecol Oncol. 2008;111:438-43.
- DiazJ, BarakatR,Abu RustumN, et al. Parametrial Metastasis: a cause of false- negative sentinel lymph node mapping in early stage cervical carcinoma. Gynecol Oncol.2010;116:41.
- Lanowska M, Mangler M, Speiser D, et al. Radical vaginal trachelectomy after laparoscopic staging and neoadjuvant chemotherapy in women with early-stage cervical cancer over 2 cm: oncologic fertility, and neonatal outcome in a series of 20 patients. Int J Gynecol Cancer. 2014;24:586-93.
- Robova H, Rob L, Halaska MJ, et al. Review of neoadjuvant chemotherapy and trachelectomy: which cervical cancer patients would be suitable for neoadjuvant chemotherapy followed by fertility-sparing surgery? Curr Oncol Rep. 2015;17:446.
- Pareja R, Rendón GJ, Vasquez M, et al. Immediate radical trachelectomy versus neoadjuvant chemotherapy followed by conservative surgery for patients with stage IB1 cervical cancer with tumors 2cm or larger: A literature review and analysis of oncological and obstetrical outcomes. Gynecol Oncol. 2015;137:574-80.
- BulkyPM. Early-Stage Cervical Cancer (2-4 cm Lesions): Upfront Radical Trachelectomy or Neoadjuvant Chemotherapy Followed by Fertility-Preserving Surgery: Which Is the Best Option? Int J Gynecol Cancer. 2015;25:722-8.
- Festi A, Landoni F. Chemo-conization for early stage cervical cancer. Textbook of Gynaecological Oncology, Gunes Publishing, 2011;530-536.
- Bentivegna E, Gouy S, Maulard A, et al. Oncological outcomes after fertility-sparing surgery for cervical cancer: a systematic review. Lancet Oncol. 2016;17:e240-53.