Case Report - Journal of Clinical Ophthalmology (2021) New Insights in Ophthalmology
Management of juvenile uveitis in juvenile idiopathic arthritis: A Hungarian approach.
Alok Bahl1*, Lilla Smeller2, Sohár Nicolette2
1Royal Eye Infirmary, University Hospitals Plymouth NHS Foundation Trust, Plymouth, United Kingdom
2Department of Ophthalmology, University of Szeged, Hungary
- Corresponding Author:
- Dr. Alok Bahl
Royal Eye Infirmary
University Hospitals Plymouth
NHS Foundation Trust
Plymouth
United Kingdom
E-mail: alok.bahl@nhs.net
Accepted date: 15 February, 2021
Citation: Bahl A, Smeller L, Nicollete S. Management of juvenile uveitis in juvenile idiopathic arthritis: A Hungarian approach. J Clin Ophthalmol 2021;5(S2):347-349.
Abstract
The Ophthalmology department at the University of Szeged in Hungary is one of few tertiary centers in the country that takes on complicated cases of juvenile uveitis. Delayed initial presentation combined with confirmed systemic diseases makes cases more complicated to manage and treat. A thorough medical history is vital to help focus investigations. This therefore, involves a multidisciplinary team approach to the management of these complicated cases. Furthermore, good communication with families (parents) is key in establishing a strong bond and helps increase rates of compliance with medications especially in socio- economically challenged communities. This case provides an in-depth analysis of the management of juvenile uveitis.
Keywords
Juvenile uveitis, Idiopathic arthritis, Intraocular pressure, Optical Coherence Tomography (OCT).
Background
This case helps reiterate the importance of good communication skills and the issue of compliance with medication and provides a step by step approach to the options available in managing complicated juvenile uveitis.
Case Presentation
A young teenage boy presented with redness in both eyes and associated pain with worsening vision in his left eye. He had been seen by an ophthalmologist in his village and was diagnosed to have severe anterior uveitis. He was started on intravenous dexamethasone (due to systemic involvement, joint swelling and pain) with an initial dose of 1 milligram/kilogram of body weight for 3 days after which he was given steroid tablets at tapering doses due to worry of adverse systemic side effects. His steroid tablets were started at 16 milligrams per day which was tapered to 8 milligrams for 3 days and tapered again to 4 milligrams. He was referred to the uveitis outpatient clinic in Szeged after his ocular signs and symptoms became worse.
At the tertiary center initially on examination with slit lamp and 90 Dioptre funduscopic mirror we noted snow banking inferiorly with the presence of inflammatory cells in the vitreous of the left eye whilst the right eye was normal.
These inflammatory cells (snowflakes) appeared to be white in colour and round in shape. The intraocular pressure (IOP) was normal in both eyes and there was no evidence of cataract formation. His visual acuity in the right eye was 1.0 and 0.6 in the left eye using logmar chart.
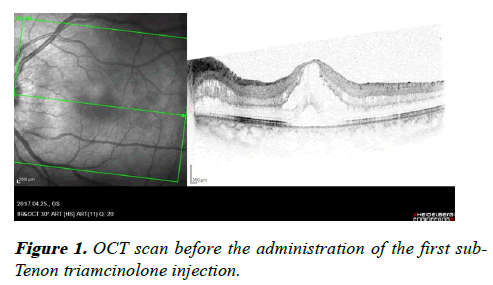
On Optical Coherence Tomography (OCT) scan, there was evidence of cystoid macular oedema (CMO) as shown in Figure 1 where there were a number of cyst-like areas filled with fluid in the left eye only. The central retinal thickness was 729 micrometres. Due to the presence of CMO, it was decided to administer a sub–Tenon Triamcinolone injection. Also, at this time his blood report showed an increased C- reactive protein value of 9.5 mg/l and an increased erythrocyte sedimentation rate of 34 mm/h with slightly reactive lymphocytosis.
After an initial examination, he was also referred to a paediatric-rheumatologist in order to find any systemic cause for the uveitis. The rheumatologist started him on methotrexate (20 mg/week) which is the first line choice of immunosuppressant drug as the uveitis was not responding to the previous trialed steroids.
Past medical history – Nil
Social history – lives with parents, non-smoker and at secondary school.
Family history – Nil of note to contribute in relation to genetically passed on conditions.
Investigations
Blood tests that included autoimmune screen, full blood count, kidney function test, liver function test, bone profile test, C reactive protein and Erythrocyte sedimentation rate. OCT scans at regular intervals to assess the effect of the injected medication. Chest X ray to rule out other systemic causes of juvenile uveitis – e.g. sarcoidosis
Differential diagnosis
Recurrent episodes of uveitis indicate a need to rule out causes like JIA, sarcoidosis, ocular toxoplasmosis, ocular tuberculosis, toxocariasis, Lyme disease and sympathetic ophthalmia [1].
Outcome and follow-up
3 months from the first injection, on examination, there was slight opacification of the lens along with the snowballing and snow banking seen inferiorly in the left eye. It was also noted that he started having systemic symptoms like pain in the fingers and pain in the muscles of the thigh. His dexterity had worsened and so did his performance in school and was diagnosed with JIA. In June 2017, a follow up OCT scan of the left eye showed increased central retinal thickness at a value of 842 micrometres with evidence of progressing CMO which therefore, warranted the use of a second sub-Tenon triamcinolone injection.
This result was considered an inadequate response after viewing post injection OCT and he was therefore, advised to receive a third sub-Tenon triamcinolone injection after which his follow up OCT was much improved with minimal CMO.
He received a total of 3 injections of sub-Tenon triamcinolone, an OCT scan showed a good outcome. Methotrexate 20 mg/ week was being taken to control the inflammation. His liver functions were monitored due to the hepatotoxic effect of methotrexate.
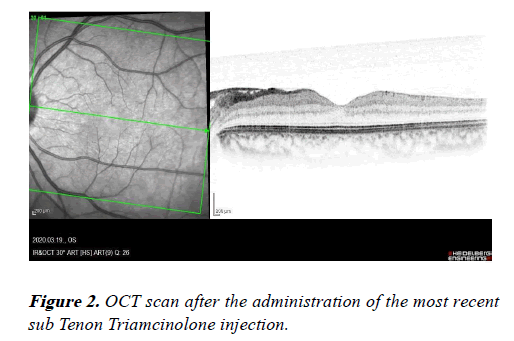
Two years on, OCT shows a significant amount of CMO and after a detailed conversation with the patient and his parents, the patient mentioned he did not think he needed to continue taking (also did not want to take) the methotrexate as he thought “he was cured”. He also developed a cataract and underwent phacoemulsification and implantation of an intraocular lens in the left eye. He received a further sub-Tenon Triamcinolone injection with a great response as seen in Figure 2, and was recommenced on 20 mg of methotrexate. He is now continued to be followed up on a regular basis.
Discussion
The importance of detailed history taking cannot be emphasised enough in uveitic cases especially in children. The Massachusetts Eye Research and Surgery Institution developed an Ocular Inflammatory Disease Review of Systems Questionnaire [2] includes detailed family history, social history, ocular and systemic medications and allergies, past medical and surgical history. There is a long list of systemic symptoms to help diagnose specific diseases associated with uveitis [3]. The duration, onset and course of the inflammation, the location of the inflammatory process with detailed clinical examination of the eyes and body, help in differential diagnosis and requesting for specific investigations.
In certain cases of known diagnosis like JIA, children do not have any ocular symptoms. In these cases, screening plays an important role.
The most common cause of uveitis in children is JIA. In 73% of these cases considered at risk, uveitis occurs within the first year of the onset of arthritis and could be the first sign of JIA [4]. Despite remarkable progress in the early detection and treatment of inflammation, vision-threatening complications of uveitis still occur in a vast majority of patients [5]. This emphasises the need for regular ophthalmic screening and paediatricians and rheumatologists should be reminded to send such cases to the ophthalmologist.
The most common treatment option for anterior uveitis is a tapering course of topical dexamethasone 0.1% drops, with mydriatics, and occasionally subconjunctival steroid when required based on clinical judgement.
Complications are more often seen in delayed presentations. Early diagnosis and prompt initiation of treatment to achieve complete quiescence is the mainstay of management of juvenile uveitis patients for prevention of sight threatening complications [6].
Due to the lack of treatment or in cases of inadequate treatment certain complications can include formation of, cataract (40-80%), band keratopathy (30-80%), CMO (30- 50% in chronic cases), vitreous haze/debris (20-30%), glaucoma (10-30%), chronic hypotony and phthisis (5-20%) and other posterior pole complications (e.g. disc neovascularization, macular hole) that are rare [3].
Complications from treatment of the uveitis may include ocular complications like cataracts, keratitis, and steroid- induced glaucoma from topical steroids, whereas regional corticosteroids cause complications like lid abnormalities, orbital socket contraction, and globe perforation [7].
Treatment complications may also include certain systemic complications like gastrointestinal bleeding from the use of non-steroidal anti-inflammatory drugs, growth retardation, weight gain, acne, mood swings, and infections from systemic corticosteroids. Immunosuppressive therapy with the use of methotrexate, cyclosporine- A, cyclophosphamide, chlorambucil can lead to certain dangerous complications, for example bone marrow suppression and pancytopenia [3].
Learning Points
• Uveitis is the first sign of many systemic diseases and needs to be investigated
• A detailed history, thorough examination and a multidisciplinary approach with good communication skills is vital to help achieve the best possible outcome
• Follow up patients on a regular basis to check on disease process. This provides reassurance and positive feedback to yourself and the patient.
References
- Foster CS: Pediatric Uveitis. The Ocular Immunology and Uveitis Foundation. 2017.
- The Ocular Immunology and uveitis foundation.
- Roque M. Juvenile Idiopathic Arthritis Uveitis. Medscape. 2016.
- Rodríguez-GarcíaA. The importance of an ophthalmologic examination in patients with juvenile idiopathic arthritis. Reumatol Clin.2015;11:133-8.
- Samra KA, Maghsoudlou A, Roohipoor R, et al. Current treatment modalities of jia-associated uveitis and its complications: literature review. Ocul Immunol Inflamm. 2016;24:431-9.
- Majumder PD, Biswas J. Pediatric uveitis: An update. Oman J Ophthalmol. 2013;6:140-50.
- Kanski J, Bowling B. Clinical Ophthalmology: A systematic approach. 7th edition. ElsevierSaunders. Edinburgh, 2011.