Research Article - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 4
Macular hole surgery with silicone oil as a tamponade
Carl-Ludwig Schönfeld*, Linda Maren Meyer, Thomas Klink, Christos Haritoglou
Department of Ophthalmology, Eyeclinic Herzog Carl-Theodor, München, Germany
- Corresponding Author:
- Prof. Dr. Carl-Ludwig Schönfeld
Department of Ophthalmology
Eyeclinic Herzog Carl-Theodor
München
Germany
E-mail: cb.schoenfeld@gmx.net
Accepted date: 19 June, 2021
Citation: Schönfeld CL, Meyer LM, Klink T, et al. Macular hole surgery with silicone oil as a tamponade. J Clin Ophthalmol 2021;5(4):425-430.
Abstract
Purpose: Pars plana vitrectomy (PPV) with gas endotamponade is the gold standard for the surgical treatment of macular holes. An alternative may be an endotamponade with silicone oil (SiO) which does not require postoperative prone posture.
Methods: 56 patients/57 eyes with macular holes (diameter 94-932 μm) underwent a primary PPV with SiO endotamponade or a secondary SiO after failure of a previous intervention. Endpoints were closure of macular hole and best corrected visual acuity (BCVA) measured by means of logMAR.
Results: Closure of macular holes was achieved in 50 eyes (87.7%), 90.0% in primary and 82.4% in secondary SiO. LogMAR improved in 82.5% of primary and 76.5% of secondary SiO. Mean postoperative logMAR decreased significantly both in the whole group and in the two subgroups. In total, the mean factor of BCVA improvement was 2.63 ± 2.57, and it did not differ significantly between primary and secondary SiO (3.09 ± 2.51 vs. 1.82 ± 2.40).
Conclusion: PPV with SiO endotamponade for the treatment of macular holes achieves very good results with regard to the anatomical closure and VA. SiO is not only an alternative for elderly or comorbid patients where postoperative prone posture is impossible, but also in recurrent cases or large macular holes avoiding manipulation under the retina.
Keywords
Macular hole, Retinal surgery, Vitreous surgery, Silicone oil.
Introduction
Since the early 1990s it is possible to close macular holes surgically [1], and up to now several surgical techniques have been developed and refined to improve functional and anatomical results. Today the gold standard includes transconjunctival sutureless pars plana vitrectomy (PPV), peeling of the internal limiting membrane (ILM) using dyes such as trypan blue, brilliant blue or indocyanine green followed by gas tamponade and prone positioning of the patient after surgery [2]. The gas endotamponade substitutes the vitreous, and its surface tension helps to approximate the edges of the macular hole resulting in a complete closure [3,4].
In general, gas endotamponades used for the treatment of macular holes include sterile air, 16% perfluoroethane (C2F6), 14% perfluoropropane (C3F8), and 20% sulfur hexafluoride (SF6) with closure rates of up to 93% [5-7]. Due to their very low specific gravity and high buoyancy, gases fulfil their function in macular hole surgery best if the patient spends at least the first postoperative week in prone position to ensure a permanent contact of the gas bubble to the macular hole [2,8,9].
However, macular hole surgery with gas tamponade has some drawbacks. Several studies demonstrated that macular holes also may close without prone positioning. A significant benefit of face-down posturing was reported for large macular holes ≥ 400 μm, but not for smaller macular holes [10]. A lot of patients with macular holes are 60 years and older and unable to maintain prone position because of medical or functional restrictions [11]. Even patients without such limitations often poorly tolerate the prone position, and their adherence is therefore compromised [12]. Another argument against gas endotamponade is its contraindication in forthcoming air travel [11]. In these cases, oil tamponade may represent an alternative to gas tamponade.
In addition to these limitations, less favorable surgical outcome using gas tamponade is achieved in the treatment of naïve larger holes of >400 μm and especially in persistent macular holes where the ILM has already been removed around the hole. New surgical techniques, such as several variations of the ILM flap technique for large macular holes, have been developed to improve anatomic results for these cases [13]. In persistent large macular holes, where the ILM has already been removed during the first operation, implantation of retinal grafts, amniotic membrane, lens capsule, or pieces of peripheral ILM into the hole have been suggested [14-16]. Very recently it has been suggested to inject BSS (balanced salt solution) under the retina at the posterior pole around the macular hole in order to allow for a better attenuation of the macular hole in selected cases [17]. However, these interventions require surgical skill and a great deal of experience. It is also unknown how implanted grafts will integrate at the macular hole area, to what extent the retina may remodel, and how the RPE (retinal pigment epithel) may be altered. While anatomic results of these techniques are promising, it still remains unclear to which extent function will be restored. Therefore, we hypothesize that the use of silicone oil as a tamponade may still be a valuable alternative technique without excessive manipulation around or under the macular hole in persistent or large macular holes.
The tamponade effect of silicone oil is based on its surface tension and buoyancy due to its specific gravity and polarity.
The tamponade effect is caused by the direct contact between oil and retina [18], with the oil sealing the macular hole and preventing further fluid efflux into the subretinal space. Therefore, the oil-fill of vitreous cavity must be as complete as possible [19]. Besides the fact that this surgery requires far less manipulation in the macular hole area, silicone oil also is of advantage since patients do not have to keep prone positioning postoperatively.
“Elder” surgical techniques tend to be forgotten in times when new surgical approaches are investigated and promoted. Given this background and to reappraise macular hole surgery with silicone oil tamponade, we conducted the present retrospective study using silicone oil in small, large and persistent macular holes.
Materials and Methods
In this retrospective cohort study, we analyzed data of patients with macular holes who had undergone pars plana vitrectomy (PPV) and silicone oil endotamponade at the Herzog Carl- Theodor Eye Hospital, Munich, Germany, between 2012-2017 with a minimum follow-up of 6 months. The study was conducted according to the tenets of the Declaration of Helsinki and IRB approval was obtained.
We excluded patients with preexisting ocular diseases prone to influence the surgical outcome, ocular trauma and ocular surgery except for cataract surgery and an unsuccessful former attempt to close a macular hole.
Subgroup analysis differentiated between patients with primary silicone oil tamponade or secondary silicone oil tamponade after failure of a previous surgical approach with gas endotamponade (persistent macular hole). We conducted a standard 23 gauge vitrectomy with ILM peeling and endotamponade of silicone oil (Siluron® 5000, Geuder, Heidelberg/Germany).
The charts of all patients were retrospectively reviewed. We documented age, gender, macular hole diameter measured at the minimum aperture, and best-corrected visual acuity (BCVA) for our analysis. As for BCVA measurement, we met the demands of Elliot (2016): ETDRS chart scored by-letter, luminance 160 cd m-2, distance 6 m, VA with a subjective refraction result, termination if the patients made three or more errors in a line of 5 letters [20]. BCVA values were converted to the logarithm of the minimum angle of resolution equivalent (logMAR) for statistical analysis.
Final postoperative VA was measured at the last follow-up after oil-removal. The factor of improvement was calculated according to the formula 10logMARpost-logMARpre.
Statistical analysis was performed using SPSS software (version 22.0, SPSS, Chicago, Ill., USA). We computed mean value, standard deviation (SD) and range for continuous variables, and the frequency of counts and percentage for categorial data. Subgroup comparisons were analyzed by Student’s t-test and Pearson’s chi-squared test with a significance level of 0.05 and a confidence coefficient of 0.95.
Results
Total sample analysis
We included 56 patients (57 eyes) aged from 50 to 89 years (71.5 ± 7.9 years [average ± standard deviation]), among them 38 women (67.8%) and 18 men (32.2%). Follow-up ranged from 6 months to 7 years (5.2 ± 1.8 years).
The diameter of macular holes varied between 94 μm and 932 μm with a mean value of 424.2 ± 176.4 μm. According to the minimum hole diameter, 30 holes (52.6%) were categorized as large (>400 μm), 16 (28.1%) as medium (250-400 μm) and 11 (19.3%) as small (<250 μm). A closure of macular hole was achieved in 50 eyes (87.7%) while the macular hole remained unclosed in 7 eyes (12.2%).
An improvement of BCVA was achieved in 46 out of 57 eyes (80.7%), while it remained unchanged in 5 eyes (8.8%) and worsened in 6 eyes (10.5%).
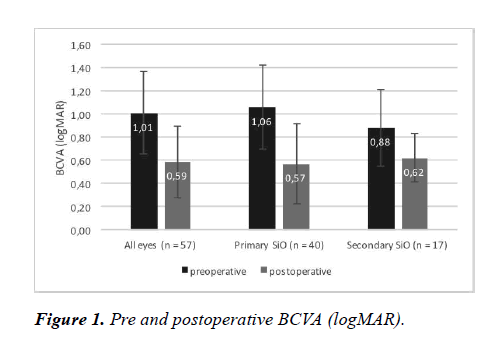
Across all eyes, logMAR improved from 1.01 ± 0.36 before surgery to 0.59 ± 0.31 postoperatively (p<0.001). This corresponds to an improvement of 2.63 times.
Primary vs. secondary silicone oil endotamponade
A primary PPV with silicone oil endotamponade (“primary SiO”) was conducted in 40 eyes (70.2%), among them 7 eyes from 6 patients who had refused prone position. In 17 out of 57 eyes (29.8%) vitrectomy with silicone oil endotamponade was conducted following an unsuccessful attempt by means of a gas endotamponade (“secondary SiO”). The subgroups did not differ in respect of the baseline parameters (Table 1) with the exception of age.
| Primary SiO | Secondary SiO | p | |
|---|---|---|---|
| (n=39 pts/40 eyes) | (n=17 pts/eyes) | ||
| Age (years) | 73.2± 7.0 | 67.4±8.4 | 0.01 |
| (52-89) | (50-78) | ||
| Gender | 27 female (69.2%) | 11 female (64.7%) | n.s. |
| 12 male (30.8%) | 6 male (35.3%) | ||
| Indication: Positioning | 7 (17.9%) | 2 (11.8%) | n.s. |
| Hole size category | n.s. | ||
| large (>400µm) | 22 (55.0%) | 8 (47.2%) | |
| medium (250-399µm) | 11 (27.5%) | 5 (29.4%) | |
| small (<250µm) | 7 (17.5%) | 4 (23.4%) | |
| Diameter of | 434.6±179.1 | 399.9±167.2 | n.s. |
| macular hole (µm) | (172-932) | (94-709) | |
| BCVA – preoperative (logMAR) | 1.06±0.36 | 0.88± 0.33 | n.s. |
| (range) | (0.3± 2.0) | (0.3-1.3) | |
*n.s.=not significant; pts=patients; SiO=silicone oil
Table 1: Basic data of patients with primary or secondary silicone oil endotamponade.
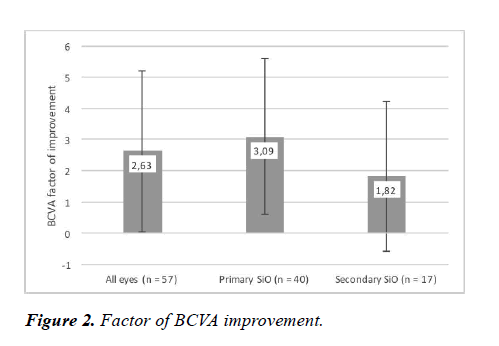
The visual acuity improved in 82.5% of eyes with primary SiO and in 76.5% of eyes with secondary SiO (p>0.05). BCVA improvement was statistically significant in both subgroups: It decreased from 0.12 ± 0.12 logMAR units to 0.34 ± 0.12 logMAR units in the primary SiO group (p<0.001) and from 0.18 ± 0.15 logMAR units to 0.29 ± 0.16 logMAR units in the secondary SiO group (p<0.001) (Table 2 and Figure 1). These results correspond to a factor of BCVA improvement of 3.09 ± 2.51 in eyes with primary silicone oil application and 1.82 ± 2.40 in eyes with secondary silicone oil application (p=0.07) (Table 3 and Figure 2).
| Preoperative | Postoperative | p | |
|---|---|---|---|
| BCVA (logMAR) | |||
| All (n=57) | 1.01±0.36 | 0.59±0.31 | <0.001 |
| Primary SiO (n=40) | 1.06±0.36 | 0.57±0.35 | <0.001 |
| Secondary SiO (n=17) | 0.88± 0.33 | 0.62± 0.21 | 0.007 |
Table 2: Pre and postoperative BCVA in all eyes and in eyes with primary or secondary SiO.
| All (n=57) | Primary SiO (n=40) | Secondary SiO(n=17) | p (primary vs. secondary) | |
|---|---|---|---|---|
| Change of visual acuity | ||||
| improved | 46 (80.7%) | 33 (82.5%) | 13 (76.5%) | n.s. |
| unchanged | 5 (8.8%) | 4 (10.0%) | 1 (5.9%) | |
| worsened | 6 (10.5%) | 3 (7.5%) | 3 (17.6%) | |
| Factor of BCVA improvement | 2.63±2.57 | 3.09±2.51 | 1.82±2.40 | 0.07 |
*n.s.: not significant
Table 3. Categorical changes in BCVA and factor of BCVA improvement in all eyes and in eyes with primary or secondary SiO.
Closure of macular holes
The closure of macular holes was successfully achieved in 36 out of 40 (90.0%) eyes with primary and 14 out of 17 eyes (82.4%) eyes with secondary SiO.
The total of seven patients with non-closure of their macular holes included 4 women and 3 men, aged 77.9 ± 5.8 years (Table 4). Four of them underwent a primary and three a secondary silicone oil endotamponade. The size of the seven unclosed holes comprised all size categories in both subgroups.
| Age | Gender | Primary/Secondary | Diameter (µm) | Size | logMAR preoperative | logMAR postoperative | |
|---|---|---|---|---|---|---|---|
| 1 | 79 | female | primary | 685 | large | 1 | 1 |
| 2 | 72 | male | primary | 270 | medium | 0.7 | 1 |
| 3 | 89 | female | primary | 262 | medium | 0.3 | 0.4 |
| 4 | 82 | male | primary | 217 | small | 0.5 | 1 |
| 5 | 77 | male | secondary | 692 | large | 0.4 | 0.7 |
| 6 | 71 | female | secondary | 468 | large | 0.3 | 0.5 |
| 7 | 75 | female | secondary | 94 | small | 0.3 | 0.7 |
| MW | 77.9 | 384 | 0.5 | 0.76 | |||
| SD | 5.8 | 217.9 | 0.24 | 0.23 |
Table 4: Patients without closure of their macular hole.
Discussion
The current gold standard for the treatment of a macular hole is transconjunctival sutureless pars plana vitrectomy (PPV) with peeling of the ILM followed by gas endotamponade and prone positioning for most cases. Using this technique closure rate of more than 90% can be achieved. Its major disadvantage is the demand for a face-down positioning postoperatively, which may represent a challenge for elderly or handicapped patients [12].
The anatomical and functional results of the aforementioned current standard of care are especially limited in large holes greater than 400 μm measured at the minimum aperture and persistent macular holes. Therefore, in order to improve surgical success in large and persistent macular holes, modifications of the standard surgical technique have been a subject of investigation. Very recently new surgical approaches have been published [14-16], including the positioning of autologous material such as retinal tissue, lens capsule or ILM inside or under the macular hole aperture or rim. Alternatively, subretinal BSS injection was recently published as an alternative method to mobilize retinal tissue at the posterior pole and allow for an attenuation of large macular holes [17]. However, while anatomical results appear promising, there is little knowledge on how tissue transplants inside or under the hole will integrate, whether there will be RPE alterations seen in the postoperative course, and how function will develop.
The endotamponade with silicone oil may offer an alternative, because there is not only no need for a postoperative facedown posture, but even more importantly the use of silicone oil avoids excessive manipulation in the macular hole area, except maybe for a careful aspiration using a soft tipped needle. A known drawback of silicone oil tamponade is the need for a secondary surgery for oil removal. In addition, its efficacy and safety are still being discussed [11,21-24].
Given this background, we conducted the present study to investigate the functional and anatomic results of macular hole surgery using silicone oil as a tamponade (5.000 centistokes [cst]) in 56 patients/57 eyes with a macular hole. Patients were mostly elderly (mean age of 71.5 ± 7.9 years) with a predominance of females (67%) similar to previous publications [25]. Higher age and comorbidities were reasons for the choice of an endotamponade with silicone oil, which is reflected by the fact that our patients with a primary silicone oil endotamponade were significantly older than patients in whom silicone oil was used in secondary surgeries (73.2 ± 7.0 years vs. 67.4 ± 8.4 years; p=0.01). Additionally, nine of 56 patients (16.1%) had refused to a gas endotamponade explicitly because they feared postoperative prone position. We included macular holes of all sizes from 94 μm up to 932 μm, which is reflected by the large range of function before surgery.
In 40 eyes of 39 patients the PPV with silicone oil was conducted as first intervention to close the macular hole and an anatomical closure was achieved in 36 eyes (90.0%). In a comparable study, Pertile and Claes reported on 35 eyes with macular holes stage 3-4, which were treated by means of PPV and peeling of ILM with silicone oil tamponade, and observed a higher closure rate of 97.1% [24]. Stalmans et al. compared 5.000 vs. 1.000 cst silicone oil (n=36 eyes each) as an endotamponade and even reported a closure rate of 100% [26]. In other studies, the closure rates covered a range from 65-100% [11,19,21-23]. Therefore, the closure rate of 90% as observed in our series is quite in line with the published literature and comparable to other studies [11,23,24].
The closure rate in our 17 patients who underwent a secondary surgery using silicone oil as a tamponade following failed gas endotamponade was slightly lower (14 out of 17 eyes, 82.4%) compared to the aforementioned group. Previously reported results of anatomical closure following reoperation with gas tamponade varied in a similar range from 73%-91% [27].
In total, we could not achieve a closure of the macular hole in 7 eyes; there were no correlations to age, gender, primary/ secondary SiO, or hole diameter/hole size. Our results indicate that the use of silicone oil in macular hole surgery is not disadvantageous for the patient compared to surgery using a gas endotamonade both for primary and secondary cases and appears beneficial for a great spectrum of macular hole sizes.
Successful closure of the macular hole is a prerequisite but not a guarantee for improved visual acuity [11,28,29]. In our series of macular hole surgery with silicone oil endotamponade, the visual acuity improved in 82.5%, remained unchanged in 10.0%, and worsened in 7.5% of primaryly treated eyes. The mean value of best corrected visual acuity decreased from 1.01 ± 0.36 logMAR units preoperatively to 0.59 ± 0.31 logMAR units postoperatively (p<0.001), corresponding to a factor of improvement of 2.63 ± 2.57.
The functional results of other studies on silicone oil endotamponade are variable and partially contradictory. Karia et al. observed any improvement in visual acuity only in 38% of their patients [30], while in the study of Goldbaum et al. the logMAR value of visual acuity improved by an average of 0.26 to 0.61 (20/81) [19]. Similar results were obtained by Ivanovska-Adjievska et al. who found a mean BCVA improvement from 0.6 logMAR units to 0.8 logMAR units and a significant reduction of metamorphopsia in all patients [31]. Two-armed studies comparing gas versus silicone oil often favorized gas endotamponade. Lai et al. reported that the final median visual acuity for the gas group was significantly better than for the oil group (20/50 vs. 20/70; p=0.047) [21]. Similar results were obtained by Tafoya et al. who saw improvements in visual acuity more frequently in eyes treated with gas endotamponade than following silicone oil endotamponade [23]. In another study visual acuity improved to 20/70 or better in only 17.3% eyes of the SiO group but in 73.0% eyes of the gas group [11]. In contrast, Pertile and Claes observed an excellent recovery of visual acuity up to 1.0 more frequently in the group treated with silicone oil tamponade. A visual acuity of 0.4 or better was seen in 74% of eyes in the SiO group, but only in 47% of eyes in the gas group (p=0,0217) [24].
In our series there were no significant differences in postoperative function comparing primary versus secondary surgery: The mean factor of BCVA improvement was 3.09 ± 2.52 in our primary and 1.82 ± 2.40 in our secondary treated eyes (p=0.07). A greater difference was observed by Kumar et al. who found a mean visual improvement of 0.41 logMAR units in primary and disappointing 0.03 logMAR units in secondary cases [22].
The partly very deviating results comparing studies on silicone oil assisted macular hole surgery are difficult to interpret. One reason may be different study designs with small or variable sample sizes as well as differences in age, comorbidities and ophthalmologic medical history of the patients. Results may also be influenced by variable classifications, hole sizes and measurements as well as duration of symptoms. Surgeons‘ proclivity for a certain technique and corresponding surgical skill may also play a role. Furthermore, the surgical modalities may vary with regard to the silicone oil used (1.000, 2.000 and 5.000 cst) and the additional application of surgical adjuncts such as autologous serum [19,22].
However, we strongly believe that silicone oil tamponade to seal a macular hole is still a very useful technique for several reasons. One major advantage is the fact that, in contrast to “newer” surgical approaches [13-17], no manipulation of the macular hole and the neurosensory is required, nor is there a danger to negatively affect the subretinal space and the RPE. Furthermore, the installation of a silicone oil tamponade in macular hole surgery is quite easy to perform. More importantly, previous experimental studies evaluated the fluid under silicone (“sub-silicone oil fluid”) and examined multiple inflammatory cytokine levels and osmotic pressures [32]. Lambrou et al. performed an animal experiment to examine the effect of silicone oil or sub-silicone oil fluid on RPE cells [33]. RPE is thought to be one of the major players in inducing PVR by biologically promoting epithelial-mesenchymal transition [33,34]. The authors suggested that silicone oil in the vitreous cavity had an increased mitogenic activity for RPE cells compared to gas-filled or fluid-filled-vitreous [33]. In 2004, Asaria and coworkes also demonstrated that the concentration of fibrogenic (bFGF) and inflammatory (IL-6) growth factors and protein is raised in retro-silicone oil fluid [35]. They suggested that this finding may contribute to the process of retro-oil perisilicone proliferation and subsequent fibrocellular membrane formation. Taken together, this data underline the fact that silicone oil fill of the vitreous cavity is associated with fibrocellular proliferation which may be very beneficial to assist the closure of macular holes, especially in cases with persistent holes and larger macular hole diameters.
Conclusion
In summary, we believe that silicone oil tamponade in selected macular hole cases should not be forgotten in the times of new and “sexier” surgical approaches for these cases, since it provides good anatomical and functional results without excessive manipulation at the central retina. We believe that there is an unmet need for larger, multicentric studies with a stringent study protocol comparing different surgical techniques especially for large and persistent macular holes including silicone oil assisted and recent techniques using autologous transplants in macular hole surgery.
Ethics Approval
Ethical approval was waived by the local Ethics Committee of Ludwig Maximilian University of Munic in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Author Contributions Statement
All authors fulfill the ICMJE criteria for authorship.
References
- Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991;109:654-9.
- Gupta D. Face-down posturing after macular hole surgery: A review. Retina. 2009;29:430-43.
- Feng X, Li C, Zheng Q, et al. Risk of silicone oil as vitreous tamponade in pars plana vitrectomy: A systematic review and meta-analysis. Retina. 2017;37:1989-2000.
- Vaziri K, Schwartz SG, Kishor KS, et al. Tamponade in the surgical management of retinal detachment. Clin Ophthalmol. 2016;10:471-6.
- Briand S, Chalifoux E, Tourville E, et al. Prospective randomized trial: Outcomes of sf(6) versus c(3)f(8) in macular hole surgery. Can J Ophthalmol. 2015;50:95-100.
- Hasegawa Y, Hata Y, Mochizuki Y, et al. Equivalent tamponade by room air as compared with sf(6) after macular hole surgery. Graefes Arch Clin Exp Ophthalmol. 2009;247:1455-9.
- Rahman R, Madgula I, Khan K. Outcomes of sulfur hexafluoride (sf6) versus perfluoroethane (c2f6) gas tamponade for non-posturing macular-hole surgery. The Br J Ophthalmol. 2012;96:185-8.
- Duker JS, Kaiser PK, Binder S, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611-9.
- Pieczynski J, Kuklo P, Grzybowski A. Pars plana vitrectomy with silicone oil tamponade for primary and secondary macular hole closure: Is it still a useful procedure Pars plana vitrectomy with silicone oil tamponade for primary and secondary macular hole closure: Is it still a useful procedure? Eur J ophthalmol. 2018;28:503-14.
- Xia S, Zhao XY, Wang EQ, et al. Comparison of face-down posturing with nonsupine posturing after macular hole surgery: A meta-analysis. BMC ophthalmology. 2019;19:34.
- Couvillion SS, Smiddy WE, Flynn HW Jr., et al. Outcomes of surgery for idiopathic macular hole: A case-control study comparing silicone oil with gas tamponade. Ophthalmic Surg Lasers Imaging. 2005;36:365-71.
- Morimoto E, Shimada Y, Sugimoto M, et al. Adherence to face-down and non-supine positioning after macular hole surgery. BMC ophthalmology. 2018;18:322.
- Michalewska Z, Michalewski J, Adelman RA, et al. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018-25.
- Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA ophthalmology. 2016;134:229-30.
- Rizzo S, Caporossi T, Tartaro R, et al. A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina. 2019;39:S95-S103.
- Yepez JB, Murati FA, De Yepez J, et al. Anterior lens capsule in the management of chronic full-thickness macular hole. Retin Cases Brief Rep. 2018;12:286-90.
- Fotis K, Alexander P, Sax J, et al. Macular detachment for the treatment of persistent full-thickness macular holes. Retina. 2019;39:S104-S107.
- Fawcett IM, Williams RL, Wong D. Contact angles of substances used for internal tamponade in retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol. 1994;232:438-44.
- Goldbaum MH, McCuen BW, Hanneken AM, et al. Silicone oil tamponade to seal macular holes without position restrictions. Ophthalmology. 1998;105:2140-7.
- Elliott DB. The good (logmar), the bad (snellen) and the ugly (bcva, number of letters read) of visual acuity measurement. Ophthalmic Physiol Opt. 2016;36:355-8.
- Lai JC, Stinnett SS, McCuen BW. Comparison of silicone oil versus gas tamponade in the treatment of idiopathic full-thickness macular hole. Ophthalmology. 2003;110:1170-4.
- Kumar V, Banerjee S, Loo AV, et al. Macular hole surgery with silicone oil. Eye (Lond). 2002;16:121-5.
- Tafoya ME, Lambert HM, Vu L, et al. Visual outcomes of silicone oil versus gas tamponade for macular hole surgery. Seminars in ophthalmology. 2003;18:127-131.
- Pertile G, Claes C. Silicone oil vs. Gas for the treatment of full-thickness macular hole. Bull Soc Belge Ophtalmol. 1999;274:31-6.
- Singh SR, Hariprasad SM, Narayanan R. Current management of macular hole. Ophthalmic Surg Lasers Imaging Retina. 2019;50:61-8.
- Stalmans P, Pinxten AM, Wong DS. Cohort safety and efficacy study of siluron2000 emulsification-resistant silicone oil and f4h5 in the treatment of full-thickness macular hole. Retina. 2015;35:2558-66.
- Christmas NJ, Smiddy WE, Flynn HW Jr. Reopening of macular holes after initially successful repair. Ophthalmology. 1998;105:1835-8.
- Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939-48.
- Freeman WR, Azen SP, Kim JW, et al. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The vitrectomy for treatment of macular hole study group. Arch Ophthalmol. 1997;115:11-21.
- Karia N, Laidlaw A, West J, et al. Macular hole surgery using silicone oil tamponade. Br J Ophthalmol. 2001;85:1320-3.
- Ivanovska-Adjievska B, Boskurt S, Semiz F, et al. Treatment of idiopathic macular hole with silicone oil tamponade. Clin Ophthalmol. 2012;6:1449-54.
- Kaneko H, Takayama K, Asami T, et al. Cytokine profiling in the sub-silicone oil fluid after vitrectomy surgeries for refractory retinal diseases. Sci Rep. 2017;7:2640.
- Lambrou FH, Burke JM, Aaberg TM. Effect of silicone oil on experimental traction retinal detachment. Arch Ophthalmol. 1987;105:1269-72.
- Takayama K, Kaneko H, Hwang SJ, et al. Increased ocular levels of microrna-148a in cases of retinal detachment promote epithelial-mesenchymal transition. Invest Ophthalmol Vis Sci. 2016;57:2699-705.
- Asaria RH, Kon CH, Bunce C, et al. Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J ophthalmol. 2004;88:1439-42