Mini Review - Journal of Clinical Ophthalmology (2020) Therapeutic Advances in Vision Research
Keratoconus in Upper Egypt: Where are we standing?
Mortada Ahmed Abozaid*
Department of Ophthalmology, Sohag University, Sohag Governorate, Egypt
- Corresponding Author:
- Dr. Mortada Ahmed Abozaid
Department of Ophthalmology Faculty of medicine Sohag University Egypt
E-mail: mourtada_abdelaal@med.sohag.edu.eg
Accepted date: April 7, 2020
Citation: Abozaid MA. Keratoconus in Upper Egypt: Where are we standing?. J Clin Ophthalmol 2020;4(S1):1-3
Abstract
Keratoconus represents a major health problem in Upper Egypt; it is defined as a progressive non-inflammatory thinning of the cornea which assumes a conical shape. It is a vision threatening form of corneal ectasia the prevelance of which is thought to be underestimated and its treatment has become much easier in the last few years thanks to the wide availability of accurate diagnostic tools; namely corneal tomography and anterior segment optical coherence tomography and efficient treatment procedures; namely femtosecond laser-assisted intrastromal corneal ring segments implantation and accelerated corneal cross-linking. Eye doctors in Upper Egypt wish to launch widespread screening programs for early detection of keratoconus which ensure better management and more preservation of vision.
Keywords
Cross-linking, Kerarings, Pentacam, Screening for keratoconus
Introduction
Keratoconus is the most common form of corneal ectasia. It is characterized by non-inflammatory thinning of the corneal stroma leading to progressive myopia, astigmatism, large amount of high order aberrations and finally loss of vision due to corneal opacification. The onset of keratoconus is usually at puberty and then progresses at variable rates till it arrests in the 3rd or 4th decades. However, it can start or arrest at any age. It is a bilateral disease which may affect one eye more than the other and is well known to be aggravated by eye rubbing [1,2].
The prevalence of keratoconus is widely variable in different regions of the world. In Upper Egypt which is the southern part of Egypt, the weather is characterized by being hot, dry and dusty. Accordingly, the prevelance of keratoconus is relatively higher compared to other regions which together with low socioeconomic levels make this potentially blinding disease a major health problem in Upper Egypt [3].
Review Analysis
The clinical features of keratoconus vary according to the stage of progression or severity with many patients discovered accidentally during screening for refractive surgery. We should here remember that most patients with keratoconus do not prefer glasses or contact lenses due to their suboptimal vision and so tend to seek for refractive surgery and thus may increase the prevalence of keratoconus among refractive candidates.
While in its well-established form, patients complain from defective, distorted or suboptimal vision and show classic signs on examination such as scissoring red reflex, oil droplet, Munson’s sign, Vogt’s striae, Fleisher ring or scarring. Unlike many other diseases such as glaucoma or retinal dystrophies, keratoconus doesn’t lead to total blindness.
Discussion
The great advancement in the field of corneal imaging and its wide availability suggested that the prevalence of keratoconus is underestimated. We should take advantage of such advancement in its early detection. Such early diagnosis will allow more preservation of vision, less need for keratoplasty and lower economic burden on the health care systems. Elevation-based corneal tomography especially that relying on the principle of Scheimpflug imaging represents the major tool in the early detection of keratoconus and the most effective method for screening of refractive candidates. Anterior-segment optical coherence tomography is also helpful in determining the depth and continuity of the demarcation line seen in the cross-linked cornea as an indicator of the efficacy of cross-linking.
Until recently, ophthalmologists have been watched patients with keratoconus suffering from progressive visual loss until they reach the end stage of the disease when surgical intervention in the form of keratoplasty is offered to restore their vision. However, the poor access to donor eye banks, the high surgical skills required in addition to the possible devastating complications of keratoplasty made many doctors and patients afraid of such surgery.
Thanks to the Dresden group [4], it became possible for the first time, to arrest the progression of keratoconus via corneal cross- linking surgery. In this surgery, a photochemical reaction is induced within the corneal stroma through activation of a photo- sensitizer (such as riboflavin) by ultraviolet light to release free oxygen radicals resulting in the formation of new covalent bonds between collagen fibrils that eventually strengthen the cornea and stop progression of ectasia. The accelerated mode of CXL made it more convenient to both the patient and the surgeon. According to Bunsen-Roscoe law of reciprocal irradiation, delivering 5.4 J/cm2 of UV light can be done via 30 minutes of irradiation at 3.0 mW/cm2 or 3 minutes of irradiation at 30 mW/cm2. However, the limiting factor would be availability of oxygen for formation of free radicals [5].
The KXL® accelerated CXL system of Avedro (Waltham, Massachusetts, USA) is the most commonly used CXL device in Upper Egypt. It has the options of epithelium-on or epithelium-off, pulsed or continuous treatments via 4 preset protocols of accelerated CXL in addition to the conventional Dresden protocol and a separate protocol for Lasik extra. An extra user programmable protocol is also available for surgeon convenience. The epi-on method is the one used when CXL is combined with ICRS implantation and the pulsed mode has the theoretical advantage of allowing more time for oxygen delivery necessary for the photochemical reaction.
The introduction of Intrastromal Corneal Ring Segments (ICRS) implantation helped more in the visual rehabilitation of keratoconic patients. These are synthetic segments that act as a spacer within the peripheral corneal stroma to cause an arc-shortening effect of the central cornea thus reducing its curvature and power. These segments were developed originally to correct low and moderate degrees of myopia but their effect was overcome by the great success of laser correction procedures and so their use shifted to correct the refractive, topographic and aberrometric changes of keratoconic corneas [6,7].
Kerarings are the only ICRS available in Upper Egypt. They are manufactured by Mediphacos from polymethylmethacrylate in different arc lengths. They have a triangular cross section and a 600 um base diameter while the apical diameter measures 5 mm. They are available in 0.05 mm steps thicknesses. A nomogram provided by the manufacturer is used to select the suitable ring segements in every patient.
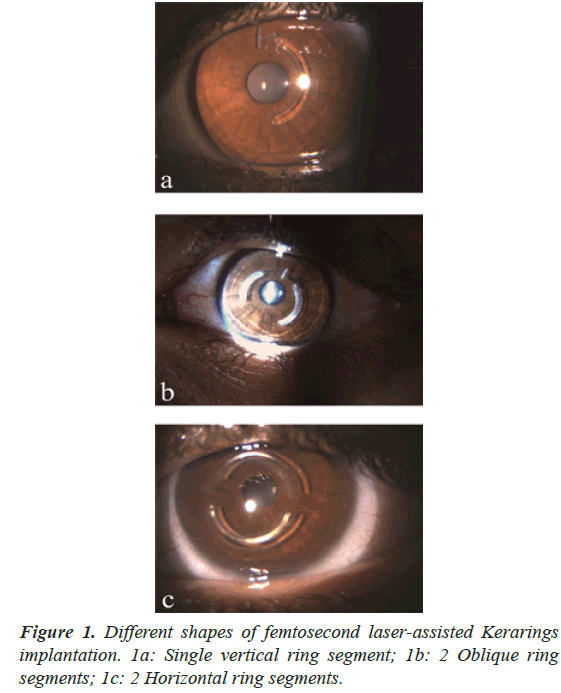
The introduction of femtosecond laser technology in the creation of intrastromal tunnels made ICRS implantation much easier, more accurate and with fewer complications compared to the manual technique. The iFS advanced femtosecond laser (Abbott, Chicago, Illinois, USA) is the most commonly used platform in Upper Egypt. The corneal tunnel usually has an inner diameter of 5 mm and an outer diameter of 5.9 mm and it is created at a depth of 75%-80% of the thinnest corneal location with the incision placed at the axis of the steeper keratometry (Figure 1).
Other efforts to rehabilitate vision in keratoconic patients included topography-guided Photorefractive Keratectomy (PRK), toric Implantable Collamer Lenses (ICL) and toric Intraocular Lenses (IOL). Combining PRK (topography-guided or wavefront-guided) with CXL looks attractive for the visual rehabilitation of keratoconic patients, however the behavior of cross-linked cornea remains unpredictable compared to the normal cornea despite the gain in its rigidity by CXL. On the other hand, combining CXL with toric ICLs or toric IOLs has a great dilemma in the correct calculation of the power of the lens to obtain emmetropia.
Although ICRS and CXL have revolutionized the management of keratoconus, we are still in need for more efforts to approach results comparable to laser vision correction procedures in keratoconic eyes especially after availability of femtosecond laser assistance of ICRS and accelerated devices of CXL. A change in the ability of the combined ICRS and CXL to fully correct the refractive error of keratoconic patients would represent a major advance in management [8,9].
ICRS are well known to improve the vision in keratoconic eyes, however it is still unclear if they can halt the progression of the disease or not. On the other hand, CXL is confirmed to stabilize the keratoconic cornea and halt its progression but we are not sure if it can improve the vision as well. Many ophthalmologists think that combining these 2 procedures has synergistic effect rather than an additive effect on improving the vision and halting progression of keratoconus and consequently we need to develop new nomograms which take such effect into consideration.
The use of vector analysis especially Alpins’ method to assess astigmatism correction after ICRS implantation is easy to apply and very important to understand the effects of ICRS on the cornea for better adjustment of the nomograms used to select the suitable ring segments. Such adjustment, as we mentioned, is our priority now to increase patient satisfaction and reduce the need for glasses postoperatively [10-12].
Combining femtosecond laser-assisted ICRS and accelerated CXL in one procedure has many advantages over sequential surgery such as decreased cost, faster rehabilitation and more importantly enhancing the effect of CXL by giving an extra pathway for the delivery of riboflavin deep into the stroma through the fresh tunnels created for ICRS insertion.
The safety profile of such combined procedure is excellent. The intraoperative complications are few and include inaccurate detection of the corneal reflex for good centration of the rings, loss of vacuum during tunnel creation, difficult insertion of the rings and inadequate soaking of the cornea with riboflavin. While the postoperative complications include infection, scarring, ring migration or extrusion, corneal haze and failure of corneal stabilization requiring repeat cross-linking.
Although many patients are satisfied with their ICRS, few are unhappy with them mostly due to the unexpected behavior of their abnormal corneas to the ICRS implantation. Such behavior may necessitate explanation of the rings with or without insertion of new ones.
Keratolasty is considered the final and radical solution for keartoconus; however eye doctors face several problems in this surgery. The law which regulates corneal transplantation in Egypt has been issued since 1962 and although it was modified several times, there is still existing extreme difficulty in finding donors which makes keratoplasty surgery entirely dependent on imported corneas from countries other than Egypt. In addition, the great skills needed and the high potential of complications makes keratoplasty surgery unfavorable in Upper Egypt.
Conclusion
Eye doctors in Upper Egypt wish to alert the community to the risks of keratoconus in order to adopt a road map for its management including:
• Mass education of the hazards of eye rubbing on the cornea.
• Prompt treatment of childhood allergies especially vernal keratoconjuctivitis.
• Screening for keratoconus through corneal topography in school children and high risk patients such as those with spring catarrh, family history of keratoconus or patients with irregular or rapidly changing astigmatism.
• Providing corneal cross-linking via health insurance.
References
- Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322.
- Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319.
- Saro AS, Radwan GA, Mohammed UA, et al. Screening for keratoconus in a refractive surgery population of Upper Egypt. Delta Journal of Ophthalmology 2018;19:19–23.
- Wollensak G, Spoerl E, Seiler T. Stress–strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg. 2003;29:1780–5.
- Goldich Y, Marcovich AL, Barkana Y, et al. Safety of corneal collagen cross-linking with UV-A and riboflavin in progressive keratoconus. Cornea. 2010;29:409–11.
- Colin J, Cochener B, Savary G, et al. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000; 26:1117–22.
- El-Raggal TM. Sequential versus concurrent KERARINGS insertion and corneal collagen cross-linking for keratoconus. Br J Ophthalmol. 2011;95:37–41.
- Abozaid MA. Sequential Keraring implantation and corneal cross-linking for the treatment of keratoconus in children with vernal keratoconjunctivitis. Clin Ophthalmol. 2017;11:1891–5.
- Abozaid MA, Hassan AAA, Abdalla A. Intrastromal corneal ring segments implantation and corneal cross-linking for keratoconus in children with vernal keratoconjunctivitis–three-year results. Clin Ophthalmol. 2019;13:2151–7.
- Alpins N.Astigmatism analysis by the Alpins method. J Cataract Refract Surg. 2001:27:31-49.
- Alpins N. A new method of analyzing vectors for changes in astigmatism. J Cataract Refract Surg. 1993:19:524-33.
- Abozaid MA, Abdalla A. Vector Analysis of Astigmatism in Keratoconic Eyes After Combined Intrastromal Corneal Ring Segments Implantation and Collagen Cross-Linking. Clin Ophthalmol. 2020;14:473-80.