Case Report - Journal of Clinical Dentistry and Oral Health (2017) Oral Medicine and Surgery
Glandular odontogenic cyst of the anterior maxilla in a 13-year old male: a rare case of location and age.
John J Frazier1* and Diane J Flint2
1Oral and Maxillofacial Radiology, Texas A and M College of Dentistry, TX 75246, USA
2Oral and Maxillofacial Radiology Advanced Education Program, Texas A and M College of Dentistry, TX 75246, USA
- *Corresponding Author:
- John J Frazier
Oral and Maxillofacial Radiology
Texas A and M College of Dentistry, USA
Accepted on February 24, 2017
Citation: Frazier JJ, Flint DJ. Glandular Odontogenic Cyst of the Anterior Maxilla in a 13-Year Old Male: A Rare Case of Location and Age. J Oral Med Toxicol. 2017;1(1);10-13
Abstract
The Glandular Odontogenic Cyst (GOC) was first described by Gardner in 1988 and recognized as a distinct entity by the World Health Organization in 1992. Padayachee and Van Wyk in 1987 described a cyst with histological features similar to the botryoid odontogenic cyst and a mucoepidermoid tumor and termed it “sialo-odontogenic cyst”. The GOC comprises 0.012- 1.3% of all jaw cysts. It most commonly occurs in the 4th decade and rarely occurs in persons under twenty years of age. The mandible is the most common site with approximately 75% of the reported cases. The significance of this paper is in reporting the combination of two rare characteristics of location and age in one patient.
Introduction
The Glandular Odontogenic Cyst (GOC) is a rare developmental odontogenic cyst that occurs 75% of the time in the mandible and rarely presents in persons under 20 years of age [1]. The GOC was originally described by Padayachee and Van Wyk [2] in 1987 who reported on two cases of multilocular mandibular cysts with features of both Botryoid Odontogenic Cyst (BOC)and central mucoepidermoid tumor (mucoepidermoid carcinoma or MEC). They concluded that these lesions differed from a BOC and MEC and warranted a separate classification, which they termed sialo-odontogenic cyst. Gardner et al. [3] described eight cases with similar histological features and coined the name glandular odontogenic cyst to emphasize the odontogenic derivation of this cyst. The glandular odontogenic cyst or sialo-odontogenic cyst was included as a distinct entity as a developmental odontogenic cyst in the 1992 WHO’s Histological Typing of Odontogenic Tumors [4]. It was defined as “a cyst arising in the tooth-bearing areas of the jaws and characterized by an epithelial lining with cuboidal or columnar cells both at the surface and lining crypts or cyst-like spaces within the thickness of the epithelium”. GOCs should be distinguished from other odontogenic cysts because: (1) They can recur more often than dentigerous or radicular cysts; and (2) Their histologic appearance can overlap with the lateral periodontal cyst, botryoid odontogenic cyst and central mucoepidermoid carcinoma [5]. Since the GOC is a relatively recently described entity, there is not much information in the literature regarding the clinicopathological features of GOC’s, or their occurrence in the maxilla and in a young age group. This paper describes a rare case of 13-year-old male with a GOC of the anterior maxilla.
Case Report
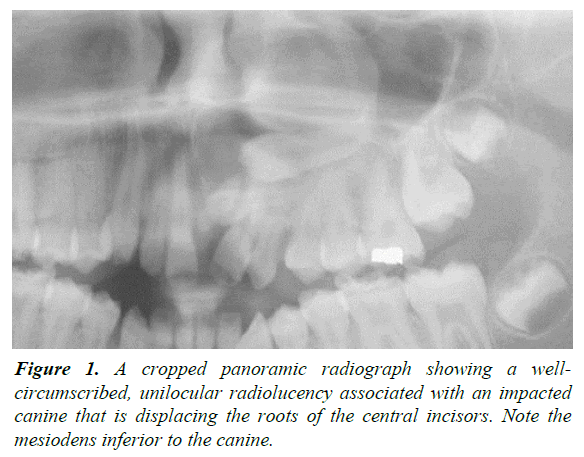
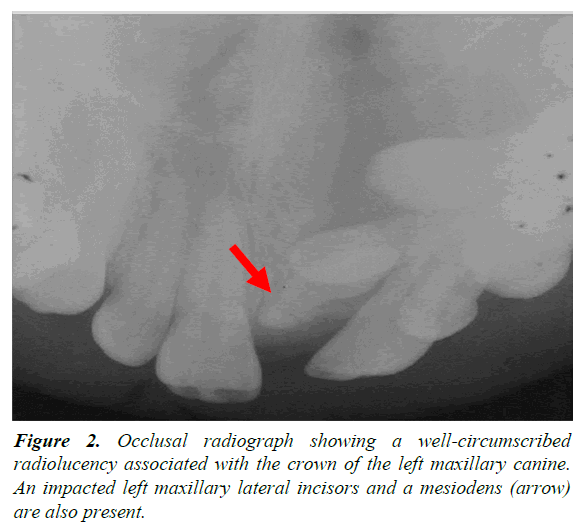
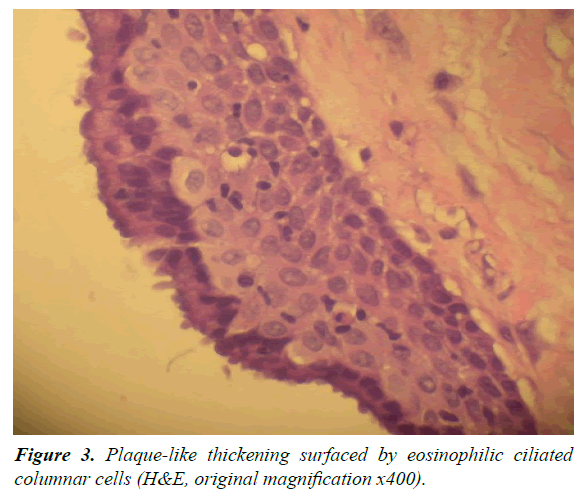
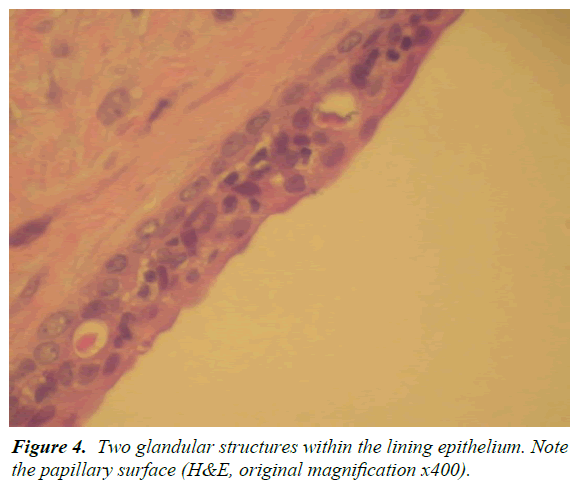
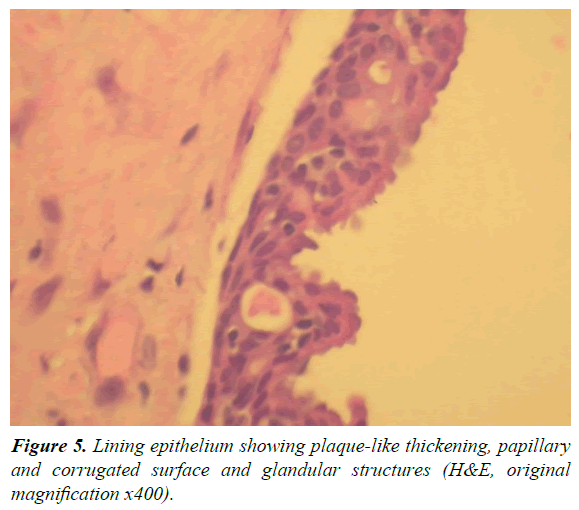
A 13-year-old male was referred by an orthodontist to an oral surgeon for evaluation of impacted teeth #10 and #11 and a mesiodens. A panoramic and occlusal radiograph revealed a well-circumscribed unilocular radiolucency associated with the crown of an impacted left maxillary canine. The border of the lesion was corticated and originated from approximately the cemento-enamel junction of the impacted canine. It extended superoinferiorly from the nasal fossa floor to the maxillary alveolar ridge. In the mesiodistal direction, the lesion extended from the mesial aspect of the root of the right maxillary central incisor to the mesial aspect of the root of the left maxillary 1st premolar. In the anteroposterior dimension, the lesion extended from the facial cortical plate of the maxilla to the anterior border of the inferior turbinate. The lesion displaced the roots of the left maxillary central and lateral incisors distally. No root resorption or cortical bone expansion was noted (Figures 1 and 2). The differential diagnosis included dentigerous cyst, Odontogenic Keratocyst (OKC), and, given the patient age/ location/association with an impacted canine, an Adenomatoid Odontogenic Tumor (AOT). With a presumed diagnosis of a dentigerous cyst, the original treatment plan consisted of enucleation of the cyst, extraction of the mesiodens and orthodontic assisted eruption of left maxillary lateral incisor and canine. Eventually it was determined that the teeth could not be brought in orthodontically due to their high horizontal position and location between the roots of the bicuspids. The teeth were therefore extracted. At the time of surgery, the large size of the lesion and bony erosion suggested that the lesion could possibly be an OKC, and was treated by enucleation along with Carnoy's solution. Post-surgery, the tissue was sent to the hospital surgical pathology department with a tentative diagnosis of a dentigerous cyst. The histological examination showed a cystic structure surfaced predominantly by a thin layer of epithelium with focal plaque-like thickenings. In areas, the luminal surface of the epithelium demonstrated a layer of columnar cells and glandular structures (Figures 3-5). The histological findings were consistent with a diagnosis of glandular odontogenic cyst. At present, no other treatment is planned for this patient. The follow-up plan is re-evaluation every three months with a new radiograph at six months and at one year. After three years the patient will be followed every six months.
Differential Diagnosis
The present case is of a young adolescent male with a radiolucent lesion associated with an impacted canine of the anterior maxilla. A reasonable differential diagnosis would consist of entities with the above characteristics and would include a dentigerous cyst, an odontogenic keratocyst and an adenomatoid odontogenic tumor. The dentigerous cyst is the most common radiolucent lesion associated with the crown of an unerupted tooth and represents about 20% of the odontogenic cysts with the mandibular 1st molar being the most affected and the maxillary canines and maxillary molars being the 2nd most common sites [1]. The radiographic features of the dentigerous cyst are of a well-defined radiolucency surrounding the crown of an impacted tooth with the lesion attached to the cemento-enamel junction. Treatments for a dentigerous cyst consist of enucleation and marsupialization with a good prognosis [6]. The odontogenic keratocyst is a developmental lesion that primarily affects persons in the age range of 10-30 years old [7]. It has a propensity for the posterior mandible and the ascending ramus but can be found anywhere in the jaws. Radiographically it is radiolucent and can be either unilocular or multilocular with a tendency to grow in an elongated fashion with minimal expansion of the cortical bone [8]. Odontogenic keratocysts are t associated with crowns of teeth in 25-40% of cases [1]. When associated with the crown of a tooth, OKCs usually attach at a level inferior to the cemento-enamel junction and therefore can be distinguished from a dentigerous cyst. If the attachment is close to or on the cemento-enamel junction, it can be difficult to differentiate between the two entities. Treatment for an odontogenic keratocyst is enucleation and curettage with or without the use of Carnoy’s solution [9]. Odontogenic keratocyst have high recurrence rates [8] and should be followed post-surgery. The adenomatoid odontogenic tumor is a benign neoplasm that represents 3-7% of all odontogenic tumors with two-thirds of patients affected occurring in the age range of 10-19 years old [10]. There are three types of adenomatoid odontogenic tumors, the follicular type, which is associated with an impacted tooth and represents 73% of cases, the extrafollicular type not associated with a tooth and representing 24% of cases, and the peripheral type [11]. In the follicular type, the crown of the impacted tooth with or without portions of the root is encapsulated. The encapsulation can be totally radiolucent or, more often, it may contain flecks of calcifications [1]. When only the crown is encapsulated by a radiolucent lesion, radiographically differentiating adenomatoid odontogenic cysts from a dentigerous cyst can be challenging and it has been documented that 77% of the follicular type AOTs are initially diagnosed as dentigerous cysts [12]. The differential diagnosis of dentigerous cyst, odontogenic keratocyst and adenomatoid odontogenic tumor was based on the well-defined radiolucent lesion surrounding the crown of an unerupted canine.
A dentigerous cyst was the most likely lesion to fit the radiographic findings. The odontogenic keratocyst and adenomatoid odontogenic tumor both meet the criteria and either could arguably be considered more likely. The glandular odontogenic cyst would not be considered in the differential as the patient’s age, the site of the lesion, and the lack of GOCs being associated with the crown of an unerupted tooth would preclude this diagnosis.
Discussion
The glandular odontogenic cyst is a rare entity that was first described by Gardner [3] in 1988 and was recognized as a distinct entity by the World Health Organization in 1992. The characteristic histological features are a cystic space lined by non-keratinized stratified epithelium surfaced by eosinophilic cuboidal or columnar cells. Occasionally these cells may be ciliated and the surface can have papillary projections. The lining can have plaque-like thickenings [5,13-15] similar to that seen in the Lateral Periodontal Cyst (LPC) or BOC. Within the lining epithelium are micro-cystic or glandular structures, as well as epithelial whorls or spheres [3], mucin pools and mucous cells. Although GOCs generally have mucous cells within the lining epithelium or lining the glandular spaces, their presence is not unique and can be seen in many intraosseous cysts and have been reported in 5-27% of odontogenic cysts. Clinically, it is most common in middle age adults with most reports having a mean age in the 4th decade and a few cases reporting it in the 5th decade. The age ranges from 11 to 90 years old. Males and females are affected equally; however males tend to be affected at a younger age then females. The GOC has a predilection for the anterior jaws with an affinity for the anterior mandible with as many as 75% of the cases reported there [1]. When in the mandible, it has a tendency to cross the midline and it has been reported to cross the midline in the maxilla [1,5,15-20]. Infrequently it is seen in the posterior jaws. Radiographically, the lesion presents either as a unilocular or multilocular radiolucency with well-defined margins and a sclerotic rim. The behaviour of GOCs are of an aggressive growth potential and a tendency to recur. Recurrence rates are 21-30% and have been reported as high as 55% with conservative treatment [13]. The GOC represents 0.012-1.3% of all jaw cysts, though it has been suggested that these numbers may be conservative, as cases of GOC could have been diagnosed as central MEC or LPC [13]. The treatment modalities range from conservative treatment: excision enucleation, curettage and meticulous follow-up [14-16] to aggressive treatment: marginal or enbloc resection. Aggressive treatment is recommended by some authors due to the aggressive growth and recurrence of these cysts. Histologically, GOC can be similar to LPC and BOC or MEC [1,5,13-21]. In certain focal microscopic fields, however, examining multiple fields should give the pathologist enough information to differentiate these entities. GOC, like LPC and BOC exhibit plaque-like thickenings but LPC and BOC lack glandular structures and ciliated epithelium, features found in GOC. A more difficult distinction is between a GOC and MEC, especially a cystic MEC. Both can have cystic spaces lined by epithelium containing mucous cells and gland-like structures [13,17]. The one feature not reported in MEC that can help in differentiating it from a GOC is plaque-like thickenings [17]. The present case is of a 13-year-old male with a GOC in the anterior maxilla. Though the anterior maxilla is the 2nd most common site affected, relative to the mandible it represents the minority of cases seen clinically with very few cases reported in the literature [5,14]. Glandular odontogenic cysts in young persons are rare. In a four global group systematic review, MacDonald-Jankowski [19] found no cases of GOC in the 0-9 year old group and the 10-19 year old group represented 10% of the total of all GOC. In a thirty year review of odontogenic cysts in the United Kingdom, Jones et al. [20] found no cases of GOC in the paediatric population. A literature search for GOC of the anterior maxilla in a young person produced no results. This paper adds to the small body of literature on GOC and a unique perspective on its presentation by reporting an extremely rare case (perhaps the first case) of GOC in the anterior maxilla of an adolescent male.
References
- Neville BW, Damm DD, Allen CM, et al. Oral and Maxillofacial Pathology. 3rd edn. Elsevier BV; 2009.
- Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987;16(10):499-504.
- Gardner DG, Kessler HP, Morency R, et al. The glandular odontogenic cyst: an apparent entity. J Oral Pathol. 1988;17(8):359-66.
- Speight, P. WHO International histological classification of tumours: Histological typing of odontogenic tumours. 2nd edn. In: Kramer IRH, Pindborg JJ, and Shear M (eds). Springer-Verlag, Heidelberg. J Pathol. 1992;168(4): 427-8.
- Sittitavornwong S, Koehler JR, Said-Al-Naief N. Glandular Odontogenic Cyst of the Anterior Maxilla: Case Report and Review of the Literature. J Oral Maxillofac Surg. 2006;64(4):740-5.
- Santos BZ, Beltrame AP, Bolan M, et al. Dentigerous cyst of inflammatory origin. J Dent Child (Chic). 2014;81(2):112-6.
- Kaushik R, Pushpanshu K, Punyani SR, et al. Giant keratocystic odontogenic tumor: a challenging diagnosis. Autops Case Rep. 2016;6(3):41-6.
- Chaudhary S, Sinha A, Barua P, et al. Keratocystic odontogenic tumour (KCOT) misdiagnosed as a dentigerous cyst. BMJ Case Rep. 2013.
- Diaz-Belenguer A, Sanchez-Torres A, Gay-Escoda C, Role of Carnoy's solution in the treatment of keratocystic odontogenic tumor: A systematic review. Med Oral Patol Oral Cir Bucal. 2016;21(6):689-95.
- Dhirawani RB, Pathak S, Mallikaarjuna K, et al. An adenomatoid odontogenic tumor in disguise. J Indian Soc Pedod Prev Dent. 2016;34(3):291-3.
- Won-Gyo S, Chul-Hwan K, Hae-Seo P, et al. Adenomatoid odontogenic tumor associated with an unerupted mandibular lateral incisor: a case report. J Korean Assoc Oral Maxillofac Surg. 2015;41(6):342-5.
- Philipsen HP, Reichart PA. Adenomatoid odontogenic tumour: facts and figures. Oral Oncol. 1999;35(2):125-31.
- Krishnamurthy A, Sherlin HJ, Ramalingam K, et al. Glandular Odontogenic Cyst: Report of Two Cases and Review of Literature. Head Neck Pathol. 2009;3(2):153-8.
- Guruprasad Y, Chauhan DS. Glandular odontogenic cyst of the maxilla. J Clin Imaging Sci. 2011;1:54.
- Koppang HS, Johannessen S, Haugen LK, et al. Glandular odontogenic cyst (sialo-odontogenic cyst): report of two cases and literature review of 45 previously reported cases. J Oral Pathol Med. 1998;27(9):455-62.
- Magnusson B, Göransson L, Odesjö B, et al. Glandular odontogenic cyst. Report of seven cases. Dentomaxillofac Radiol. 1997;26(1):26-31.
- Noffke C, Raubenheimer EJ. The glandular odontogenic cyst: clinical and radiological features; review of the literature and report of nine cases. Dentomaxillofac Radiol. 2002;31(6):333-8.
- Foss RD, Fielding CG. Glandular Odontogenic Cyst. Head Neck Pathol. 2007;1(2):102-3.
- MacDonald-Jankowski DS. Glandular odontogenic cyst: systematic review. Dentomaxillofac Radiol. 2010;39(3):127-39.
- Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006;35(8):500-7.
- Savage NW, Joseph BK, Monsour PA, et al. The glandular odontogenic jaw cyst: report of a case. Pathology. 1996;28(4):370-2.