Research Article - Archives of General Internal Medicine (2017) Volume 1, Issue 3
Forced Expiratory Volume Factors of Stage III Non-Small Cell Lung Cancer Patients.
Rabindra Nath Das*
Department of Statistics, The University of Burdwan, Burdwan, West Bengal, India
- *Corresponding Author:
- Rabindra Nath Das
Department of Statistics
The University of Burdwan
West Bengal, India
E-mail: rabin.bwn@gmail.com
Accepted on June 12, 2017
Citation: Das RN. Forced expiratory volume factors of stage III non-small cell lung cancer patients. Arch Gen Intern Med. 2017;1(3):3-7
Abstract
Objectives: Forced expiratory volume in 1 (FEV1) second is known as the amount of air volume that can forcibly be blown out in one second, after full inspiration. Average FEV1 values between 80% and 120% are considered as normal. The determinants of FEV1 are aimed to identify in the report for stage III non-small cell lung cancer (SIIINSCLC) patients.
Background: Previous research articles have reported that the average FEV1 values in healthy individuals depend on height, age, body mass index, sex and ethnicity. Little studies have been performed regarding the FEV1 determinants for SIIINSCLC patients.
Materials and Methods: Published records on 239 SIIINSCLC patients with 23 study characters (variables/factors) are considered in the present study. The study variable FEV1 is positive and heterogeneous. Statistical analysis technique namely, joint generalized linear Log-normal models is used for analyzing the response FEV1.
Results: The mean FEV1 (MFEV1) is higher for SIIINSCLC patients who are current smoker (P=0.0601), or who have lower body mass index (BMI) (P=0.0599). Location of tumor is positively partially related (P=0.2365) with the MFEV1. The MFEV1 is higher for SIIINSCLC patients with histology level at squamous cell carcinoma (P=0.1088), or T-stage at level (T2=2) (P=0.1752), or N-stage at level (N2=3) (P=0.1440) and (N4 or Nx=4) (P=0.0142) than the other levels. The MFEV1 is higher for SIIINSCLC patients with chemotherapy at levels (standard sequential=3) (P<0.0001) and (standard concurrent=4) (P<0.0001), than the patients with no chemo level. The FEV1 variance (FEV1V) is higher for SIIINSCLC patients at older ages (P=0.1282), or never/exsmoker patients (P=0.2985). The FEV1V increases as the number of positive lymph node stations increases (P=0.0017). The FEV1V is inversely related with T-stage at level (T2=2) (P=0.0172) and at level (T4 or Tx=4) (P=0.0240). The FEV1V decreases at the higher equivalent dose (P=0.1822), or at larger gross tumor volume (P=0.0003), or at higher survival times (P=0.0451).
Conclusions: The FEV1 determinants for both the mean and variance have been identified for SIIINSCLC patients. These results may help the lung cancer specialists. The current findings of FEV1 (related to SIIINSCLC patients) are new addition to the lung cancer literature.
Keywords
Chemotherapy, Forced expiratory volume, Heteroscedastic, Log-normal model, Lung cancer
Introduction
Forced Expiratory Volume in 1 (FEV1) second is the amount of air volume that can forcibly be blown out from the lungs in the first second of a forced exhalation. FEV1 is highly related with the Chronic Obstructive Pulmonary Disease (COPD) which is a progressive disease that makes it hard to breath. For COPD patients, the air from their lungs is to be exhaled in smaller amounts and at a lower rate in comparison to a healthy individual without COPD. Generally, doctors use FEV1 as one of the measures to determine the lung function of an individual. Therefore, the determinants of FEV1 are very important to the medical practitioners. Many research articles have reported that the average FEV1 values in healthy individuals depend on height, age, body mass index, sex and ethnicity [1-5].
The new report makes an attempt to identify the FEV1 determinants for SIIINSCLC patients. Lung cancer starts if the lung cells become abnormal, and they grow out of control. Tumor is formed with the growing of more cancer cells, and the tumors spread through the different organs of the body. Generally, there are two types of lung cancers, namely, Non-Small Cell Lung Cancer (NSCLC), and Small Cell Lung Cancer (SCLC) [6-10]. The FEV1 of SIIINSCLC patients is positive and non-constant variance response. It belongs to exponential family distribution. So, it should be modeled using joint Log-normal and gamma models. Joint Log-normal model gives better fit of FEV1 for SIIINSCLC patients. Best of our knowledge, there is little study of FEV1 for SIIINSCLC patients. Thus, we have motivated to identify the FEV1 determinants for SIIINSCLC patients.
Materials
The considered data set is obtained from Oberije et al. [11]. It contains 239 SIIINSCLC patients, with 23 attribute characters/ variables. The data set can be obtained from the link: http://www.redjournal.org/article/S0360-3016(15)00254-0/fulltext. The covariates/factors along with their levels, means, standard deviations, proportions are displayed in Table 1. Data collection method, subject population are clearly described in Oberije et al.; Das and Mukherjee [11,12].
| Factors name | Operationalization | Mean (standard deviation)/Proportion |
|---|---|---|
| Sex | Sex (Male=1; Female=2) | 1%=73.1; 2%=26.9 |
| Age | Age at study | 65.56 (9.40) |
| WHO-PS | World helth organization performance status or measure (WHO-PS) levels are 1, 2, 3 | 1%=42.43; 2%=45.80; 3%=11.77 |
| BMI | bmipatient pre RT: Body mass index of patient at pre radiation therapy | 25.09 (4.14) |
| FEV1 | Forced expiratory volume in 1 second. percentage of predicted pre RT | 77.20 (21.10) |
| Smok2 | Never/ex smoker=1; Current smoker=2 | 1%=64.28; 2%=35.72 |
| T_ct_loc | CT-scan: Locations of tumor, 19 locations are: right lowerlobe (1); right middlelobe (2); right hilus (3); right upperlobe (4); leftlowerlobe (5); leftupperlobe (6); lefthilus (7); mediastinum (8); notapplicable (9); lingula (10); upperlobe, unspecified (11); lowerlobe, unspecified (12); lung,trachea (13); lung, trachea left (14); lung,trachea, right (15); LUL+LLL (16); right bronchus (17); left bronchus (18); multiple lobes (19) | 4.22 (1.13) Attribute character, but treated as discrete variable |
| Histology | Histology: (Adenocarcinoma=1; Squamous Cell Carcinoma=2, Large cell carcinoma=3, other=4) | 1%=32.35; 2%=15.96; 3%=39.07; 4%=12.62 |
| PLNS | Probably this is PLNS variable that means number of positive lymph node stations | 3.13 (1.21) |
| Countpet_mediast6g | None | 2.77 (1.03) |
| T-stage | T-stage (combined 6th or 7th edition): (T0-1=1; T2=2; T3=3; T4 or Tx=4) | 1%=13.02; 2%=36.13; 3%=9.66; 4%=41.19 |
| N-stage | N-stage (combined 6th or 7th edition): (N0=1; N1=2; N2=3; N3 or Nx=4) | 1%=17.22; 2%=2.10; 3%=49.15; 4%=31.53 |
| S-stage | Clinical overall stage: Levels: (IIIA=1; IIIB=2) | 1%=31.93; 2%=68.07 |
| Timing | Chemotherapy: Level: (No chemo=1; Sequential=2, Concurrent=3) | 1%=32.35; 2%; 15.96 3%=39.07 |
| Group | Group: (no chemo=1; sequentialselected=2; standard sequential=3; standard concomitant=4) | 1%=10.50; 2%=6.72; 3%=47.90; 4%=34.88 |
| Yearrt | Start of study | 2006 (2.32) |
| Equivalent-dose (Eqd) | Equivalent radiation dose (corrected for fraction size) at 2 Gray (Gray (Gy) is the SI unit of absorbed dose. One gray is equal to an absorbed dose of 1 Joule/kilogram (100 rads) | 59.69 (7.22) |
| Treatment time (Ott) | Overall treatment time | 30.10 (8.50) |
| Gtv1 | Gross tumor volume | 89.24 (97.83) |
| Tumorload_total | None | 123.45 (105.52) |
| Survmonth | Survival time in months | 26.77 (23.36) |
| Survyear | Survival time in years | 2.23 (1.95) |
| Deadstat | Dead/alive: (alive=1; dead=2) | 1%=84.45; 2%=15.55 |
Table 1. Factors/variables (operationalization) in the FEV1 analysis and descriptive statistics.
Statistical methods and FEV1 data analysis
The FEV1 response is continuous, positive and heteroscedastic. The probability distribution of FEV1 belongs to exponential family distribution. It should be analyzed by joint Log-normal or gamma model analyses which are given in Firth; Das and Lee; Lee et al.; Das [13-16]. One can easily find the detailed analysis techniques of joint Log-normal and gamma models in Lee et al.; Das [15-17]. These are not reproduced herein.
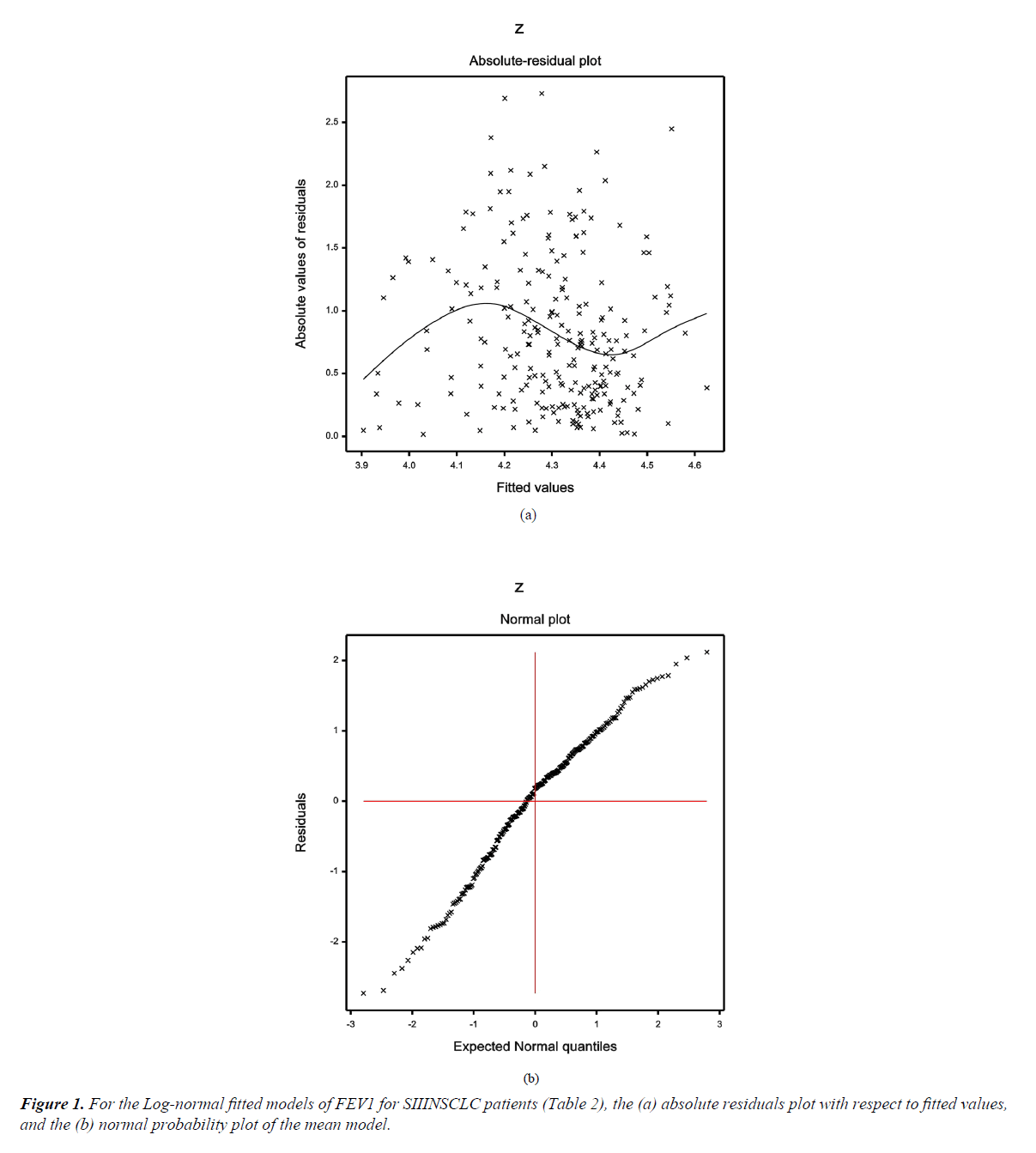
The response FEV1 is considered as the dependent variable, and the remaining others are considered as the explanatory factors/ variables. The response FEV1 has been fitted using both the joint Log-normal and gamma models. It is found that the joint Log-normal model fit gives better outcomes, than gamma fit. The outcomes of joint Log-normal model analysis are displayed in Table 2. On the basis of lowest Akaike information criterion (AIC=2063, for the fitted Log-normal model in Table 2) value in each class, the final fitted models have been selected. AIC selects a model that minimizes the predicted additive errors and squared error loss [18]. Some partially significant/insignificant factors/variables are included in both the mean and variance of the fitted Log-normal models (Table 2) for better fitting [18]. The included partially significant factors/variables in the fitted Log-normal models (Table 2) are called confounder in epidemiology. Diagnostic checkup of the final selected fitted Log-normal models in Table 2 is displayed in Figure 1.
| Model | Covariate | Estimate | Standard error | T-vale | P-value |
|---|---|---|---|---|---|
| Mean Model | Constant | 4.0770 | 0.14018 | 29.085 | <0.0001 |
| T-stage 2 | 0.0947 | 0.06960 | 1.360 | 0.1752 | |
| T-stage 3 | 0.0850 | 0.08347 | 1.018 | 0.3097 | |
| T-stage 4 | -0.0045 | 0.06965 | -0.065 | 0.9482 | |
| BMI | -0.0072 | 0.00382 | -1.891 | 0.0599 | |
| T_ct_loc | 0.0091 | 0.00770 | 1.187 | 0.2365 | |
| Group 2 | 0.0847 | 0.08372 | 1.012 | 0.3126 | |
| Group 3 | 0.2314 | 0.05491 | 4.215 | <0.0001 | |
| Group 4 | 0.3070 | 0.05668 | 5.417 | <0.0001 | |
| Smok 2 | 0.0589 | 0.03116 | 1.889 | 0.0601 | |
| Histology 2 | 0.0751 | 0.04665 | 1.610 | 0.1088 | |
| Histology 3 | 0.0021 | 0.03584 | 0.060 | 0.9522 | |
| Histology 4 | -0.0111 | 0.05231 | -0.212 | 0.8323 | |
| N-stage 2 | 0.0194 | 0.07621 | 0.255 | 0.7989 | |
| N-stage 3 | 0.0694 | 0.04735 | 1.466 | 0.1440 | |
| N-stage 4 | 0.1238 | 0.05008 | 2.472 | 0.0142 | |
| Dispersion Model | Constant | -0.7525 | 1.2521 | -0.601 | 0.5484 |
| Age | 0.0185 | 0.0121 | 1.527 | 0.1282 | |
| Smok 2 | -0.2247 | 0.2157 | -1.042 | 0.2985 | |
| PLNS | -0.2069 | 0.0652 | -3.175 | 0.0017 | |
| T-stage 2 | -0.7569 | 0.3146 | -2.406 | 0.0172 | |
| T-stage 3 | -0.3968 | 0.4422 | -0.897 | 0.3706 | |
| T-stage 4 | -0.7465 | 0.3286 | -2.272 | 0.0240 | |
| Equivalent dose | -0.0187 | 0.0140 | -1.338 | 0.1822 | |
| Gtv1 | -0.0053 | 0.0015 | -3.616 | 0.0003 | |
| Survmonth | -0.1204 | 0.0598 | -2.015 | 0.0451 |
Table 2. Joint Log-normal fitted model results of FEV1 for SIIINSCLC patients.
Figure 1a shows the Log-normal fitted absolute residual values plot in respect of fitted values (Table 2), which is a flat diagram with the running means, indicating that variance is constant. Figure 1b displays the normal probability plot for the Log-normal fitted mean model (Table 2), which does not reveal any kind of model lack of fit due to missing vales, or variables, or outliers.
Interpretations of FEV1 data analysis
The summarized outputs of the FEV1 analysis are displayed in Table 2. The mean model of FEV1 (Table 2) interprets the following:
1. The mean FEV1 (MFEV1) is inversely partially related with the Body Mass Index (BMI) (P=0.0599). It means that MFEV1 of SIIINSCLC patients is higher who have lower BMI.
2. The MFEV1is positively partially related with T-stage at level (T2=2) (P=0.1752), implying that MFEV1 is higher of SIIINSCLC patients at level (T2=2), than the other levels.
3. The MFEV1 is directly partially associated with smoking status (Smok2) (P=0.0601), indicating that MFEV1 is higher of current SIIINSCLC patients, than the never/ ex-smokers.
4. In the data set there are 19 locations of tumor. Location of tumor (P=0.2365) is partially positively related with the MFEV1.
5. The MFEV1 is directly related with chemotherapy group at level (standard sequential=3) (P<0.0001) and at level (standard concurrent=4) (P<0.0001), indicating that MFEV1 is higher at levels standard sequential=3 and standard concurrent=4, than the no-chemo=1 group and sequential selected=2 group of SIIINSCLC patients.
6. The MFEV1 is directly correlated with histology at level (squamous cell carcinoma=2) (P=0.1088), implying that MFEV1 is higher at level squamous cell carcinoma=2, than the other levels of SIIINSCLC patients.
7. The MFEV1 is directly associated with the N-stage at level (N2=3) (P=0.1440) and (N3 or Nx=4) (P=0.0142), indicating that MFEV1 is higher at levels (N2=3) and (N3 or Nx=4), than the other levels of SIIINSCLC patients.
Dispersion model of FEV1 (Table 2) of SIIINSCLC patients interprets the following:
1. The FEV1 variance (FEV1V) is positively partially associated with the age (P=0.1282), indicating that FEV1V is higher at older ages, and vice versa.
2. The FEV1V is inversely partially related with smoking status (Smok2) (P=0.2985), indicating that FEV1V is higher for non-smoker/ex-smokers of SIIINSCLC patients, than the current smokers.
3. The FEV1V is inversely significantly related with PLNS (i.e., number of positive lymph node stations) (P=0.0017), indicating that FEV1V increases as PLNS increases.
4. The FEV1V is reciprocally related with T-stage at level (T2=2) (P=0.0172) and (T4 or Tx=4) (P=0..0240), indicating that FEV1V is higher at levels (T2=2) and (T4 or Tx=4).
5. The FEV1V is reciprocally partially related with equivalent dose (Equd) (P=0.1822), indicating that FEV1V decreases as the equivalent dose increases.
6. The FEV1V is reciprocally related with gross tumor volume (Gtvl) (P=0.0003), indicating that FEV1V decreases as the Gtvl increases.
7. The FEV1V is reciprocally related with survival time in month (Survmonth) (P=0.0451), indicating that FEV1V is decreases as the Survmonth increases.
Conclusion
In the current report, the determinants of FEV1 of SIIINSCLC patients have been determined (Table 2). In the interpretation section, effects of the determinants have been focused. Many determinants of FEV1 have been derived in Table 2, which are almost new in lung-cancer literature. The present report shows that age, BMI, equivalent dose, tumor volume, survival time in month, location of tumors, smoking status, chemo-group, T-stage, N-stage, histology, number of positive lymph node stations (Table 2) are the important determinants of FEV1 of SIIINSCLC patients, which are little focused in earlier research reports. Care should be taken on equivalent dose applying. Lung cancer patients and medical lung cancer specialists will be benefited from the present research.
Conflict of interest
The authors confirm that this article content has no conflict of interest.
References
- Jain NB, Brown R, Tun CG, et al. Determinants of Forced Expiratory Volume in 1 Second (FEV1), Forced Vital Capacity (FVC), and FEV1/FVC in Chronic Spinal Cord Injury. Arch Phys Med Rehabil. 2006;87(10):1327-33.
- Linn WS, Spungen AM, Gong H, et al. Forced vital capacity in two large outpatient populations with chronic spinal cord injury. Spinal Cord. 2001;39:263-8.
- Linn WS, Spungen AM, Gong H, et al. Smoking and obstructive lung dysfunction in persons with chronic spinal cord injury. J Spinal Cord Med. 2003;26:28-35.
- Spungen AM, Grimm DR, Schilero G, et al. Relationship of respiratory symptoms with smoking status and pulmonary function in chronic spinal cord injury. J Spinal Cord Med. 2002;25:23-7.
- Crapo RO, Morris AH, Clayton PD, et al. Lung volumes in healthy nonsmoking adults. Bull Eur Physiopathol Respir. 1982;18:419-25.
- Siegel R, Ma J, Zou Z, et al. Cancer statistics. CA Cancer J Clin. 2014;64:9-29.
- Berghmans T, Paesmans M, Sculier JP. Prognostic factors in stage III non-small cell lung cancer: A review of conventional, metabolic and new biological variables. Ther Adv Med Oncol. 2011;3:127-38.
- Fowler JF. Biological factors influencing optimum fractionation in radiation therapy. Acta Oncol. 2001;40:712-7.
- Solan MJ, Werner-Wasik M. Prognostic factors in non-small cell lung cancer. Semin Surg Oncol. 2003;21:64-73.
- Burnham KP, Anderson DR. Model selection and multimodal inference. NY, USA: Springer Science & Business Media. 2002.
- Oberije C, Ruysscher DD, Houben R, et al. A validated prediction model for overall survival from stage III non-small cell lung cancer: Toward survival prediction for individual patients. Int J Radiation Oncol Biol Phys. 2015;92(4):935-44.
- Das RN, Mukherjee S. Mean-variance overall survival time fitted models from stage III non-small cell lung cancer. Epidemiology (Sunnyvale). 2017;7(1):296.
- Firth D. Multiplicative errors: log-normal or gamma? J R Statist Soc B. 1988;50(2):266-8.
- Das RN, Lee Y. Log-normal versus gamma models for analyzing data from quality improvement experiments. Quality Engineering. 2009;21(1):79-87.
- Lee Y, Nelder JA, Pawitan Y. Generalized linear models with random effects (Unified Analysis via H-likelihood). London: Chapman & Hall. 2006.
- Das RN. Discrepancy in fitting between log-normal and gamma models: An illustration. Model Assisted Statistics and Applications. 2012;7(1):23-32.
- Das RN. Robust response surfaces, regression, and positive data analyses. Chapman & Hall, London. 2014.
- Hastie T, Tibshirani R, Friedman J. The elements of statistical learning. Springer-Verlag, NY, USA. 2001.