Research Article - Journal of Intensive and Critical Care Nursing (2023) Volume 6, Issue 2
Factors associated with increased nursing workload in a pediatric ICU: A prospective observational cohort study.
Alexandra Stavroula Nieri1*, Georgia Sinani2, Evaggelia Asimina2, Eleni Spithouraki1, Stavrina Ilia2, Margarita Giannakopoulou1
1Department of Nursing, National and Kapodistrian University of Athens, Athens, Greece
2Department of Nursing, University Hospital of Heraklion, Crete, Greece
- Corresponding Author:
- Alexandra Stavroula Nieri
Department of Nursing,
National and Kapodistrian University of Athens,
Athens,
Greece,
E-mail: alexandranieri@hotmail.gr
Received: 13-Feb-2023, Manuscript No. AAICCN-23-89261; Editor assigned: 17-Feb-2023, PreQC No. AAICCN-23-89261 (PQ); Reviewed: 03-Mar-2023, QC No. AAICCN-23-89261; Revised: 31-Mar-2023, Manuscript No. AAICCN-23-89261 (R); Published: 28-Apr-2023, DOI: 10.35841/aaiccn-6.2.136
Citation:Nieri AS, Sinani G, Asimina E, et al. Factors associated with increased nursing workload in a pediatric ICU: A prospective observational cohort study. J Intensive Crit Care Nurs. 2023;6(2):136
Abstract
Introduction: NW is related to the quality of care provided in the ICUs, as it was found that increased NW affects negatively both patient safety and nursing outcomes. The identification of the factors that influence the NW is particularly important, as it helps to improve care. However, it has not been investigated which factors influence the NW in Pediatric Intensives Care Units (PICU).
Aim: To assess the NW in the PICU, as well as to investigate the factors with increased NW.
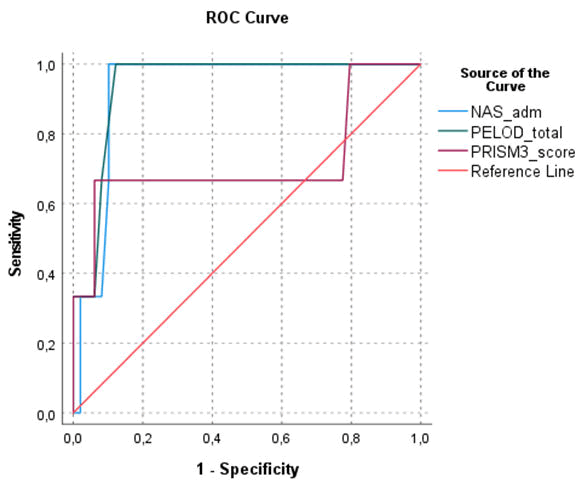
Methods: A prospective and observational study was performed in one PICU (6-bed PICU and 1-bed for short-term care) in Greece from the 1st of July to the 31st of December 2021. NW was assessed daily for each patient with the P-NAS scale, while clinical severity was assessed on the 1 st day of patients' hospitalization using the Pediatric Risk of Mortality IV (PRISM IV) score and Paediatric Logistic Organ Dysfunction 2 (PELOD-2) score. Descriptive analyses, correlation study with parametric and Area under the Receiver Operating Characteristic Curve (AUC-ROC) were performed, with statistical significance α=0.05.
Results: The study sample consisted of 55 patients (60% boys; median age: 3.72 (0.69-11.78) years) and 684 NW records were performed. Four (7.3%) children died. The mean scores of P-NAS on admission, on discharge, and in total records were 83.87 (± 22.42), 72.87 (± 22.93) and 27.41 (± 7.01), respectively. The NW on admission had statistically significant correlation the PRISM IV score IV (rho=0.371, p=0.007) and PELOD-2 (rho=0.631, p<0.001). The AUC-ROC of NAS for predicting death of critically ill children was 0.929 (0.849, 1.008). The admission from another hospital (p<0.001), the emergency admission (p<0.001), and the diagnostic category of trauma (p=0.028) were associated with increased NW on admission. Moreover, department (p<0.001) and type of admission (p<0.001) and the existing of comorbidities (p<0.001) were associated with increased daily NW in PICU.
Conclusion: The P-NAS are reliable and valid tool for the assessment of NW in PICU. The P-NAS had good discrimination in predicting mortality in critically ill children. Prognostic factors of high workload were the severity scores, the coming from another hospital, the trauma diagnosis, and the emergency admission.
Keywords
Pediatric intensives care units, Pediatric risk of mortality, Prognostic factors, Diagnosis.
Introduction
The Pediatric Intensive Care Unit (PICU) is a special ward that provides specialist care in infants, children, and adolescents with possible or existing life-threatening illnesses or injuries. In the context of the holistic nursing approach, the care provided includes not only the children, but their families as well as. The high demands of daily practice in the PICU lead nurses to an increased nursing workload [1].
Nursing Workload (NW) is defined as the total time required to perform nursing activities in a specific period of time. NW is related to the quality of care provided in the ICUs, as it was found that increased NW affects negatively both patient safety and nursing outcomes. Moreover, increased patients to nurses ratio in ICU is associated with higher rates of hospital acquired infections, increased length of stay and higher mortality rates. However, the staffing process is one of the most important problems of any health organization, since staff payroll costs are the largest expense in the majority of health care budgets, especially in PICUs, where the nurse-to-patient ratio is higher than in general medical and surgical ward [2].
The assessment of NW is necessary to investigate the interaction of nurses with patients, and for hospital budget estimation, treatment planning and cost-effectiveness analyzes in ICUs. Nowadays, several measurement systems have been developed for the assessment of the NW in ICUs, focusing on the needs and severity of the patients' condition. The most commonly used systems are the Therapeutic Intervention Scoring System (TISS-28), the Nursing Activities Score (NAS) and the Nine Equivalents of Nursing Manpower use score (NEMS).
The assessment of the NW in PICUs with the above systems has been the subject of few studies. In Greece, the NW in PICU has been assessed in only one study with the Pediatric version of NAS (P-NAS) and the TISS-28 for 5 weeks. In our country, no system is used for the nursing staffing of PICUs, so it is important to investigate the usefulness of the NW scales in the assessment of the NW and the calculation of the required staffing to provide high quality care. Moreover, the factors associated with increased NW in PICUs have not been adequately examined. Therefore, the purpose of the present study was to implement the P-NAS in order to measure the NW in hospitalized patients in a Greek PICU. Additionally, the current study investigated the factors associated with increased NW in PICU [3,4].
Materials and Methods
Study design and population
This prospective and observational cohort study was conducted in one University PICU (6-bed PICU and 1-bed for short-term care), which is located in the inner area of Heraklion (Crete), from the 1st of July to the 31st of December 2021. The study population included all patients, who were admitted to the PICUs during the study period. We excluded patients staying in the ICU for <8 h. From 104 patients were hospitalized in the PICU during the study period, 49 patients were excluded because they were stayed in the PICU for less than 8 hours. Therefore, the study sample consisted of 55 patients. Two patients were over 18 years of age; however, we did not exclude them from the study, because ΝW scales are valid tools for the assessment of NW in adult ICUs [5].
Data collection
The nursing workload was assessment using Pediatric version of Nursing Activities Score (PNAS). The P-NAS have been validated in Greek PICU in a previous study. NAS consists of 23 items that assess the routine activities performed by the nurses looking after critically ill patients. NAS score represents the percentage of the time the nursing staff needs to perform the care-related tasks per ICU patient per 24 hours. The total NAS score ranges from 0% to 177%, and each NAS point corresponds to 14.4 min of nursing care. The assessment of NW was performed daily for each hospitalized patient. We performed a total of 684 measurements with the P-NAS scale [6].
Moreover, the Pediatric Risk of Mortality ΙV (PRISM IV) score and Paediatric Logistic Organ Dysfunction 2 (PELOD-2) score was used to assess the severity of the patients. For the PRISM-IV score, the laboratory data (PaO2, PaCO2, PT, aPTT, serum urea nitrogen, serum potassium, serum creatinine, blood glucose, and serum bicarbonate levels, white blood cell and platelet counts) were collected for the 2 hrs before admission to 4 hrs after admission. The other physiologic variables (temperature, systolic blood pressure, heart rate, GCS score, pupillary reaction) were collected for the first 4 hrs of PICU care. The PELOD-2 score evaluates five organ systems (neurologic, cardiovascular, respiratory, renal, and hematologic) using 10 variables (GCS score, pupillary reaction, lactatemia, mean arterial blood pressures, PaO2/FiO2 ratio, PaCO2, invasive ventilation, creatinine level, white blood cell count, and platelet count). For variables that were measured more than once within 24 hrs of admission, the worst values for the day were selected for calculating the PELOD-2 [7].
In addition, a form was used to record the demographic and clinical data of patients admitted to the PICU. The data were recorded by one researcher, non-PICU staff member, and 2 PICU nurses. Data collection was performed through observation of the pediatric patients and the medical/nursing records.
Data analysis
All statistical analyses were performed using Statistical Program for Social Science (SPSS) version 28.0 and STATA version 13.0. Categorical variables are presented as absolute (Ν) and relative (%) frequencies. Continuous variables are expressed as mean (± Standard Deviations (SDs)) or medians (Interquartile Ranges (IQRs)). The normality assumption for continuous variables was evaluated by using the normal Q-Q plots and normality test. In order to compare NW with demographic and clinical characteristics, we used: a) t-test or Mann-Whitney test to compare the quantitative variable between the two groups, depending on whether the quantitative variable followed the normal distribution, b) the ANOVA test or the Kruskal Wallis test to compare the quantitative variable between the three or more groups, depending on whether the quantitative variable followed the normal distribution, c) the Pearson's coefficient or the Spearman coefficient (rho) between quantitative variables. Moreover, for the prediction ability of the P-NAS and the clinical severity scores in predicting the patients’ outcome in the PICU, the Area under the Receiver Operating Characteristic Curve (AUC-ROC) was calculated. Acceptable discrimination is represented by an area under the curve of 0.70-0.79, good discrimination by an area ≥ 0.80, and excellent discrimination by an area ≥ 0.90. The level of statistical significance set at α=0.05 [8].
Results
Demographic and clinical characteristics of patients
The study sample consisted of 55 patients who were hospitalized in the PICU for at least 24 hours. Of the 55 patients, 33 (60.0%) were male. The median age of the patients was 3.72 (0.69-11.78) years. The observed mortality was 7.3%. The mean PELOD II score was 3.50 (± 4.15) and PRISM IV score 5.79 (± 5.76). Additional demographic and clinical data of the sample are presented in Table 1.
| Demographic and clinical characteristics | |
| Gender, Ν (%) | |
| Male | 33 (60.0) |
| Female | 22 (40.0) |
| Age (years), Median (IQR) | 3.72 (0.69 – 11.78) |
| Age categories, Ν (%) | |
| Infants | 17 (30.9) |
| Children | 25 (45.5) |
| Adolescent | 11 (20.0) |
| Adults | 2 (3.6) |
| Department of origin, N (%) | |
| Emergency department | 11 (20.0) |
| Ward | 15 (27.3) |
| Surgery | 14 (25.5) |
| Another hospital | 15 (27.3) |
| Type admission, N (%) | |
| Elective | 17 (30.9) |
| Emergency | 38 (69.1) |
| Type of patient, N (%) | |
| Medical | 31 (56.4) |
| Surgical | 15 (27.3) |
| Trauma | 9 (16.4) |
| Comorbidities, N (%) | |
| No | 32 (58.2) |
| Yes | 23 (41.8) |
| PRISM III/IV score, Mean (±SD) | 5.79 (± 5.76) |
| PELOD II, Mean (±SD) | 3.50 (± 4.15) |
| Length of stay in PICU (days), Median (IQR) | 5.00 (3.00-16.00) |
| Outcome, N (%) | |
| Survival | 51 (92.7) |
| Death | 4 (7.3) |
Nursing workload
The mean P-NAS score, for the total records (N=684), was 76.75 (± 15.18), which corresponded to 1105.27 (± 218.64) minutes of nursing care. The NW on admission was statistically significantly greater than the NW at discharge (p<0.001) (Table 2).
| Workloads | N | P-NAS score mean (± SD) |
|---|---|---|
| Nursing workload in total records | 684 | 27.41 (± 7.01) |
| Nursing workload on admission | 52 | 83.87 (± 22.42) |
| Nursing workload on discharge | 52 | 72.87 (± 22.93) |
Table 2. Nursing workload.
Prognostic ability of P-NAS and severity score for predicting mortality in PICU
The P-NAS score had a positive statistically significant correlation with the PRISM IV (rho=0.371, p=0.007) and PELOD-2 (rho=0.631, p<0.001). ROC curve analysis showed that the AUCs (95% CI) of P-NAS, PRISM IV, and PELOD-2 for predicting death of critically ill children were 0.929 (0.849, 1.008), 0.718 (0.221, 1.214), and 0.942 (0.865, 1.019), respectively (Figure 1).
Comparison of P-NAS score with demographic and clinical characteristics
Table 3 shows the comparison of the demographic characteristics of the patients with the NW on admission and in total records. As shown in the table, the P-NAS score on admission did not differ statistically significantly according to the patients' gender (p=0.557) and age (p=0.080). P-NAS on admission was statistically significantly greater in patients who admitted in PICU emergency than in patients who admitted in elective (93.21 (± 20.51) vs. 64.64 (± 11.15), p<0.001). Furthermore, the P-NAS on admission differed statistically significantly according to the sources of PICU patient admission (p=0.021). More specifically, patients admitted to the PICU from the operating room had a statistically significantly lower P-NAS on admission than those admitted to the PICU from another hospital (70.15 (± 13.11) vs. 93.74 (± 25.83), p=0.025). Also, NAS score on admission differed statistically significantly according to patient type (p=0.016). Specifically, surgical patients had a statistically significantly lower P-NAS on admission than medical patients (p=0.038).
Additionally, the daily P-NAS score was statistically significantly greater in boys than in girls (78.03 (± 15.59) vs. 75.40 (± 14.64), p=0.023). The daily P-NAS differed statistically significantly according to the sources of PICU patient admission (p<0.001), the type of admission (p<0.001), and the existence of comorbidities (p<0.001). More specifically, the patients without comorbidities had a statistically significantly higher daily P-NAS compared to the patients with comorbidities (80.60 (± 17.21) vs. 74.81 (± 13.66), p<0.001).
| Demographic and clinical characteristics | P-NAS on admission | P-NAS in total records | ||||
|---|---|---|---|---|---|---|
| Mean (± SD) | p-value | Mean (± SD) | p-value | |||
| Gender | ||||||
| Male | 31 | 85.16 (±23,57) | 0.557 | 281 | 78.03 (± 15.59) | 0.023 |
| Female | 21 | 81.95 (±21,02) | 279 | 75.40 (± 14.64) | ||
| Age (years) | 52 | 0.245* | 0.08 | 684 | 0.016** | 0.675 |
| Department of origin | ||||||
| Emergency department | 11 | 89.46 (± 17.76) | <0.001 | 102 | 76.64 (± 10.29) | <0.001 |
| Ward | 13 | 83.28 (± 24.55) | 233 | 76.05 (± 10.87) | ||
| Surgery | 14 | 70.15 (± 13.11) | 54 | 67.82 (± 10.67) | ||
| Another hospital | 15 | 93.74 (± 25.83) | 295 | 78.98 (± 19.11) | ||
| Type admission | ||||||
| Elective | 17 | 64.64 (± 11.15) | <0.001 | 196 | 71.31 (± 17.04) | <0.001 |
| Emergency | 35 | 93.21 (± 20.51) | 488 | 78.94 (± 13.79) | ||
| Type of patient | ||||||
| Medical | 28 | 86.73 (± 21.56) | 0.028 | 534 | 76.25 (± 13.99) | 0.202 |
| Surgical | 15 | 73.79 (± 20.72) | 87 | 77.74 (± 19.21) | ||
| Trauma | 9 | 91.76 (± 24.40) | 63 | 79.63 (± 18.20) | ||
| Comorbidities | ||||||
| No | 32 | 83.13 (± 24.31) | 0.592 | 230 | 80.60 (± 17.21) | <0.001 |
| Yes | 23 | 85.05 (± 19.55) | 454 | 74.81 (± 13.66) | ||
Note: **Spearman coefficient; *Pearson coefficient
Table 3. Comparison of P-NAS score with demographic and clinical characteristics.
Discussion
The present study assessed the NW in a PICU and examined the factors associated in with increased NW. For the assessment of NW, we used the P-NAS scale, because it is widely used in foreign health care systems, as it is important tool not for the calculation of the nursing staffing, but also for the cost management. However, international data regarding the P-NAS in PICUs are limited [9].
Another finding of our study was that the P-NAS had acceptable discrimination for predicting of patients’ outcome in PICU. More specifically, the AUC of NAS for predicting death of critically ill children was 0.929 (0.849, 1.008). However, PELOD-2 had better discrimination from the PNAS. This is the first study that reports the performance of PNAS in predicting mortality among critically ill children [10]. Two studies have evaluated the discrimination of nursing workload scoring systems to predict mortality risk in patients admitted to adult ICU. One study showed that the discriminative ability of the TISS was similar to that of APACHE II. Additionally, Nassiff et al found that the NAS has a lower discrimination than the APACHE II. In more details, the AUC was 0.626 (0.570, 0.678) and 0.721 (0.669, 0.769), for NAS and APACHE II, respectively. In a recent metaanalysis, which included 29 studies, it was found that the pooled discrimination performance for the PRISM-III/IV and the PELOD-2 score was 0.84 (95% CI: 0.80-0.87) and 0.83 (95% CI: 0.80-0.86) [11,12].
One of the main findings of this study was that the mean scores of P-NAS on admission, on discharge, and in total records were 83.87 (± 22.42), 72.87 (± 22.93), and 27.41 (± 7.01), respectively. Τhe NW on admission was significantly higher than the NW on discharge. In the study NAS admission scores (59.0 ± 12.0) and the daily NAS scores (56.0 ± 11.0) were lower compared to the findings of the current study. Also found lower P-NAS (62.6 ± 17.3) score on admission in comparison to our study. On the other hand, the mean NAS in adults ICUs, in a review study, has been found to range from 50.4 to 104, with 60% of the total studies obtaining values between 60 and 70. These score differences of NW could be associated to the different politics of management and operation of each PICU [13,14].
Furthermore, in our study was found that the admission from another hospital, the emergency admission, and the diagnostic category of trauma were associated with increased NW. In the study of Romano et al, in 2019, where the sample consisted of 211 patients hospitalized in an adult ICU in Brazil, a statistically significant relationship was found between the type of admission and NW on the 1st day of hospitalization in PICU [15]. In another study, which conducted in 3 adults ICU, it was found that APACHE II, days of stay in ICU ≥ 3, surgical service of provenance, and diagnostic category of traumatology and emergencies were associated with a high NAS score. There are no studies that investigate the factors that influence the NW in PICU [16]. Finally, another finding was the moderatestrength positive correlation between NW on admission and severity scores (PRISM IV, PELOD). The Pediatric Index of Mortality (PIM) score on admission was not a predictor of NW on admission. In contrast, in adult ICUs, it has been found that the Simplified Acute Physiology Score (SAPS) and the Logistic Organ Dysfunction Score (LODS) were predictors of NW on admission to the ICU.
Conclusion
The use of the NAS seems to be particularly important in the clinical practice, and in particular in PICUs, as it enables the assessment of the NW and the optimal nurse to patient ratio. In this way, it is ensured that nursing staff is resourced adequately, and children are receiving safe and high-quality care. Moreover, the P-NAS had good discrimination in predicting mortality in critically ill children. Therefore, the PNAS is a useful and helpful scale to evaluate the severity of critically ill children effectively and accurately in Greek PICUs.
Limitations of the Study
Despite the fact that the current study reached important conclusions about NW in PICU, it is nevertheless characterized by a number of limitations. The present study was carried out in one PICU in Athens, thus ensuring homogeneity in terms of the nursing care provided, however, the fact that patients from other PICUs were not included in the study sample may cause some degree of limitation as towards the generalization of the results. Also, there was no randomization of the time period of its conduct, resulting in bias error of the possible seasonal variation of the NW. Additionally, the main researcher was not a member of the staff in the PICU and the recording of the NW scales was done once every 24 hours. This may have resulted in the underestimation of NW, in cases of poor documentation of nursing interventions, in the patients' files, from where the data were collected.
Ethical Approval
The research was carried out in accordance to Helsinki’s declaration and the General Data Protection Regulation (GDPR) 2016/679. The protocol was approved by the ethics committee of the department of nursing, national and Kapodistrian university of Athens (Register number: 180), and by the ethics committees of the PICU hospital (Register numbers: 14448/22-10-2019). Due to the observational nature of the study and the anonymization of the data, the written consent of patients or relatives was not required.
Acknowledgment
The research work was supported by the Hellenic Foundation for Research and Innovation (HFRI) under the HFRI PhD fellowship grant (Fellowship number: 1524).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Bae SH. Intensive care nurse staffing and nurse outcomes: A systematic review. Nurs Crit Care. 2021;26(6):457-66.
[Crossref] [Google Scholar] [PubMed]
- Campagner AO, Garcia PC, Piva JP. Use of scores to calculate the nursing workload in a pediatric intensive care unit. Rev Bras Ter Intensiva. 2014;26(1):36-43.
[Crossref] [Google Scholar] [PubMed]
- Carlson RV, Boyd KM, Webb DJ. The revision of the declaration of Helsinki: Past, present and future. Br J Clin Pharmacol. 2004;57(6):695-713.
[Crossref] [Google Scholar] [PubMed]
- Chang LY, Yu HH, Chao YF. The Relationship between nursing workload, quality of care, and nursing payment in intensive care units. J Nurs Res. 2019;27(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Coyne I. Families and health?care professionals' perspectives and expectations of family?centred care: Hidden expectations and unclear roles. Health Expect. 2015;18(5):796-808.
[Crossref] [Google Scholar] [PubMed]
- Fagerstrom L, Kinnunen M, Saarela J. Nursing workload, patient safety incidents and mortality: An observational study from Finland. BMJ Open. 2018;8(4):e016367.
[Crossref] [Google Scholar] [PubMed]
- Fasoi G, Patsiou EC, Stavropoulou A, et al. Assessment of nursing workload as a mortality predictor in Intensive Care Units (ICU) using the Nursing Activities Score (NAS) scale. Int J Environ Res Public Health. 2021;18(1):79.
[Crossref] [Google Scholar] [PubMed]
- Frey B, Hossle JP, Sigrist MS, et al. Measurement of resident workload in paediatric intensive care. Swiss Med Wkly. 2013;143(3536):w13844.
[Crossref] [Google Scholar] [PubMed]
- Kung E, Waldhor T, Rittenschober-Bohm J, et al. Increased nurse workload is associated with bloodstream infections in very low birth weight infants. Sci Rep. 2019;9(1):6331.
[Crossref] [Google Scholar] [PubMed]
- Leteurtre S, Duhamel A, Salleron J, et al. PELOD-2: An update of the PEdiatric logistic organ dysfunction score. Crit Care Med. 2013;41(7):1761-73.
[Crossref] [Google Scholar] [PubMed]
- Miranda DR, de Rijk A, Schaufeli W. Simplified therapeutic intervention scoring system: The TISS-28 items--results from a multicenter study. Crit Care Med. 1996;24(1):64-73.
[Crossref] [Google Scholar] [PubMed]
- Miranda DR, Nap R, de Rijk A, et al. Nursing activities score. Crit Care Med. 2003;31(2):374-82.
[Crossref] [Google Scholar] [PubMed]
- Nassiff A, Araujo TR, Menegueti MG, et al. Nursing workload and patient mortality at an intensive care unit. Texto Contexto-Enfermagem. 2018;27(4).
- Needham J. Accuracy in workload measurement: A fact or fallacy? J Nurs Manag. 1997;5(2):83-7.
[Crossref] [Google Scholar] [PubMed]
- Nieri AS, Manousaki K, Kalafati M, et al. Validation of the nursing workload scoring systems “Nursing Activities Score”(NAS), and “Therapeutic Intervention Scoring System for Critically Ill Children”(TISS-C) in a Greek paediatric intensive care unit. Intensive Crit Care Nurs. 2018;48:3-9.
[Crossref] [Google Scholar] [PubMed]
- Padilha KG, Stafseth S, Solms D, et al. Nursing activities score: An updated guideline for its application in the intensive care unit. Rev Esc Enferm USP. 2015;49:131-7.
[Crossref] [Google Scholar] [PubMed]