Research Article - Journal of Clinical Ophthalmology (2023) Volume 7, Issue 4
Eyecare practices and glaucoma patient care trends in the face of a global pandemic, COVID-19
Mustafa Safi1, Katayun Fethat2, Jason Bacharach1,3*
1Department of Ophthalmology, California Pacific Medical Center, San Francisco, California, United States of America
2University of California, Davis, California, United States of America
3North Bay Eye Associates, Petaluma, California, United States of America
- Corresponding Author:
- Dr. Jason Bacharach
Clinical Instructor and Chief of Glaucoma Division
California Pacific Medical Center
San Francisco
California
United States of America
E-mail: jb@northbayeye.com
Accepted date: 25 March, 2021
Citation:Safi M, Fethat K, Bacharach J. Eyecare practices and glaucoma patient care trends in the face of a global pandemic, Covid-19. J Clin Ophthalmol 2021;5(S3):381-385.
Abstract
Objective: To understand the effects of the COVID-19 pandemic on glaucoma eyecare practices and patient care trends.
Design: Cross-sectional
Participants: Comprehensive and glaucoma trained ophthalmologists
Method: This was an internet-based statewide survey distributed to comprehensive and glaucoma-trained ophthalmologists in California. The survey consisted of 10 questions designed to address the effect of the pandemic on the volume of patient care visits, laser utilization, teleophthalmology trends, and frequency of routine, urgent and emergent glaucoma surgical procedures, among others.
Main outcome measure: Not-applicable
Results: Most ophthalmologists reported decreased patient volume as they focused primarily on seeing urgent and emergent glaucoma cases. While most respondents noted a significant decrease in routine surgical procedures, a majority reported a similar volume of urgent and emergent procedures comparable to the pre-COVID-19 era. Notably, most ophthalmologists responded that they did not change their prescription filling habits during the pandemic. Selective laser trabeculoplasty (SLT) utilization decreased, paralleling the reported decrease in patient volume. Finally, just over half of the ophthalmologists surveyed implemented teleophthalmology into their practice.
Conclusion: Discovering patient care trends shed light on areas of needed advancement, such as teleophthalmology, and provides necessary insight into how ophthalmologists are coping with the challenges brought on by the pandemic.
Keywords
Coronavirus, Teleophthalmology, Glaucoma, Pandemic.
Introduction
In December 2019, in Wuhan City, Hubei Province, China, the Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCoV- 2) was first isolated [1]. It has since spread relentlessly throughout the world, with the World Health Organization (WHO) declaring it a pandemic as of March 11, 2020 [2]. Despite the development of a vaccine approved for mass production and utilization in the general population in an unprecedented short interval of time, the pandemic maintains a chokehold on the economic and medical infrastructure of nations worldwide, with recent surges in the number of confirmed cases and related deaths [3].
COVID-19 is a highly contagious virus and spreads via respiratory droplets among persons in close contact and possibly from contaminated surfaces [4]. As such, many business operations within eyecare have been severely affected by it and, in many instances, required to halt all operation [5]. In the healthcare domain, ophthalmology is one of a handful of specialties severely affected by COVID-19. Notably, elective surgical procedures have stopped for the most part and some practices have limited in-person visits to decrease the risk of exposure to the ophthalmologist and associated staff [6].
In the setting of chronic ocular diseases such as glaucoma, in which in-person office visits are of critical importance in making therapeutic adjustments such as adding additional pressure-lowering drops, laser treatment, and/or ultimately surgery, it is yet to be determined how COVID-19 has altered outcomes for these patients. We conducted a statewide survey to better understand the effect of the COVID-19 pandemic on glaucoma eyecare practices and patient care trends in glaucoma management.
Materials and Methods
A cross-sectional, internet-based, anonymous survey using Google Forms was distributed and administered to ophthalmologists in California. Emails were sourced from the American Academy of Ophthalmology website and Google Search. Participants were screened based on their practice specialty and selected if they were a comprehensive or glaucoma specialist. The survey consisted of 10 multiple-choice questions. Questions were created to address changes in prescription refill habits, selective laser trabeculoplasty utilization, telemedicine attitudes, volume of patients seen, and routine, and urgent surgical procedures performed. Not all of the questions required a response, and not all participants answered all questions.
Institutional review board approval was not required. The research adheres to the tenets of the Declaration of Helsinki.
Results
470 surveys were distributed, of which 79 responses were obtained (16.81%). The majority of respondents were from private practices (72.2%, n=57), followed by major academic centers (16.5%, n=13), and hybrid practices (11.4%, n=9). Furthermore, the bulk of ophthalmologists reported practicing in urban (53.2%, n=42) and suburban (38.0%, n=30) environments, while few (8.9%, n=7) reported practicing in rural settings. Regardless of the environment or type of practice, patient volume was impacted during the COVID-19 pandemic, as 78.5% (n=62) of ophthalmologists reported that they only saw urgent and emergent cases.
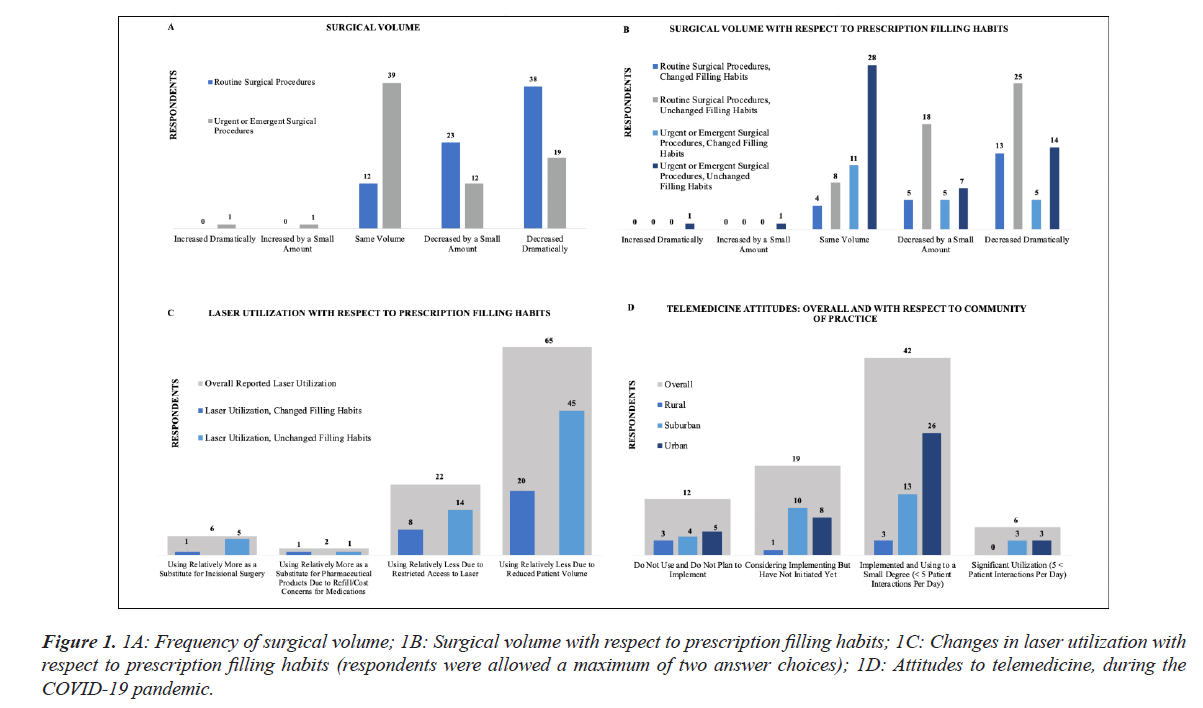
The majority of surveyed ophthalmologists reported a dramatic decrease in routine glaucoma procedures (52.1%, n=38) and reduced laser utilization (90.3%, n=65) during the pandemic. However, respondents reported that the volume of urgent and emergent glaucoma procedures (54.2%, n=39) and prescription filling habits (70.9%, n=56) remained unchanged.
When examining the interplay between prescription refills and procedures, most respondents reported a dramatic decrease in routine glaucoma procedures regardless if the practice changed their prescription filling habits (56.52%, n=13) or not (44.64%, n=25). However, 47.83% (n=11) of ophthalmologists who changed their prescription habits and 50.0% (n=28) of those who did not, noted that their urgent and emergent glaucoma surgical volume remained the same. This result was not expected or intuitive as we expected an increase in prescription volume as surgical case volume decreased.
Furthermore, 86.96% (n=20) of respondents who changed their prescription habits, and 80.36% (n=45) who did not, reported reduced laser utilization due to reduced patient volume. Notably, 8.93% (n=5) of practices that did not adjust their refill habits reported relatively more laser utilization as a substitute for incisional surgery. In comparison, only 4.34% (n=1) of practices that had altered their prescription writing habits reported the same.
Regarding implementation of teleophthalmology services, 53.2% (n=42) of ophthalmologists started using this as an alternative to in-person visits with an average of less than 5 patients per day. 61.9% (n=26) of those were from urban practices, 43.3% (n=13) from suburban practices, and 42.86% (n=3) from rural based practices. Nearly half (42.86%, n=3) of respondents from rural environments did not plan to implement teleophthalmology, and neither did 13.33% (n=4) of those from suburban and 11.90% (n=5) of those from urban environments. Refer to Tables 1-3 and Figure 1 regarding the aforementioned data.
| Type of Practice | Community of Practice | Change in patient volume | Change in prescription refill habits | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Respondents | Frequency (%) | Respondents | Frequency (%) | Respondents | Frequency (%) | Respondents | Frequency (%) | ||||
| Private | 57 | 722% | Rural | 7 | 8.90% | Unchanged | 0 | 0% | No | 56 | 70.90% |
| Major Academic Center | 13 | 16.50% | Urban | 42 | 53.20% | Minor Reduction in Volume | 15 | 19% | Yes | 23 | 29.10% |
| Hybrid | 9 | 11.40% | Suburban | 30 | 38.00% | Only Seeing Urgent or Emergent Cases | 62 | 78.50% | Declined to Respond | 0 | 0% |
| Declined to Respond | 0 | 0% | Declined to Respond | 0 | 0% | Completely Stopped Seeing Patients | 2 | 2.50% | |||
Table 1: Frequency of type and community of practice, volume of patients seen, prescription refill habits.
| Change in Volume of Routine Surgical Glaucoma Procedures | Change in Volume of Urgent or Change in Volume of Routine Surgical Glaucoma Procedures | Change in Volume of Routine Surgical Glaucoma Procedures With Respect to Prescription Filling Habits | Change in Volume of Urgent or Change in Volume of Routine Surgical Glaucoma Procedures With Respect to Prescription Filling Habits | |||||
|---|---|---|---|---|---|---|---|---|
| Respondents | Frequency (%) | Respondents | Frequency (%) | Changed filling habits | Did not change filling habits | Changed filling habits | Did not change filling habits | |
| Respondents | Frequency (%) | Respondents | Frequency (%) | |||||
| Increased Dramatically | 0 | 0% | 1 | 1.40% | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.79%) |
| Increased by a Small Amount | 0 | 0% | 1 | 1.40% | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.79%) |
| Same Volume | 12 | 16.40% | 39 | 54.20% | 4 (17.39%) | 8 (14.29%) | 11 (47.83%) | 28 (50.00%) |
| Decreased by a Small Amount | 23 | 31.50% | 12 | 16.70% | 5 (21.74%) | 18 (32.14%) | 5 (21.74%) | 7 (12.50%) |
| Decreased Dramatically | 38 | 52.10% | 19 | 26.40% | 13 (56.52%) | 25 (44.64%) | 5 (21.74%) | 14 (25.00%) |
| Declined to Respond | 6 | 7.59% | 7 | 8.86% | 1 (4.35%) | 5 (8.93%) | 2 (8.700%) | 5 (8.93%) |
Table 2: Change in volume of urgent or change in volume of routine surgical glaucoma procedures with respect to prescription filling habits.
| Respondent's laser utilization* | Laser utilization with respect to prescription filling habits* | Change in attitudes relative to telemedicine utilization during COVID-19 | Change in attitudes relative to telemedicine utilization with respect to community of practice | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Respondents | Frequency (%) | Changed Filling Habits | |||||||
| Respondents | Respondents | Frequency (%) | Rural (Respondents, Frequency (%)) | Suburban (Respondents, Frequency (%)) | Urban (Respondents, Frequency (%)) | ||||
| Using Relatively More as a Substitute for lncisional Surgery | 6 | 8.30% | 1 (4.34%) | Do Not Use and Do Not Plan to Implement | 12 | 15.20% | 3 (42.86%) | 4 (13.33%) | 5 (11.90%) |
| Using Relatively More as a Substitute for Pharmaceutical Products Due to Refill/Cost Concerns for Medications | 2 | 2.80% | 1 (4.34%) | Considering Implementing But Have Not Initiated Yet | 19 | 24.10% | 1 (14.29%) | 10 (33.33%) | 8 (19.05%) |
| Using Relatively Less Due to Restricted Access to Laser | 22 | 30.60% | 8 (34.78%) | Implemented and Using to a Small Degree (<5 Patient Interactions Per Day) | 42 | 53.20% | 3 (42.86%) | 13 (43.33%) | 26 (61.90%) |
| Using Relatively Less Due to Reduced Patient Volume | 65 | 90.30% | 20(86.96%) | Significant Utiliz.at ion (>5 Patient Interactions Per Day) | 6 | 7.60% | 0 (0%) | 3 (10.00%) | 3 (7.14%) |
| Declined to Respond | 7 | 8.86% | 1 (4.34%) | Declined to Respond | 0 | 0% | 0 (0%) | 0 (0%) | 0 (0%) |
Table 3: Selective laser trabeculoplasty (SLT) utilization, telemedicine attitudes, routine and urgent surgical procedures performed with respect to change in volume of routine and urgent or emergent glaucoma surgical procedures.
Figure 1: 1A: Frequency of surgical volume; 1B: Surgical volume with respect to prescription filling habits; 1C: Changes in laser utilization with respect to prescription filling habits (respondents were allowed a maximum of two answer choices); 1D: Attitudes to telemedicine, during the COVID-19 pandemic.
Discussion
The COVID-19 pandemic had a significant impact on medicine. While some specialties during this time such as ICU and ER physicians had a surge in the number of patients they cared for, others, such as ophthalmology, were negatively impacted.
Our study found a significant decrease in patient volume, with most practitioners focusing primarily on seeing urgent and emergent cases. We expected this outcome given the chronic and vision-threatening nature of glaucoma, leaving patients vulnerable to vision loss if left untreated in uncontrolled situations. Furthermore, in light of seeing a decrease in patient volume, only about a third of practitioners changed their prescription habits. For the near 70% of ophthalmologists who did not change their prescription habits, the reason is unclear. Perhaps their patients' glaucoma was deemed stable, manageable by their current glaucoma eye drop regimen, thus not requiring any changes. We expected to see an increased volume of pharmaceutical prescriptions as surgical volume dropped.
Clinical implications of reduced in-person surveillance of glaucoma patients during the height of the pandemic are yet to be determined. In addition to the IOP, other clinical variables are assessed and considered in making therapeutic adjustments in glaucoma management, including both structural and functional evaluations. Additional long-term post-pandemic outcomes studies will be needed to see if the reduction in inperson visits resulted in a negative effect on patient outcomes due to glaucoma progression.
Implementation of remote evaluation using the currently available telehealth applications for ophthalmology may be impractical in glaucoma management. Technology to do basic parts of the evaluation such as remote monitoring of the intraocular pressure, as well as structural and functional evaluation of the optic nerve is not readily available. Thus, it should not be surprising that nearly 40% of practitioners had not incorporated teleophthalmology in their practice. In addition, there may be cultural impedance to remote care. It has been previously reported that a majority of ophthalmologists were not comfortable with delivering patient care remotely [7]. However, approximately 53% of ophthalmologists had implemented teleophthalmology in some fashion, likely to evaluate patients for tolerability and side effects of drops, modification to prescriptions, and to determine if an in-person visit is necessary [8]. Perhaps more sophisticated tools and Artificial Intelligence (AI) software will be developed in the future which would allow the ophthalmologist to evaluate and manage glaucoma remotely [9,10]. One example would be having patients self-measure IOP and physicians review results remotely. A recent report using the IcareONE rebound tonometer providing similar measurements to the physicians' IOP measurements with the Goldman applanation tonometer is encouraging [9]. Advancements in AI is also encouraging. An example is Pegasus, which accurately detected glaucomatous optic neuropathy approximately 83% of the time [10]. The average accuracy of this system was similar to that of ophthalmologists and optometrists although more testing with Pegasus on a larger patient population is needed before mass utilization [10].
Although we expected to find an increased utilization of Selective Laser Trabeculoplasty (SLT) laser during the height of the pandemic shut down, the rate of SLT use went down significantly due to the decreased patient volume. This finding was in spite of the LiGHT study demonstrated that SLT is an effective treatment option in the management of glaucoma [11]. If a reduction in SLT is a marker for delay in introducing any glaucoma treatment, that could potentially lead to significant and permanent blindness [12,13]. Interestingly, reduced rates of laser treatment were also seen in other subspecialties during the pandemic [14].
Similarly, the frequency of routine glaucoma procedures also saw a significant impact, with over 50% of respondents noting a decrease in routine surgical glaucoma procedures. This is consistent with a study that reported a significant reduction in elective surgical procedures in the United Kingdom during the pandemic compared to the year before [15]. The UK report also hypothesized a reduction in surgical volume was likely a result of decreased patient volume. Many factors could be implicated as causal ranging from the patient's concern over their face masks interfering with their appointment to practitioners down booking clinic out of fear of contracting the virus from the patient [16,17].
On the other hand, urgent and emergent surgical glaucoma procedure volume remained relatively stable. Approximately 78% of ophthalmologists were primarily seeing urgent and emergent patients. Over half of those ophthalmologists did not report a change in the volume of urgent and emergent glaucoma procedures. Our data is consistent with a study in India where approximately 82% of ophthalmologists who were still seeing patients during the lockdown only saw urgent or emergent cases [5].
Our study has limitations. The first is the study's low response rate. At the time of survey distribution, many ophthalmology offices were closed and/or significantly reduced their hours of operation. Thus, many providers may not have accessed their business emails or found completing the survey a priority. The second limitation concerns the overall study design. While this study was a descriptive survey-based cross-sectional study, perhaps future studies will use a quantitative study design, with more specific questions to measure the pandemic's effects. Another limitation is based on possible regional disparity in response to the pandemic. California implemented an early lockdown which could have resulted in a more draconian response in reduction in eyecare. Therefore, future studies should distribute surveys throughout the United States to discover the pandemic's national effect on ophthalmology, which would allow for better generalizability.
Conclusion
The COVID-19 pandemic had a significant impact on ophthalmology practices. While this study uncovered that many ophthalmologists saw urgent and emergent cases to the same degree as before the pandemic, the number of routine surgical procedures and laser utilization significantly decreased. Also, many ophthalmologists have not incorporated teleophthalmology into their practices. Our research and the pandemic in general, underscored the need for reliable and accurate teleophthalmology options for both practitioners and their patients.
Conflict of Interest
There is no financial conflict of interests to disclose. Each author participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Financial Support
Funding was provided by the Pacific Vision Foundation, San Francisco, CA, and the California Pacific Medical Center, San Francisco, CA
References
- Shi Y, Wang G, Cai XP, et al. An overview of COVID-19.J Zhejiang Univ Sci B. 2020;21:343-60.
- WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. World Health Organization.
- COVID Data Tracker. Centers for Disease Control and Prevention.
- Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak.J Autoimmun. 2020;109:102433.
- Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey.Indian J Ophthalmol. 2020;68:725-30.
- Williams AM, Kalra G, Commiskey PW, et al. Ophthalmology practice during the coronavirus disease 2019 pandemic: The University of Pittsburgh experience in promoting clinic safety and embracing video visits.Ophthalmol Ther. 2020;9:1-9.
- Woodward MA, Ple-Plakon P, Blachley T, et al. Eye care providers' attitudes towards tele-ophthalmology.Telemed J E Health. 2015;21:271-3.
- Jayadev C, Mahendradas P, Vinekar A, et al. Tele-consultations in the wake of COVID-19-Suggested guidelines for clinical ophthalmology.Indian J Ophthalmol. 2020;68:1316-27.
- Sakamoto M, Kanamori A, Fujihara M, et al. Assessment of IcareONE rebound tonometer for self-measuring intraocular pressure.Acta Ophthalmol. 2014;92:243-8.
- Rogers TW, Jaccard N, Carbonaro F, et al. Evaluation of an AI system for the automated detection of glaucoma from stereoscopic optic disc photographs: The European Optic Disc Assessment Study.Eye (Lond). 2019;33:1791-7.
- Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): A multicentre randomised controlled trial.Lancet. 2019;393:1505-16.
- Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome.Eye (Lond). 2017;31:771-5.
- Jayaram H, Strouthidis NG, Gazzard G. The COVID-19 pandemic will redefine the future delivery of glaucoma care.Eye (Lond). 2020;34:1203-05.
- Babu N, Kohli P, Mishra C, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute.Indian J Ophthalmol. 2020;68:1540-4.
- Ting DSJ, Deshmukh R, Said DG, et al. The impact of COVID-19 pandemic on ophthalmology services: Are we ready for the aftermath?Ther Adv Ophthalmol. 2020;12:2515841420964099.
- National Glaucoma Research Foundation Survey Reveals Glaucoma Patients’ Experiences and Concerns During COVID-19 Pandemic. Glaucoma Research Foundation.
- Minocha A, Sim SY, Than J, et al. Survey of ophthalmology practitioners in A&E on current COVID-19 guidance at three Major UK Eye Hospitals.Eye (Lond). 2020;34:1243-5.