Research Article - Journal of Clinical Ophthalmology (2021) New Insights in Ophthalmology
Effects of Covid-19 on walk-in and after hours ophthalmology presentations at a tertiary academic eye center
Sam Whittier1,2, Michael Murri1, Brian Stagg1, Amy Lin1*
1Department of Ophthalmology, Moran Eye Center, University of Utah, Salt Lake City, Utah, USA
2Department of Ophthalmology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, USA
- Corresponding Author:
- Dr. Amy Lin
Department of Ophthalmology
Moran Eye Center
University of Utah
Salt Lake City
Utah, USA
E-mail: amy.lin@hsc.utah.edu
Accepted date: 16 February, 2021
Citation:Whittier S, Murri M, Stagg B, et al.. Effects of Covid-19 on walk-in and after hours ophthalmology presentations at a tertiary academic eye center. J Clin Ophthalmol 2021;5(S2):343-346.
Abstract
Purpose: The novel coronavirus 2019 (Covid-19) has resulted in millions of acute infections and widespread lockdowns. Non-emergent medical care and elective surgical procedures experienced a sharp downturn as a result. The primary aim of this study was to determine the effect of the pandemic lockdown on the volume of ophthalmologic visits at a tertiary care center.
Methods: Retrospective review of 3647 patient encounters was conducted for periods February 15thJuly 31st during the years 2018, 2019, and 2020. Three sub-cohorts of data were analyzed: emergency room consultations, after-hours on-call visits, and daytime visits at a walk-in triage clinic. Encounters were subdivided into pre-lockdown, lockdown, and post-lockdown time periods. Group comparisons were performed with Poisson probability testing.
Results: A total of 1322, 1349, and 976 ophthalmology visits were recorded from February 15th to July 31st for years 2018, 2019, and 2020, respectively. Total visits in 2020 were reduced by 27% when compared to the mean visits for 2018 and 2019, most notably in April (41%), March (34%), May (32%), and June (86%) [p<0.001]. The reduction in 2020 after-hours visits (96%, p<0.001) was significantly greater than that of emergency room consultations (9.4%, p=0.10) and triage center visits (7.7%, p<0.02).
Conclusion: A substantial decrease in ophthalmic care was observed during both the 2020 pandemic lockdown, and while restrictions were eased. After-hours visits were more significantly impacted when compared to other clinical settings. The importance of maintaining ophthalmology walk-in clinics, telemedicine, and increasing patient education are key to optimizing eye health during a global pandemic.
Keywords
Covid-19, Lockdown, Consults, Tertiary academic center, Ophthalmology, Global pandemic, Triage.
Introduction
The novel coronavirus 2019 (Covid-19) originated in Wuhan province, China and began its spread worldwide throughout late 2019 and 2020. To date, over 64 million infections and 1.4 million deaths have occurred worldwide due to the virus [1]. Due to the concern for its asymptomatic spread and high transmission rate, public health officials and governmental entities encouraged and then mandated public health measures such as mask wearing, social distancing, decreases in public activity, and closures of non-essential entities [2-4].
In relation to our institution, in the state of Utah the first known COVID-19 case was placed in quarantine on February 29th [5]. Shortly thereafter the governor declared a state of emergency (March 6th), banned gatherings of 10 or more (March 19th), postponed surgeries (March 23rd), and enacted a stay at home order (March 27th) [6-8]. Later, governmentally mandated restrictions were eased on May 1st and again throughout June and July [4,9,10].
With the subsequent decrease in public mobility and caution surrounding the virus, ophthalmology practices have been impacted around the world. Studies have shown a general decrease in patient visits to emergency departments and in patients seeking ophthalmic care during lockdown periods [11-15]. However, it is unclear whether patients are deferring emergent care in one setting in order to seek care during office hours in another setting. In addition, after a lockdown period, the impact of easing restrictions on patients seeking care is not well documented.
This study is a retrospective review of ophthalmology encounters in three unique settings in our institution: University of Utah emergency room consultations, after-hours visits to the Moran Eye Center, and daytime visits to the Moran Walk-In Triage Clinic. We analyzed these visits in the time period of February 15th through July 31st 2020, both before, during, and after the lockdown period in our area. It is the first study of its kind to examine visits before, during, and after a pandemic lockdown period in multiple care settings.
Materials and Methods
This was a retrospective, cross-sectional study of 3647 patient encounters during the periods of February 15th-July 31st in the years 2018, 2019, and 2020. Institutional review board approval was secured and data was obtained from the University of Utah Data Warehouse. Data was divided into three groups of encounters: University of Utah Emergency Room consultations, after-hours on-call visits to the Moran Eye Center, and daytime visits to the Moran Eye Center Walk- In Triage Clinic. Encounters were grouped in 15 day periods and then month-long periods corresponding to pre-lockdown, lockdown, and post-lockdown time periods. Data was compiled in Excel (Microsoft Office) and group comparisons were performed with Poisson probability testing. Graphs were generated using Microsoft Office Suite.
Results
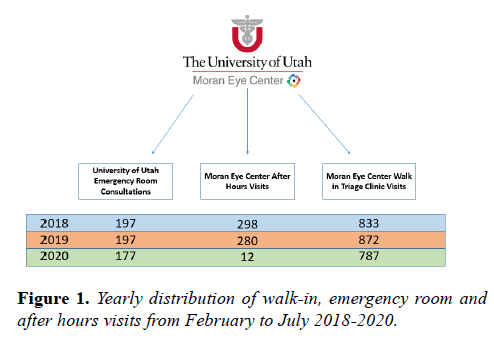
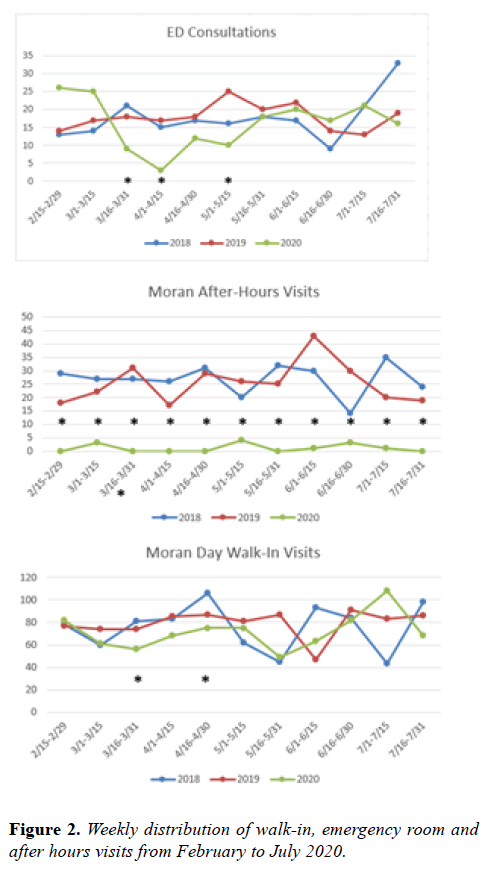
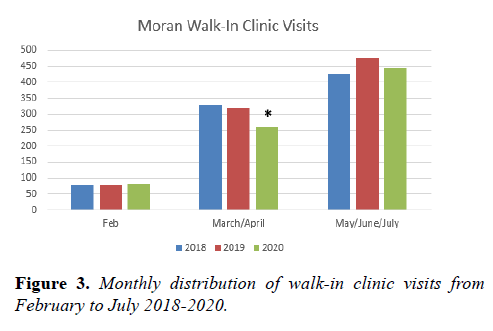
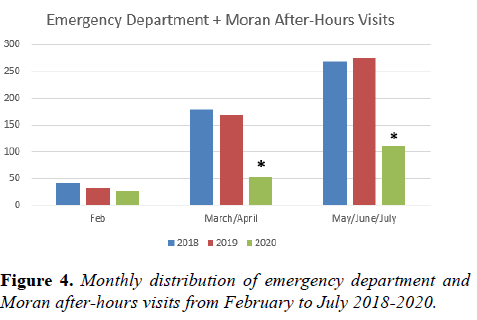
In total, there were 1322, 1349, and 976 ophthalmology visits from February 15th to July 31st in the years 2018, 2019, and 2020 respectively. There was a reduction in total visits in 2020 compared to the 2018 and 2019 mean by 27% overall, which was most stark in the months of April (41%), March (34%), May (32%), and June (86%) [p<0.001]. The differences in total visits in the two week February period and July month from 2020 compared to the 2018 and 2019 visit mean were not significant. There was a stark reduction in 2020 Moran Eye Center after-hours visits compared to 2018 and 2019 during the studied time period (Figure 1). This reduction was significantly greater than the reduction in emergency room consultations and triage center visits (96% reduction, p<0.001 vs. 9.4%, p=0.10 and 7.7%, p<0.02 reduction). In each 15-day time block, the after-hours visits were significantly reduced; emergency room consultations and Walk-In Triage Clinic visits were reduced during some lockdown period time blocks (Figure 2). Walk-In Triage Clinic visits were significantly reduced when compared from 2020 to 2018/2019 average during the March/April time period, but not during the February or May/June/July period (Figure 3). Combined emergency room and after-hours visits were significantly reduced during both the March/April lockdown period as well as the May/June/July easing period.
Discussion
During a global pandemic, the changes in seeking medical care have affected ophthalmology clinic visits, surgical cases, and emergency visits. Our data shows a generalized decrease in visits not only during the lockdown period, but also during the months afterwards when restrictions were eased. The cohort that was most affected was the Moran after-hours visits. These are usually populated with patients that call in after normal business hours, speak with a resident-trainee on call and are directed to present to the Moran Eye Center. The decrease in visits was likely influenced by the routing of patients who might be at risk for COVID-19 with ocular symptoms of conjunctivitis, potential recent travel and/or exposures, or systemic symptoms to the emergency room where they could receive testing and proper isolation, instead of presenting directly to the Moran Eye Center. However, the combination of emergency room visits and after-hours visits in 2020 were significantly lower than the 2019/2018 numbers and thus were not merely shunted from the Moran after-hours visits to the emergency room or to the Walk-In Triage Clinic the next day. The fact that this was the case both during the lockdown period and during the easing period signifies that there was likely a group in the population that was not presenting for emergent eye care that would have done so usually. It is likely that both governmental mandates during a lockdown period as well as generalized concern about COVID-19 even during an easing period had an effect on frequency of patient presentations (Figure 4).
The Moran Walk-In Triage Clinic did have a reduction in visits during the lockdown period that was significant, however during the easing period; the visits were consistent with past years’ volume. This may suggest that patients and/or providers are more comfortable with patients presenting to a daytime walk-in clinic during the Covid-19 era, than to an emergency room setting or even an after-hours setting.
In late 2020, Covid-19 counts have increased as a result of indoor gatherings and holiday-based social events [16-18]. Future case counts are difficult to predict as emerging vaccines, varying levels of public compliance with recommended social distancing measures, appearance of mutated Covid-19 variants and different governmental responses contribute to varying case counts and practice climates in each area. For example, in late 2020, California reinstituted strict stay-at-home mandates due to increasing ICU bed occupancy 18. In lockdown periods, ophthalmology departments, especially in the academic setting, should make efforts to be available to patients who may not feel comfortable seeking emergent care. In one lockdown-era study, academic ophthalmology practices were found to be less available to patients needing appointments [15,19]. In such situations, ophthalmology departments may need to employ strategies such as creating open care ophthalmology walk-in clinics, utilizing triage screening tools, and expanding telemedicine efforts in order to reach patients that may not present otherwise [20-24]. Departments should be mindful of vulnerable populations such as immunocompromised and the elderly and ensure that they are following up appropriately and safely. It is also important to encourage the public to continue to seek eye care when needed and develop creative screening tools.
Conclusion
In 2020, patients seeking ophthalmology care at our institution decreased substantially especially in after-hours visits. As the Covid-19 pandemic has remained a concern, similar patterns may continue. It is important to continue to develop ophthalmology open care walk-in clinics, telemedicine, and educate the public on proper follow up. Academic centers can lead the way in these changes in order to provide for patients in the community.
Declaration of Conflicts of Interest
None of the authors has any competing interests, financial or otherwise.
References
- World Health Organization. WHO coronavirus disease (COVID-19) dashboard, 2020.
- KSL News. Things have changed: Government leaders, schools limit public gatherings to slow virus spread, 2020.
- Recommendations Issued By Task Force to Limit Spread of COVID-19. Coronavirus.utah.gov, 2020.
- National Governors Association. Coronavirus state actions, 2020.
- St. George Man With New Virus Moves to Utah Hospital. U.S. News & World Report. Associated Press, 2020
- Harkins P, Jacobs B, Alberty E. Utah announces its first coronavirus case. And the governor declared a state of emergency. The Salt Lake Tribune, 2020.
- Pierce SD, Canham M, Tanner C, et al. Live coronavirus updates for Thursday, March 19: Utah's confirms 78 cases. The Salt Lake Tribune, 2020.
- Stevens T, Paighten H. Utah governor asks, Salt Lake City mayor orders residents to stay home to slow the spread of the coronavirus. The Salt Lake Tribune, 2020.
- Jacobs B, Means SP. Utah will begin easing coronavirus restrictions Friday, Gov. Gary Herbert says. The Salt Lake Tribune, 2020.
- Means S. Live coronavirus updates for Thursday, May 14: Herbert announces most of Utah will move from 'orange,' to low 'yellow,' risk category, not Salt Lake City. The Salt Lake Tribune, 2020.
- Moon JY, Miller JB, Katz R, et al. The impact of the COVID-19 pandemic on ophthalmic care at an eye-specific emergency department in an outbreak hotspot. Clin Ophthalmol. 2020;14:4155-63.
- Agarwal R, Sharma N, Patil A, et al. Impact of COVID-19 pandemic, national lockdown, and unlocking on an apex tertiary care ophthalmic institute. Indian J Ophthalmol. 2020;68:2391-5.
- El Hamichi S, Gold A, Heier J, et al. Impact of the COVID-19 pandemic on essential vitreoretinal care with three epicenters in the United States. Clin Ophthalmol. 2020;14:2593-8.
- Legrottaglie EF, Balia L, Camesasca FI, et al. Management of an ophthalmology department during COVID-19 pandemic in Milan, Italy. Eur J Ophthalmol. 2020;1120672120960334.
- Babu N, Kohli P, Mishra C, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68:1540-4.
- Maragakis LL. Hopkins Medicine – Health, 2020.
- Kaiser Family Foundation. State COVID-19 Data and Policy Actions, 2020.
- Bloom T, Lyster L. California sends emergency alert to SoCal residents to warn public of stay-at-home order. KTLA5, 2020.
- Starr MR, Israilevich R, Zhitnitsky M, et al. Practice patterns and responsiveness to simulated common ocular complaints among US ophthalmology centers during the COVID-19 pandemic. JAMA Ophthalmol. 2020;138:981-8.
- Arntz A, Khaliliyeh D, Cruzat A, et al. Open-care telemedicine in ophthalmology during the COVID-19 pandemic: a pilot study. Arch Soc Esp Oftalmol. 2020;95:586-90.
- Kapoor S, Eldib A, Hiasat J, et al. Developing a pediatric ophthalmology telemedicine program in the COVID-19 crisis. J AAPOS. 2020;24:204-8.e2.
- Bourdon H, Jaillant R, Ballino A, et al. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: Experience with 500 patients in March and April 2020. J Fr Ophtalmol. 2020;43:577-85.
- Kalra G, Williams AM, Commiskey PW, et al. Incorporating video visits into ophthalmology practice: a retrospective analysis and patient survey to assess initial experiences and patient acceptability at an academic eye center. Ophthalmol Ther. 2020;9:549-62.
- Bommakanti NK, Zhou Y, Ehrlich JR, et al. Application of the sight outcomes research collaborative ophthalmology data repository for triaging patients with glaucoma and clinic appointments during pandemics such as COVID-19. JAMA Ophthalmol. 2020;138:974-80.