Research Article - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 2
Dried bone allograft and orbital fracture reconstruction
Nguyen Thi Phuong1, Le Trong Cuong1, Tran Hong Nhung1*, Ha Thi Thu Ha2, Mai Quoc Tung1, Peter McCluskey3, Pham Trong Van1,21Hanoi Medical University, Hanoi, Vietnam
2Vietnam National Institute of Ophthalmology, Hanoi, Vietnam
3The University of Sydney, Sydney, Australia
- Corresponding Author:
- Dr. Tran Hong Nhung
Hanoi Medical University
Hanoi
Vietnam
E-mail: tranhongnhung0203@yahoo.com.vn
Accepted date: May 27, 2020
Citation: Phuong NT, Cuong LT, Nhung TH, et al. Dried bone allograft and orbital fracture reconstruction. J Clin Ophthalmol 2020;4(2): 239-242.
Abstract
Orbital fracture is a common eye injury related to increasing incidence of accidents. Indications for surgical intervention include: enophthalmos, diplopia and compromised cosmetic appearance. Orbital reconstruction procedure requires bone defect exposure and typically repairs with an implant such as: silicone sheet, Medpore, Titan mesh, bony allograft and other biomaterials. Dried bone grafts can be safe in terms of sterility, immunity and stability. In this report, we review 17 cases of orbital fractures repaired with dried bone implants. Postoperative outcomes were good with increased orbital volume and reduced diplopia. CT scans confirmed long term implant integration into recipients’ orbit. Dried bone graft allografts should be considered as a safe and inexpensive effective material for orbital fracture reconstruction.
Keywords
Orbital fracture reconstruction, Dried bone allograft
Introduction
Orbital fracture is a common orbital injury that requires specific management as it can be a threat to vision, cause of diplopia and compromised cosmetic appearance. Orbital fractures are widely referred to as “blow-out” fractures [1-4]. However, they do not always involve only floor fractures and may be combined with other fractures such as: medial wall, zygomatico-maxillary complex (ZMC) and Le Fort facial fractures [5]. Muscular and intermuscular membrane tissue are trapped into fracture site, causing traction and even limitation to eye movement with consequent diplopia or double vision. Orbital enlargement leads to sunken eye (enophthalmos) and/or downward displaced eye (hypoglobus).
Surgery is usually indicated for orbital fractures resulting in significant enophthalmos and diplopia that fails to resolve and significant trapping of orbital structures within the fracture. Management for such fractures is individualized and depends upon surgical issues such as: timing, approach and requirement for implants [5].
Implants material selection is based on the size and location of bone defects, molding ability of implants to fill complex defects and implant incorporation into tissue [6]. The different implant materials in use can be grouped into autologous tissue (bone, cartilage) and alloplastic materials (Titanium mesh, porous polyethylene, resorbable sheeting) [5]. Autologous bone has often been preferred for orbital fracture reconstruction because of its strength and radiopacity. Its popularity has waned due to lacked pliability and donor site morbidity [6]. This case series reports the outcomes of orbital reconstruction using dried bone allografts.
Materials and Methods
A prospective study of patients undergoing surgical repair for orbital fractures including: large orbital floor defects, combined wall fractures and ZMC fractures was undertaken at Hanoi Medical University and Vietnam National Institute of Ophthalmology.
Femur bone was processed based on “Standards for Tissue Banking. American Association of Tissue Banks (AATB) (2016)” [7]. The donors were under the age of 60 and free from HIV, hepatitis and syphilis. The collected bone was washed with hydroxyperoxite then soaked in solution of antibiotics (benzylpenicillin 1,000,000 IU and streptomycin sulfate 1 g) for 30 minutes. The sterilized bone was cut into slices with 3 mm thickness, dried in vacuum at -56°C for 72 hours and resterilized using gamma ray at 25 Gy (Figure 1).
Orbital and/or maxillofacial fractures were repaired in a sequence under general anesthesia. First, forced duction test was performed to assess ocular motility. The orbital rim was exposed by lateral canthotomy or “swinging eyelid” procedure. Dissection continued in the subperiosteal plane into the orbit to expose orbital fracture defects. Herniated tissue was retracted from the sinus mucosa back to the orbit or freed to improve ocular motility. Then, the bone implant was sized and shaped to cover the fracture rim. Tisseel fibrin glue was used to immobilize the implant. Forced duction test was performed again to assure tissue release before closing the wound.
No nose blowing was recommended to avoid implant mobilization for at least 2 weeks after surgery. Patients were treated postoperatively with Unasyn 375 mg – a combination of Ampicillin and Sulbactam 2 times a day for 3 days. Patients were observed for diplopia and enophthalmos at 1 week, 1 month and 3 month period. Enophthalmos and diplopia were assessed using Hertel exophthalmometer and binocular visual field (BVF) respectively [8].
Results
Out of 17 patients including 15 males and 2 females aged from 13 to 62, 11 patients (64.7%) complained of diplopia, 2 (11.8%) were concerned about enophthalmos and 4 (23.5%) worried about cosmetic appearance. 14 cases were admitted 1 month after injury, and only 3 patients came to the hospital less than 2 weeks after injury. Notably, 2 patients had undergone previous orbital floor reconstruction. Visual acuity was functionally good from 20/50 to 20/20 with correction.
Single wall fractures accounted for 35.3% and combined ones made up 64.7% (Table 1).
| Fracture type | No of eyes | % |
|---|---|---|
| Floor | 6 | 35.29 |
| Floor+Medial wall | 3 | 17.65 |
| Floor+ZMC | 3 | 17.65 |
| Floor+Upper wall | 2 | 11.76 |
| Multiple walls | 3 | 17.65 |
Table 1. Distribution by fracture type.
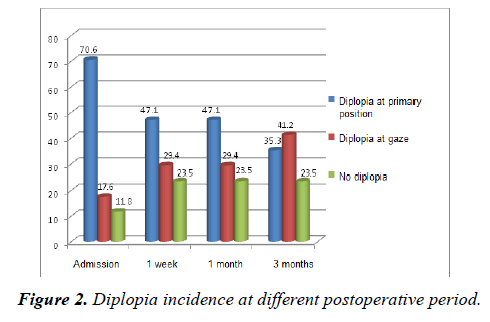
Preoperatively 70.6% of the patients had diplopia in the primary position and 17.5% in secondary positions of gaze. At final review 3 months postoperatively, 35.3% of the patients had diplopia in the primary position and 41.2% in secondary positions of gaze, 23.5% had no diplopia. Figure 2 presents details of diplopia at primary position and gaze.
Data showed significant reduction of postoperative diplopia at primary position. However, at gaze, the rate of diplopia was still high. This result may be due to late presentation with preoperative fibrosis which was underestimated during surgery. Complex muscle and orbital injury may be taken as undetermined factors leading to unpredictable outcomes.
Enophthalmos progression had also been assessed at different periods, which showed a significant reduction at one week period. However, with time, this sign increased with lower degree than at preoperative period (Table 2). Postoperative complications included entropion (1 case) and mild ectropion (1 case) that were repaired using retractor advancement procedure (Figure 2).
| Time | N (eyes) | Enophthalmos degree (mm) | p |
|---|---|---|---|
| At admission | 17 | 1.28 ± 1.40 | p=0.007 |
| 1 week | 17 | 0.35 ± 0.70 | p=0.004 |
| 1 month | 17 | 0.47 ± 0.80 | p=0.02 |
| 3 month | 17 | 0.76 ± 1.10 | p=0.03 |
Table 2. Enophthalmos evaluation at post-operative periods.
Discussion
Orbital bone fracture involves a single or complex combination of multiple walls. Surgery is the main indication with unpredictable postoperative outcomes. In the literature, several classifications of orbital wall fracture have been described [9-11]. However, this study used the one of Jaquiery et al. because it implies the large size of bone defect and the ledge for graft support [7].
In this study, surgical approach was important because it provided convenient access to defects locating in orbital floor and/or medial wall. “ Swing eyelid ” was performed with canthotomy and inferior socket incision which allowed the approach to both inferior and medial wall fracture site and to insert the graft material.
Reconstruction of orbital fractures requires the selection of a wide variety of implants which can be grouped into autogenous/autologous materials (bone and cartilage) and alloplastic materials (Titanium mesh, resorbable sheeting, and porous polyethylene) [12-18]. The consideration for choice depends on the assessment of patient’s age, size and location of fractures, cost and availability of materials. Alloplastic implants are biocompatible, easily trimmed into any desired shape and can be fixated to bone [16,17]. Recently, resorbable sheeting is pliable and can be contoured to the orbital defect [19,20]. However, this is not affordable in a developing country. The use of dried bone can meet the requirements of shortening surgical time, biocompatibility and expense. The implant can be selected based on the thickness needed to improve enophthalmos in patients with significant orbital volume insufficiency. The lack of pliability and difficult molding can be the disadvantages. Studies on iliac bone grafts have shown bone resorption [13-16]. This study demonstrates that the technique is reliable in improving enophthalmos and hypoblobus. In children with “green stick” fractures, thick dried bone graft may not be a good selection [21].
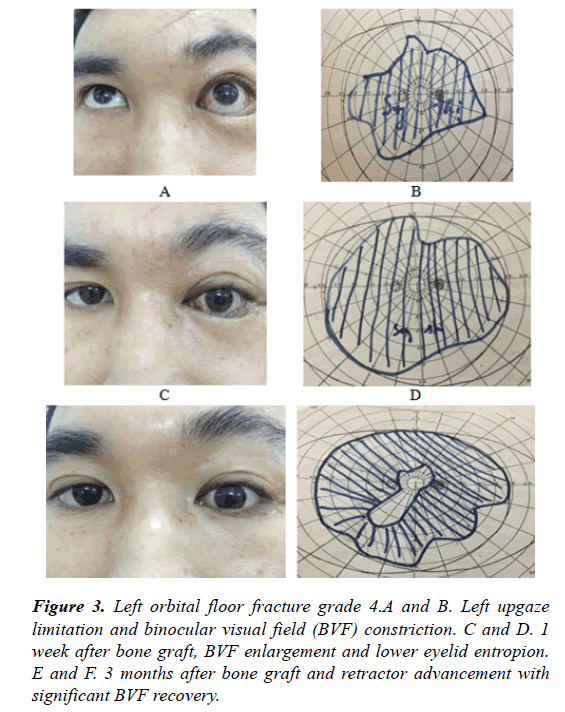
Diplopia assessment is performed using BVF [8]. This technique provides a quick assessment allowing a sufficient visual comparison of field area before and after surgery (Figure 3).
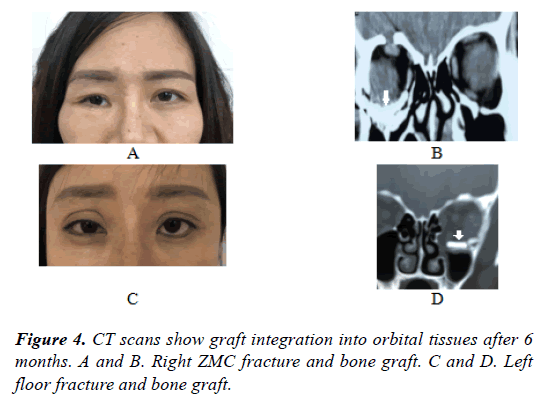
This study evaluated the stability and integration of bone graft using CT scan at 3 month time after surgery (Figure 4). The use of fibrin glue and graft with sufficient size was effective to assure graft stability.
Conclusion
The study leads to a conclusion that the use of dried bone graft is acceptable for the repair of the orbital floor defects with good clinical long-term results.
Financial Interest
None financial disclosures.
Conflicts of Interest
Conflicts of interest none with any of the authors.
References
- Cruz AA, Eichenberger GC. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol. 2004;15:416-21.
- Hwang K, You SH, Sohn IA. Analysis of orbital bone fractures: A 12-year study of 391 patients. J Craniofacial Surg. 2009;20:1218-23.
- Shere JL, Boole JR, Holtel MR, et al. An analysis of 3599 midfacial and 1141 orbital blowout fractures among 4426 United States Army Soldiers, 1980-2000. Otolaryngol Head Neck Surg. 2004;130:164-70.
- Erdmann D, Follmar KE, Debruijn M, et al. A retrospective analysis of facial fracture etiologies. Annals of plastic surgery. 2008;60:398-403.
- Boyette JR, Pemberton JD, Bonilla-Velez J. Management of orbital fractures: challenges and solutions. Clin Ophthalmol. 2015;9:2127-37.
- Mok D, Lessard L, Cordoba C, et al. A review of materials currently used in orbital floor reconstruction. Can J Plast Surg. 2004;12:134-40.
- Standards for Tissue Banking. American Association of Tissue Banks (AATB) 2016.
- Harris GJ, Garcia GH, Logani SC, et al. Correlation of preoperative computed tomography and postoperative ocular motility in orbital blowout fractures. Ophthalmic Plast Reconstr Surg. 2000;16:179-87.
- Carinci F, Zollino I, Brunelli G, et al. Orbital fractures: a new classification and staging of 190 patients. Orbital fractures: a new classification and staging of 190 patients. J Craniofac Surg. 2006;17:1040-4.
- Manolidis S, Weeks BH, Kirby M, et al. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. The J Craniofac Surg. 2002;13:726-37.
- Kunz C, Audige L, Cornelius CP, et al. The Comprehensive AOCMF Classification System: Orbital Fractures - Level 3 Tutorial. Craniomaxillofac Trauma Reconst. 2014;7:S092-102.
- Strong EB. Orbital fractures: pathophysiology and implant materials for orbital reconstruction. Facial Plast Surg. 2014;30:509-17.
- Gunarajah DR, Samman N. Biomaterials for repair of orbital floor blowout fractures: A systematic review. J Oral Maxillofac Surg. 2013;71:550-70.
- Zunz E, Blanc O, Leibovitch I. Traumatic orbital floor fractures: repair with autogenous bone grafts in a tertiary trauma center. J Oral Maxillofac Surg. 2012;70:584-92.
- Ellis E, 3rd, Tan Y. Assessment of internal orbital reconstructions for pure blowout fractures: cranial bone grafts versus titanium mesh. J J Oral Maxillofac Surg. 2003;61:442-53.
- Guo L, Tian W, Feng F, et al. Reconstruction of orbital floor fractures: comparison of individual prefabricated titanium implants and calvarial bone grafts. Annals of plastic surgery. 2009;63:624-31.
- Kontio RK, Laine P, Salo A, et al. Reconstruction of internal orbital wall fracture with iliac crest free bone graft: clinical, computed tomography, and magnetic resonance imaging follow-up study. PlastReconstr Surg. 2006;118:1365-74.
- Bayat M, Momen-Heravi F, Khalilzadeh O, et al. Comparison of conchal cartilage graft with nasal septal cartilage graft for reconstruction of orbital floor blowout fractures. Br J Oral Maxillofac Surg. 2010;48:617-20.
- Yilmaz M, Vayvada H, Aydin E, et al. Repair of fractures of the orbital floor with porous polyethylene implants. Br J Oral Maxillofac Surg. 2007;45:640-4.
- Steinmassl O, Laimer J, Offermanns V, et al. Clinical outcome following surgical repair of small versus large orbital floor fractures using polyglactin 910/polydioxanone (Ethisorb((R))). Materials (Basel). 2020;13:206.
- Oppenheimer AJ, Monson LA, Buchman SR. Pediatric orbital fractures. Craniomaxillofac Trauma Reconstr. 2013;6:9-20.