Research Article - Journal of Intensive and Critical Care Nursing (2022) Volume 5, Issue 4
Does the duration of subcutaneous low-molecular-weight heparin injection impact in the occurrence, extent of bruising and on site pain?
Rajani Shireen*, Batool Afeera, Domanog Marlene Tan, Manlapig Michelle, Rajpali Saima, Shaheen UzmaKing Faisal Specialist Hospital & Research Center, Riyadh, Kingdom of Saudi Arabia
- *Corresponding Author:
- Rajani Shireen
King Faisal Specialist Hospital & Research Center
Riyadh, Kingdom of Saudi Arabia
E-mail: shireen.rajani@gmail.com
Received: 23-Jul-2022, Manuscript No. AAICCN-22-70133; Editor assigned: 25-Jul-2022, PreQC No. AAICCN-22-70133 (PQ); Reviewed: 02-Aug-2022, QC No AAICCN-22-70133; Revised: 09-Aug-2022, Manuscript No. AAICCN-22-70133(R); Published: 13-Aug-2022, DOI:10.35841/aaiccn-5.4.116
Citation: Shireen R. Does the duration of subcutaneous low-molecular-weight heparin injection impact in the occurrence, extent of bruising and on site pain?. J Intensive Crit Care Nurs. 2022;5(4):116
Abstract
Background: Subcutaneous injections often cause pain and bruising. It is noteworthy that the pain of the site causes the patient to experience physical and mental discomfort. A few ways to prevent bruise and pain under heparin injection have been extensively researched but duration of the pain and the extent of bruising is little documented.
Aim: The purpose of this study was to evaluate the duration of injecting heparin with a low molecular weight of 10 seconds compared to 20 seconds regarding the occurrence and level of bruise and pain at the Research Hospital in Kingdom of Saudi Arabia.
Method: Quasi Experimental design was used for successive patient admission to the Cardiovascular Division under services of post cardiovascular surgery, medical cardiology and vascular cases in King Faisal Specialist Hospital & Research Centre, Riyadh, KSA. The adjusted variable was the injection time of 10 seconds (treatment A) compared to 20 seconds (treatment B). Patients were followed up at 48 and 60 hours to evaluate the degree of bruising. Expert and trained nurses performed the Enoxaparin administration to the patient. The data analysis was performed in a blind fashion.
Result: Out of 194 patients, 6.2% (n=12) patients had bruises of 10-150 mm at 48 hours and 6.7% (n=13) patients had bruises of 20-150 mm at 60 hours with injection technique of 10 seconds. During the injection duration of 20 seconds, 3.1% (n=6) patients had bruises of 10-100 mm at 48 hours which was further observed until 60 hours. Out of 194 patients, 70.6% (n=137) patients had site pain (score of 1-6) with injection technique of 10 seconds and 37.6% (n=73) patients had site pain (score of 1-5) with injection technique of 20 seconds. Research finding showing that assessment of bruise at 60 hours with injection duration of 10 seconds is more than the injection duration of 20 seconds. Analysis of pain assessment reveals that majority of patient had increase in intensity of pain in 10 seconds and no significant changes found in the pain score from initial 10 seconds versus 20 seconds.
Conclusion: Our research study provides new knowledge regarding injecting subcutaneous low molecular weight heparin that in 20 seconds injection, it lowers the occurrence of bruise in comparison to 10 seconds injection with no subsequent difference in the pain level.
Keywords
Intensive Care, ICU, Administration, Bruise, Case-crossover, Duration, Injection, Low-molecular-weight heparin, Quasi-experimental.
Introduction
Deep Vein Thrombosis is a leading cause of preventable death in the United States. The possibility of developing a Deep Vein Thrombosis is one major complication for the patient population with damaged blood vessels, decreased circulation problems or restricted mobility. Deep Vein Thrombosis can eventually lead to strokes, myocardial infarctions or pulmonary embolisms, these are often preventable complications that not only harm the patient but increase the resources needed to treat and rehabilitate the individual [1].
For years, the common method for prevention of a Venous Thromboembolism, or treatment of a Deep Vein Thrombosis, has been unfractionated heparin [2]. Heparin does not dissolve a clot; it only facilitates the body’s own mechanism to dissolve the clot [3]. Heparin’s anticoagulant effect is achieved by combining with antithrombin III, which is already present in the body [3,4]. The result is a state of increased anticoagulation.
Subcutaneous injections often cause pain and bruising [5-7]. When nurses give injections as part of the medical care, it can cause patients to become apprehensive about receiving future subcutaneous medications, anxious about the nursing staff, or even noncompliant with medical care [5]. Noted that site-pain causes the patient physical and psychological discomfort and bruising limits possible sites for subsequent injections [5].
The safe and accurate administration of medication is one of the most important responsibilities of nurses [8,9]. Although subcutaneous heparin administration is a frequently performed nursing intervention, it often causes problems such as bruise, hematoma, induration and pain at the injection site [10]. Bruise occurs when a force causes blood vessels to blast. Blood leaks into areas under the skin resulting in pain, swelling, and skin discoloration. A bruise is an area of skin discoloration that is ≥ 2 mm2 [5,11]. Subcutaneous injection of LMWH in the abdominal area could reduce the incidence of side-effects at the injection site and reduce patient discomfort [12].
Literature Review
According to the study of Reva Balci Akpinara et al. [13], after 20 second duration while administration of enoxaparin left with fewer and smaller bruises as compare to 10 second duration. This study provides new information for nursing practice about bruising associated with subcutaneous heparin.
According to Harriet Chan et al. [5], the bruise incidence at the 10 seconds injection technique sites was approximately double that of the 20-seconds injection technique sites, clearly indicating that slow administration of subcutaneous heparin injections had lesser impact on bruising. According to the randomized controlled trial of 44 patients at Division of Perioperative Nursing, Department of Nursing, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, a 30-seconds duration injection with a 10-seconds pause before needle withdrawal resulted in significantly fewer and smaller bruises [14].
In the literature, slow administration of subcutaneous heparin injection is recommended [15-17]. It is stated that when an injection is administered slowly, tissue damage can be reduced due to the reduction of giving strength of drug to the tissue [10,18,19].
According to the finding of the research study of Ayten Zaybak et al. [20], the use of a 20 seconds duration for administering heparin injections reduces the incidence or size of bruising. 20 seconds duration injection technique should be used for subcutaneous heparin injections in clinical practice. This study allocated patients from several specialties, where 50% of the patients were taken from the cardiology unit, 36% from the orthopedics unit and 14% from the neurology unit. The sample for the study consisted of 50 patients to whom subcutaneous heparin was administered All subjects were alert and conscious enough to answer questions. The percentage of bruising occurrence was 64% with the control injection technique and 42% with the experimental injection technique.
According to Tayebe Pourghaznein, Amir Vahedian Amir Vahedian Azimi et al. [21], the quasiexperimental study was conducted on 90 patients with Chronic Obstructive Pulmonary Disease hospitalized in two Intensive Care Unit wards at two teaching hospitals in Iran. They were injected heparin subcutaneously, being given a dosage of 4000 units every 12 hours. In the method; 15 seconds injection duration and waiting for 5 seconds before withdrawing the needle, the number of bruising was significantly lower and size of bruising was significantly smaller. The method 15 seconds injection duration and waiting for 5 seconds before withdrawing the needle is recommended to be used for subcutaneous heparin injection by clinical nurses. As to the results, the severity of pain in abdomen was lower than in thighs.
According to Dilek Yılmaz, et al. a quasi-experimental study was conducted with 60 patients at Department of Nursing, Bursa Uludağ University Faculty of Health Sciences, Bursa, Turkey. The patients were injected the Low Molecular Weight Heparin (LMWH) injection and pressure was applied with dry cotton for 10 seconds vs. 60-seconds directly after the needle was withdrawn. After the injection process was completed, the dimension of the bruising formed was evaluated. It was concluded that the duration of pressure applied to the injection site after subcutaneous LMWH injection did not affect the size of bruising or the severity of pain. 10-seconds of pressure applied to the injection site after subcutaneous LMWH injection may be enough to reduce complications [22].
According to Harriet Chan et al. [5], subcutaneous heparin over a longer duration may reduce injection site-pain and bruising. A convenience sample of 34 subject receiving 5000 units of a subcutaneous Fragmin injection twice a day were recruited from a large teaching hospital. Subjects rated the level of perceived site-pain intensity during injection using the vertical Visual Analogue Scale. Injection-site bruising was measured at 48 and 60 hours after injection. Results indicated that 20-seconds injection duration resulted in significantly less intense site-pain during administering the injection and fewer and smaller bruises.
During the research and studies made over the years on about more than 500 patients, five RCTs were identified that evaluated the effect of subcutaneous heparin injection duration on pain intensity, bruise size and incidence. It was found that pain may be slightly reduced 48 hours after slow injection. Similarly, there may be a reduction in bruise size and incidence after slow injection compared to fast injection, 48 and 60 hours post injection [23, 24].
Considering the investigative findings within the limitations, the following conclusions can be drawn. The 20-seconds duration injection significantly reduces site-pain during injection and results in fewer and smaller bruises. This technique, therefore, is worth considering in developing nursing practice guidelines [5].
Purpose of the Study
The purpose of this study was to evaluate the duration of injecting heparin with a low molecular weight of 10 seconds compared to 20 seconds regarding the occurrence and level of bruise and pain due to this differences in time; in Research Hospital in Kingdom of Saudi Arabia. Several studies were conducted in the past on the same subject but for patients with different medical conditions (i.e. orthopedic patients and others) and not much of the studies have been done on cardiovascular patients. Moreover, none of those studies were done in Kingdom of Saudi Arabia.
Inclusion Criteria
Patients were selected if (a) they were at least 14 years old, conscious, oriented and alert, (b) were candidates for or had already underwent cardiovascular or vascular surgery, (c) were on bed rest, (d) were about to get subcutaneous Low Molecular Weight Heparin therapy, (e) provided permission to engage in the research.
Exclusion Criteria
Patients were ruled out if they (a) were pediatric patients less than 14 yrs old, (b) were pregnant, (c) had alter integrity of abdominal area, (d) had abnormal coagulation, hematological disease, liver disease and increased International Normalized Ratio, (e) were having other subcutaneous injections at the abdomen, (f) had low platelet count (< 140, 000 /mm3), (g) had dark skin colour.
Limitations
a) Either patient was discharged before the completion of study or medication was discontinued before the completion of two injection cycles (10 and 20 seconds).
b) Pandemic crises of COVID’19.
c) Turnover of task force / Change in research team body.
d) Patient’s refusal to take part in research study.
Research Design
A quasi-experimental method was used. A continuous admission/ transfer to the cardiovascular nursing units (Adult Cardiology Unit, Cardiovascular Telemetry Unit, Coronary Care Unit, Cardiovascular Step Down Unit and Cardiac Surgery Intensive Care Unit) under adult cardiovascular, adult cardiology and vascular service in King Faisal Specialist Hospital & Research Centre, Riyadh, KSA. was eligible for enrolment as these patients receive low molecular subcutaneous heparin.
The exposure/intervention factor was the duration of the administration time of injection, 10 seconds versus 20 seconds. According to the evidence available, bruises usually peaks at 48 hours and starts disappearing within 72 hours of injection. Bruises were evaluated exactly 48 hours and 60 hours after injection; by an expert nurse with specific instructions and were blinded to the duration of injection. He/she evaluated the abdomen at the marked area 1 cm apart with nontoxic waterremovable coloured ink on both sides.
The extent of the bruise was measured with a measure tape. The maximum diameter of the bruise was recorded (in millimetres) regardless of whether the bruise was regular or uneven in shape at the time of measurement. The location of each treatment is known only to the person who injected it.
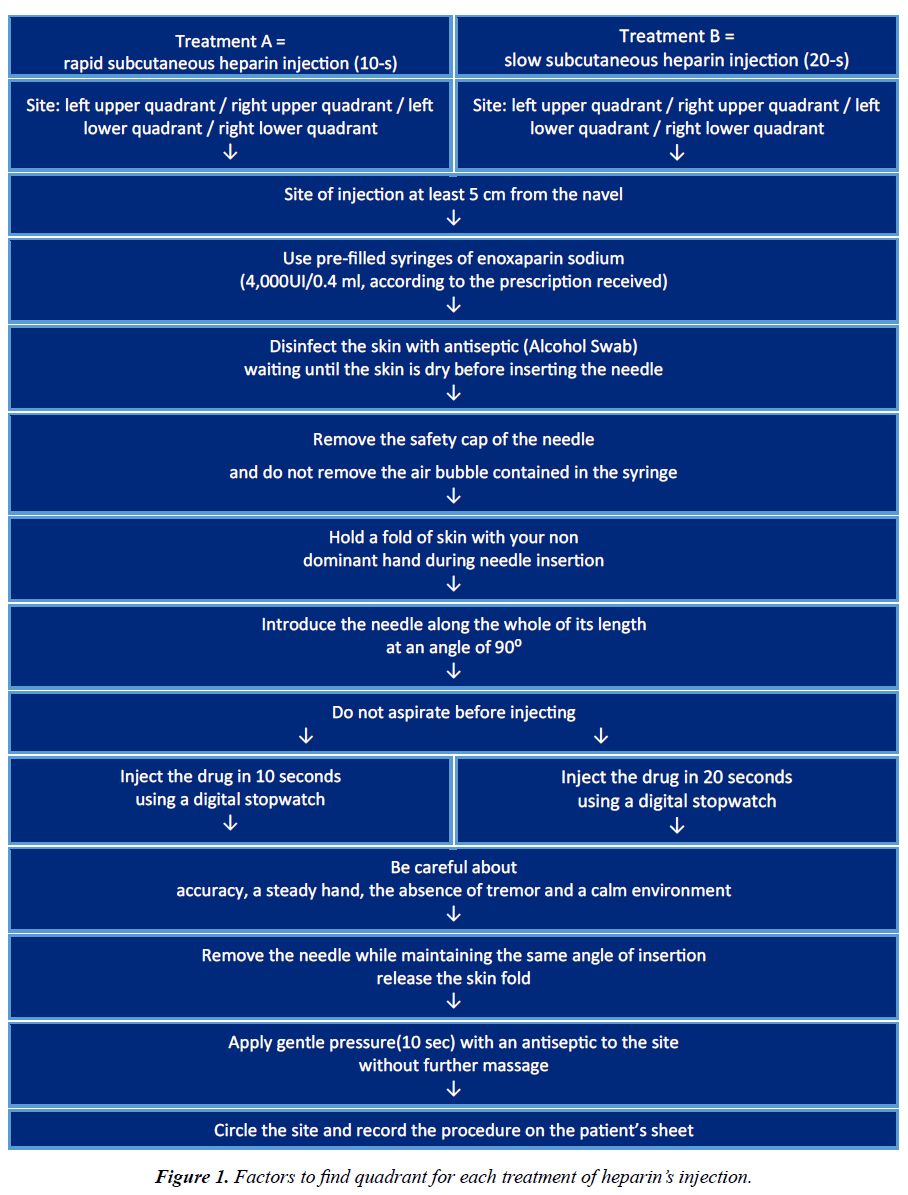
The area decided (upper left quadrant / upper right quadrant / lower left quadrant / lower right quadrant) for each treatment (treatment A; 10 seconds; treatment B; 20 seconds) was locked inside a sealed envelope and placed in a locker. The nurse who examined the bruises had no idea about the treatment performed, either on the left or right side of the abdomen. Data analysis was also performed blindly (Figure 1).
Sample Size
We performed study of 10 seconds and 20 seconds of subcutaneous heparin injection on the same patient. 194 subjects were studied in order to reject the null hypothesis; i.e., this relative risk equals 1 with probability (power) 0.8. The Type I error probability associated with this test of this null hypothesis is 0.05.
Outcomes Measure
a) To measure the occurrence, extent of bruises after two different injection durations.
b) To measure the pain score at the site of injection with two different injection durations.
Blind Procedure
The location of each treatment was known only to the nurse who injected it. The location was written on paper, placed in an envelope and stored in a locked safe. Nurses who examined the bruises did not know which treatments were performed on either location. Data analysis was also performed blindly. An envelope containing this information was opened after the analysis was completed.
Study Variables
Independent Variables collected include age, gender; diagnosis and size of bruising in mm. Investigators were trained to perform the two types of injections. Surgery, past medical history, neurologic status, current medication and admission date were collected. Dependent Variables collected include site of injection, self-reported pain scores using the Adult Verbal Pain Scale at the time of injection and site measurement at 48 hours and 60 hours after administration for occurrence of bruising using the measure tape.
Results
A total of three hundred & eight (308) patients were enrolled during the last 5 years (March 2015 – June 2020) of this research study and 62.98% (n=194) patients received 1st and 2nd subcutaneous Low Molecular Weight Heparin injection (388 injections) and completed the assessment of 48 and 60 hours.
Remaining 37.02% (n=114) patients were excluded due to discontinuation of the medication or discharged before completion of the assessment within 48 and 60 hours.
The study included 194 subjects on whom both 10 seconds and 20 seconds injection (at two distinct points in time) were administered. A total of 85.57% (n=166) subjects had the 10 seconds first followed by the 20 seconds, and the remaining 14.43% (n=28) had the 20 seconds first followed by the 10 seconds.
Occurrence and Extend of Bruise
A total of 183 subjects had similar amounts of bruising for the two injections 179 with no bruising from the 10 seconds and no bruising from the 20 seconds injection, and 4 with bruising from both injections (and of similar sizes). Among the remainder (11), nine had bruising from the 10 seconds injection and no bruising from the 20 seconds and two had bruising from the 20 seconds injection and no bruising from the 10 seconds. This suggests a stronger propensity for bruising following the 10 seconds injection versus the 20 seconds injection. Based on the finding of the research, the p-value of the analysis was found to be 0.0002 using Fisher’s Exact Test (Tables 1 and 2).
| 10 Seconds Injection (Bruise 60 hours) By 20 Seconds Injection (Bruise 60 hours) | |||
| Count | No | Yes | Total |
| Total % | |||
| Col % | |||
| Row % | |||
| No | 179 | 2 | 181 |
| 92.27 | 1.03 | 93.3 | |
| 95.21 | 33.33 | ||
| 98.9 | 1.1 | ||
| Yes | 9 | 4 | 13 |
| 4.64 | 2.06 | 6.7 | |
| 4.79 | 66.67 | ||
| 69.23 | 30.77 | ||
| Total | 188 | 6 | 194 |
| 96.91 | 3.09 | ||
Table 1.Contingency table.
| Fisher's Exact Test | Probability | Alternative Hypothesis |
|---|---|---|
| Left | 1 | Probability (20 Seconds Injection (Bruise 60 hour) = Yes) is greater for 10 Seconds Injection (Bruise 60 hour) = No than Yes |
| Right | 0.0002* | Probability (20 Seconds Injection (Bruise 60 hour) = Yes) is greater for 10 Seconds Injection (Bruise 60 hour) = Yes than No |
| 2-Tail | 0.0002* | Probability (20 Seconds Injection (Bruise 60 hour) = Yes) is different across 10 Seconds Injection (Bruise 60 hour) |
Table 2.The analysis the p-value using Fisher’s Exact Test.
Intensity of Pain
In terms of pain during the injection, 113 subjects were able to discern a differential amount of pain from the two injections 8 subjects reporting more pain from the 20 seconds injection and 105 subjects reporting more from the 10 seconds injection. This did not seem to vary according to the initial pain as illustrated in the table below (Table 2).
Interestingly, when only the initial pain scores were compared between the 166 for whom the initial injection was a 10 seconds with the 28 for whom the initial injection was a 20 seconds, no difference was found in the level of pains (p = 0.2321 using Chi Square Approximation).
Contingency analyses of pain comparison were conducted while adjusting for age, gender, type of diagnosis/surgery, and past medical history. No differential relationships in pain score comparisons were noted across these adjusting variables.
Conclusion
Our research study provides new knowledge regarding injecting subcutaneous low molecular weight heparin that in 20 seconds injection, it reduces the occurrence of bruise compared to 10 seconds injection with no subsequent variation found in the pain level of the patients receiving 10 seconds versus 20 seconds injection.
Ethical Consideration
a) This research was conducted according to the ethical principles contained in the Declaration of Helsinki, the ICH Harmonized Tripartite Good Clinical Practice Guidelines, the policies and guidelines of the RAC at King Faisal Specialist Hospital & Research Centre, Riyadh, KSA and Saudi Arabian law.
b) Each and every participant in this study gave their consent in a written statement.
c) Every subject in the research was assigned a unique identification number different from their Medical Record Number to ensure the anonymity of the patients during data analysis subsequent to its collection. The list of patients’ identification number with its respective Medical Record Number was kept under lock and key. A predefined form was used to collect data that indicated the patients’ serial number only. The database and all digital records relevant to this study were password protected and known to the investigators and research coordinator only.
References
- Chenicek TE, Jeanne F, Sandra F, et al. Effects of injection duration on site-pain intensity and bruising associated with subcutaneous administration of Lovenox (enoxaparin sodium). 2004.
- Thompson‐Ford JK. Low‐Molecular‐Weight Heparin for the Treatment of Deep Vein Thrombosis. Pharmacotherapy. 1998;18(4):748-58.
- Pavlovich-Danis S. Advances in DVT treatment and prophylaxis. Myfreece.com. 2002.
- Hovanessian, H. New-generation anticoagulants: The low molecular weight heparins. Ann Emerg Med. 1999;34(6):768-79.
- Chan H. Effects of injection duration on site-pain intensity and bruising associated with subcutaneous heparin. J Adv Nurs. 2001;35(6):882-92.
- Kuzu N, Ucar H. The effect of cold on the occurrence of bruising, Hematoma and pain at the injection site in subcutaneous low molecular weight heparin. Int J Nurs Stud. 2001;38(1):51-9.
- Venketasubramanian N, Chua H. Subcutaneous low molecular weight heparin in place of heparin infusion during warfarin dose optimization in cerebral ischemia. Clin Neurol Neurosurg. 1998;100(3):193-5.
- Hall LM, Doran D, Pink GH. Nurse staffing models, nursing hours, and patient safety outcomes. J Nurs Adm. 2004;34(1):41-5.
- Hogan MA. Administering and subcutaneous injection. Fundamental of nursing caring and clinical judgment, 1st edn, Philadelphia, Saunders. 2000:567-9.
- Kuzu, N. Subcutaneous heparin injections: How to prevent the occurrence of pain, echymosis and hematoma? Cumhur Medical J. 1999;3(2):40-6.
- McGowan S, Wood A. Administering heparin subcutaneously: An evaluation of techniques used and bruising at the injection site. Aust J Adv Nurs. 1990;7(2):30-9.
- Yun Li, Dong S, Wang P, et al. Influence of low-molecular-weight heparin injection sites on local bruising and pain: A systematic review and meta-analysis. J Clin Pharm Ther. 2021;46(3):688-97.
- Akpinar RB, Celebioglu A. Effect of injection duration on bruising associated with subcutaneous heparin: A quasi-experimental within-subject design. Int J Nurs Stud. 2008;45(6):812-7.
- Jueakaew S, Piancharoensin R, Pinkesorn N, et al. Novel subcutaneous low-molecular-weight heparin injection technique to reduce post-injection bruising. Phlebol. 2019;34(6):399-405.
- Stassi ME, Harkreader H, Hogan MA, et al. Fundamentals of nursing: Caring and clinical judgment. Saunders; 2007.
- Vanbree NS, Hollerbach AD, Brooks GP. Clinical evaluation of three techniques for administering low-dose heparin. Nursing Res. 1983;33(1):15-9.
- Canobbio MM, Paquette EV, Wells MF, et al. Patient care standards: Collaborative practice planning guides. Mosby Year Book, MO. 1996.
- Edwina AM. Do’s & don’ts: Administering subcutaneous heparin. Nursing. 2000;30(6):17-8.
- Potter AP, Perry AG. Fundamental of Nursing. C. V. Mosby Company, Louis 6th edition. 2009.
- Zaybak A, Khorshid L. A study on the effect of the duration of subcutaneous heparin injection on bruising and pain. J Clin Nurs. 2008;17(3):378-85.
- Pourghaznein T, Azimi AV, Jafarabadi MA. The effect of injection duration and injection site on pain and bruising of subcutaneous injection of heparin. J Clin Nurs. 2014;23(7-8):1105-13.
- Yılmaz D, Düzgün F, Durmaz H, et al. The effect of duration of pressure on bruising and pain in the subcutaneous heparin injection site. Jpn J Nurs Sci. 2020;17(3):e12325.
- Mohammady M, Radmehr M, Janani L. Slow versus fast subcutaneous heparin injections for prevention of bruising and site pain intensity. Cochrane Database Syst Rev. 2021.
- Beyea SC, Nicoll LH. Subcutaneous administration of heparin: an integrative review of the research. Worldviews Evid Based Nurs. 1996;3(1):1-5.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref