Research Article - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 3
Correlation between pre and post-operative macular volume and visual acuity following epiretinal membrane surgery
Kasen L Culler BS1, Hong-Gam Le MD1, Mathew W Mac Cumber MD 2, Manjot K Gill MD1*
1Department of Ophthalmology, Northwestern University Feinberg School of Medicine, Michigan, USA
2Department of Ophthalmology, Rush University Medical Center, Chicago, Illinois, USA
- Corresponding Author:
- Dr. Manjot K. Gill
Associate Professor of Ophthalmology
Director of Vitreoretinal Fellowships
Northwestern University Feinberg School of Medicine
Suite 440, 645 N Michigan Avenue
Chicago, Illinois 60611
USA
E-mail: mgill@nm.org
Accepted date: 06 May, 2021
Citation:Culler KL, Le HG, MacCumber MW, et al. Correlation between pre and post-operative macular volume and visual acuity following epiretinal membrane surgery. J Clin Ophthalmol 2021;5(3):409-413.
Abstract
Purpose: To evaluate the correlation between pre and post-operative macular volume and visual acuity (VA) and post-operative visual gain in patients who underwent surgical removal of epiretinal membrane (ERM).
Methods: Retrospective chart review of 62 patients at a single academic eye center was performed. Patients who underwent pars plana vitrectomy and membrane peel for visually significant epiretinal membrane were included. Those with any confounding macular pathology were excluded.
Fellow unaffected eyes were used as controls for macular volume comparison. Clinical and surgical data including pre and post-operative visual acuity, presence of metamorphopsia, lens status, pre and post-operative preoperative macular volume measured by Optical Coherence Tomography (OCT), and surgical procedures were collected and analyzed. The correlation between macular volume and visual acuity as well as post-operative visual gain was calculated.
Results: There was no statistically significant correlation between macular volume and baseline VA, post-operative VA, or visual gain. Patients with at least 2 lines of VA gain had a larger change in macular volume than patients with less than 2 lines gain (p=0.01).
Conclusion: In patients with ERM, macular volume may not be a reliable predictor of baseline or postoperative VA. However, our study suggests that a more favorable outcome of more than 2 lines of VA gained is associated with a higher reduction in macular volume after surgery.
Keywords
Epiretinal membrane, Macular volume, Optical coherence tomography, Vitrectomy, Membrane peel.
Introduction
Epiretinal Membrane (ERM) is a common macular disorder that can lead to blurring or distortion of central vision and has been increasingly characterized with the advent of Optical Coherence Tomography (OCT) imaging [1]. Contracture of ERM causes retinal thickening, distortion of the inner retinal layers, and cystic edema.
This condition affects up to 20% of patients older than 75 years of age [2]. The treatment for visually significant ERM is pars plana vitrectomy and membrane peeling with or without internal limiting membrane peeling.
The goals of surgical intervention are to improve visual acuity (VA) and/or to reduce metamorphopsia [3,4]. However, clinical outcomes vary, and there is currently no model that is predictive of post-operative visual acuity gain based on preoperative clinical characteristics or OCT findings. Many studies have been conducted to examine the relationships between post-operative VA and baseline variables including severity of metamorphopsia, pre-operative VA and various OCT characteristics [4].
OCT features that have been investigated include ellipsoid zone integrity, external limiting membrane integrity, fundus autofluorescence and central foveal thickness [4]. More recently, investigations of the choroidoscleral interface irregularity index and preoperative choroidal circulation have been conducted [5,6].
Most clinical variables and OCT parameter investigations have yielded mixed results or require larger studies to confirm findings, with only a few notable exceptions. Preoperative VA has consistently been shown to correlate with postoperative VA [7].
Additionally, disruption of the ellipsoid zone on pre-operative OCT has been correlated with a poorer visual outcome following surgery [8,9]. More recently, Zeyer et al. reported that a dome-shaped macular contour was correlated with increased visual acuity gain following ERM surgery when compared to a flat or depressed contour [10].
Another easily accessible imaging characteristic that warrants further evaluation is macular volume as measured by OCT. Macular volume is typically above average in eyes with clinically significant ERM, and the macular volume measured by OCT usually decreases after surgical ERM removal [11]. One small study reported VA gain of at least two lines in eyes with higher pre-operative retinal volume [12].
The purpose of our study is to evaluate the correlation between pre and post-operative macular volume with baseline VA and final post-operative visual outcomes in patients undergoing surgical removal of ERM.
Methods
This study was approved by the Institutional Review Board (IRB) of Northwestern University.
A retrospective chart review was performed of patients who underwent pars plana vitrectomy and membrane peeling for epiretinal membrane during the calendar years 2015 through 2019 in the Department of Ophthalmology at Northwestern University. Other inclusion criteria include availability of preoperative and post-operative macular OCT imaging, visual acuity data, and post-operative follow-up exam at least 3 months following surgery.
Patients were excluded from the study if they had any confounding macular pathology, including but not limited to advanced age-related macular degeneration, proliferative diabetic retinopathy, diabetic macular edema, retinal vein occlusion, or myopic degeneration.
Surgery was performed by four different retina surgeons at Northwestern Memorial Hospital using standard three ports pars plana vitrectomy with epiretinal membrane peel, with or without concurrent internal limiting membrane.
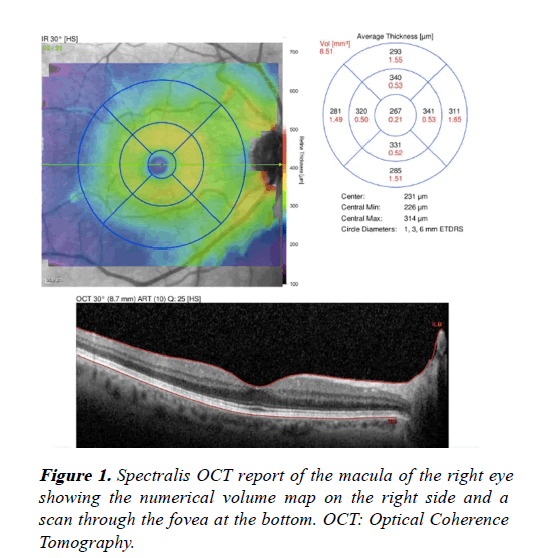
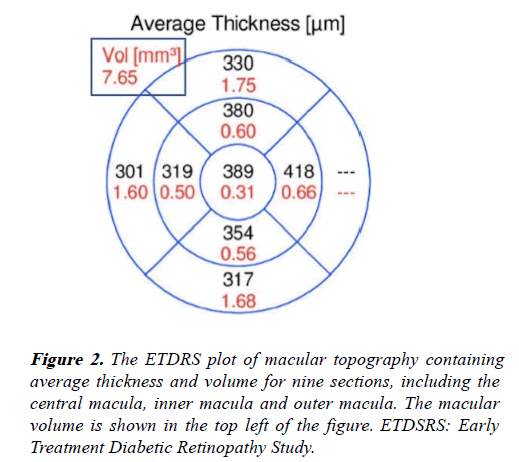
All OCT scans were obtained using the commercially available spectral domain OCT (Spectralis HRA+OCT; Heidelberg Engineering, Inc., Heidelberg, Germany).
Data collected for each patient included age, sex, diagnosis, pre and post-operative visual acuity, presence of metamorphopsia, pre and post-operative OCT macular volume, surgical procedure, and surgical complications. The presence or absence of metamorphopsia was recorded as part of the clinical evaluation prior to surgery.
Pre-operative OCT macular volume was defined as the macular volume obtained from the Spectralis report (Figures 1 and 2) of the most recent OCT scan prior to surgery, and post-operative macular volume was recorded using the OCT scan closest to the patient’s one-year follow-up visit.
Fellow unaffected eyes were used as controls for macular volume. Pre-operative visual acuity was defined as each patient’s Best Corrected Visual Acuity (BCVA) during the clinic visit prior to surgery.
Similarly, post-operative visual acuity was recorded as the patient’s BCVA closest to their one-year follow-up visit. The change in pre-operative to post-operative visual acuity was calculated both in logMAR and Snellen-equivalent lines gained between visits.
A Pearson correlation coefficient was calculated to assess the correlation between pre-operative visual acuity and preoperative macular volume, between the change in pre-operative to post-operative visual acuity and pre-operative macular volume, and between each of these visual acuity variables and post-operative macular volume.
The difference in macular volume between patients with and without metamorphopsia, as well as between patients with greater than and less than 2 Snellen lines of visual acuity improvement was analyzed using a one-tailed t-test.
Results and Discussion
A total of 62 eyes of 62 patients met criteria and were included in the final analysis (Table 1).
| Age (years) | 68 ± 7 (range 43-92) |
|---|---|
| Gender (F:M) | 29:33 |
| Metamorphopsia | 30 (48%) |
| Concurrent ILM peel | 16 (26%) |
| Pre-op lens status | 34 (55%) Phakic* |
| 28 (45%) Pseudophakic | |
| Post-op lens status | 13 (21%) Phakic |
| 49 (79%) Pseudophakic | |
| Follow-up interval (months) | 12 ± 4.4 (range 3-32) |
ILM, internal limiting membrane; pre-op, pre-operative; post-op, post-operative *7 of these patients subsequently developed worse cataract, while 21 underwent cataract surgery.
Table 1: Patient characteristics (n=62).
In this cohort, the mean pre-operative visual acuity was 0.52 ± 0.19 logMAR and the post-operative visual acuity was 0.4 ± 0.32 logMAR. On average, patients in this cohort gained approximately 0.12 logMAR of vision (p-value<0.001).
The mean pre-operative macular volume of eyes with ERM was 11.24 ± 1.60 mm3, which is significantly increased compared to the mean of 8.4 ± 0.44 mm3 in control eyes (pvalue< 0.001). Following surgery, the macular volume was significantly reduced to a mean of 9.29 ± 1.59 mm3 (pvalue< 0.001).
Correlation analysis using Pearson correlation test did not reveal a statistically significant correlation between macular volume and visual acuity either at baseline or post-operatively.
There was also no correlation between pre-operative macular volume with change in post-operative visual acuity (Table 2). There was however, a trend toward a correlation between postoperative change in macular volume with change in visual acuity (r=0.20, p-value=0.13).
| Variables | Pearson correlation coefficient (r) | p-value |
|---|---|---|
| Pre-op macular volume | r=0.05 | 0.71 |
| Pre-op VA | ||
| Pre-op macular volume | r=0.04 | 0.78 |
| VA change | ||
| Post-op macular volume | r=0.05 | 0.72 |
| Post-op VA | ||
| Macular volume change | r=0.20 | 0.13 |
| VA change |
*VA: Visual Acuity; pre-op: pre-operative; post-op: post-operative.
Table 2: Correlation between macular volume and visual acuity.
A subgroup analysis was performed to evaluate the macular volume in patients with at least 2 lines of visual acuity gain (0.2 logMAR) versus those with less than 2 lines gained. Again, no statistically significant difference in either pre-op macular volume or post-op macular volume was detected between the two groups (Table 3). Interestingly, a statistically significant difference in post-operative macular volume change was detected: patients with at least 2 lines of visual acuity gain (n=27) had a larger change in macular volume of 2.45 mm3 compared to 1.60 mm3 change in patients with less than 2 lines of visual acuity gain (p-value=0.01). It is noteworthy that the group of patients who gained at least 2 lines of vision also started out with worse baseline visual acuity, 0.57 logMAR (~20/70) versus 0.48 logMAR (~20/60) (p-value=0.04). Although not statistically significant, these patients tended to have higher baseline macular volume (p-value=0.21) and lower post-operative macular volume (p-value=0.20).
| ≤ 2 lines VA gain (n=35) | ≥ 2 lines VA gain (n=27) | |
|---|---|---|
| Pre-op VA (LogMAR) | 0.48 (~20/60) | 0.57 (~20/70) |
| Post-op VA (LogMAR) | 0.56 (~20/70) | 0.18 (~20/30) |
| VA change (LogMAR) | -0.08 | 0.39 |
| Pre-op macular volume (mm3) | 11.1 | 11.43 |
| Post-op macular volume (mm3) | 9.44 | 9.09 |
| Macular volume change (mm3) | 1.6 | 2.45 |
*VA: Visual Acuity; Pre-Op: Pre-Operative; Post-Op: Post-Operative.
Table 3: Subgroup analysis of patients with ≥ 2 lines VA gain.
In this cohort, about 48% of patients reported the presence of metamorphopsia. There was no significant difference in macular volume (p-value=0.32) between eyes with metamorphopsia (11.34 ± 1.3 mm3) compared to those without (11.15 ± 1.76 mm3).
Optical coherence tomography provides valuable information regarding the architecture of the retina and aids in the diagnosis of many macular diseases including ERM. Understanding the relationship between anatomic parameters and visual function are becoming increasingly important as OCT plays a critical role in the pre-operative evaluation for patients undergoing pars plana vitrectomy for visually significant ERM. Many OCT parameters have already been investigated, but those that have demonstrated association with post-operative outcomes are primarily qualitative. Specifically, ellipsoid zone disruption has been associated with worse visual outcomes while a domeshaped macular contour has been correlated with better visual outcomes [8-10]. Evidence for a reliable quantitative predictive metric would greatly contribute to the evaluation and counseling for patients with ERM.
Our study assesses the relationship between both pre-operative and post-operative macular volume and visual acuity in patients undergoing pars plana vitrectomy for visually significant ERM. As expected, eyes with ERM have a significantly increased OCT macular volume compared to fellow unaffected eyes. However, pre-operative macular volume did not correlate with either pre-operative visual acuity or post-operative visual acuity change. As expected postoperative macular volume was significantly decreased following surgery, however, our study did not find a statistically significant correlation between pre-operative macular volume and visual acuity change. Additionally, there was no difference in pre-op macular volume between eyes with metamorphopsia and those without. From these findings, we conclude that the magnitude of the baseline macular volume is not predictive of baseline visual acuity, presence of metamorphopsia, or potential post-operative visual gain. This is likely due to the lack of correlation between baseline macular volume and ellipsoid zone [8,9] and external limiting membrane integrity, which has been shown to be associated with lower visual acuity when disrupted [13]. However, these findings are consistent with studies of patients with diabetic macular edema (DME) where OCT measurements of retinal thickness were not found to be predictive of visual acuity at any given time point [14]. Another study investigated an OCT parameter referred to as dry retinal volume, which is the adjusted reduced retinal volume after correcting for edema based on normalized retinal reflectivity. In this study of patients with DME although predicted dry retinal volume based on OCT was well-correlated with the actual observed post-treatment retinal volume, there was no correlation between dry retinal volume and visual acuity [15]. This may be explained by the significant neuron loss that occurs in the inner retina in patient with DME that cannot be detected by OCT [16]. There may also be a variable duration of edema and ischemia in these patients which may similarly apply to patients with ERM [17].
Interestingly, although not statistically significant, our study did find a trend towards macular volume change and visual acuity change following surgery. It is possible that with a larger sample size a correlation may be established. Indeed, in the subgroup analysis, patients who gained at least 2 lines of visual acuity had a significantly larger change in macular volume compared to patients with less than 2 lines of visual acuity gain. This suggests that even though there is no direct correlation between visual acuity and macular volume, a favorable visual outcome is associated with a higher reduction of macular volume after surgery reflecting restoration of normal retinal anatomy following vitrectomy. This is consistent with the findings of Kromer et al., who found a significant correlation between macular volume reduction after surgery and visual acuity gain in their study of 45 patients with ERM [12]. However, their study reported that a significant correlation existed between postoperative visual acuity improvement and initial pre-operative perimacular volume, which we did not find in our analysis. Our finding is also consistent with Zeyer et al. who found that a pre-operative domed macular contour (and thus a larger macular volume) correlated with improved post-operative visual gain compared with a pre-operative flat or depressed macular contour [10]. We did attempt to evaluate the relationship between pre-operative domed versus flat macular contour and visual acuity gain in this study. However, our sample size was limited, with only 15% (9/62) of subjects demonstrating a flat macular contour pre-operatively compared to 85% with a domed macular contour. The imbalance in the number of patients with domed versus flat macular contour precluded our ability to detect a statistically significant correlation between this variable and visual acuity gain in this study.
Our study has several other limitations including its retrospective nature and small sample size. Given the retrospective design, several variables could not be controlled including duration of the ERM and lens status. The slow and progressive nature of the condition and subjective reporting of visual decline renders difficulty in identifying the exact onset and duration of the ERM. In this cohort, 34/62 eyes (55%) were phakic at baseline; 21 subsequently underwent cataract surgery, 7 were documented to have progression of cataract, and 6 remained stable with respect to lens grading. Postoperatively, the majority of eyes were pseudophakic (79%) at the end of the follow-up period. Although progression of cataract in 7/62 eyes may confound the post-operative visual acuity, we speculate that the correlation between macular volume and VA or post-operative VA gain is unlikely to be affected because when analyzed separately both the phakic and pseudophakic groups have similar macular volume at baseline (p-value=0.8) and post-operatively (p-value=0.9). The surgical technique also varied among the four surgeons, such as the decision to perform internal limiting membrane and the use of intravitreal triamcinolone. In addition, other OCT characteristics such as the presence of cystic edema, lamellar hole, or ellipsoid zone integrity may confound our results.
Conclusion
The findings of our study offer insights that are useful in the surgical evaluation of ERM. The impact of ERM on visual acuity and metamorphopsia is multi-factorial and more complex than what the anatomic appearance or magnitude of macular volume on OCT suggest. It appears that in patients with ERM, macular volume may not be a reliable predictor of baseline visual function or final visual outcomes following epiretinal membrane surgery. Although not predictive of final visual acuity, a more favorable outcome of more than two lines of visual acuity gained is associated with a higher reduction in macular volume after surgery. Future investigation is warranted to further study this and other OCT parameters that may reliably predict final vision outcomes and aid in the preoperative counselling of patients with ERM.
Acknowlegments
Co-first authors Kasen L. Culler and Hong-Gam Le, MD have contributed equally to this work.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Hussnain SA, Sharma T, Hood DC, et al. Schisis of the Retinal nerve fiber layer in epiretinal membranes. Am J Ophthalmol. 2019;207:304-12.
- Basic and Clinical Science Course. Retina and Vitreous. 2020-2021.
- Watanabe A, Arimoto S, Nishi O. Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology. 2009;116:1788-1793
- Scheerlinck LM, van der Valk R, van Leeuwen R. Predictive factors for postoperative visual acuity in idiopathic epiretinal membrane: A systematic review. Acta Ophthalmol. 2015; 93: 203-12.
- Kim M, Lee Y, Kim RY, et al. Choroidoscleral Interface Irregularity Index: A novel optical coherence tomography-based parameter in patients with epiretinal membrane. Sci Rep. 2020;10:696.
- Rommel F, Brinkmann MP, Sochurek JAM, et al. Ocular blood flow changes impact visual acuity gain after surgical treatment for idiopathic epiretinal membrane. J Clin Med. 2020;9:6.
- Dawson SR, Shunmugam M, Williamson TH. Visual acuity outcomes following surgery for idiopathic epiretinal membrane: An analysis of data from 2001 to 2011. Eye (Lond). 2014;28: 219-24.
- Wong JG, Sachdev N, Beaumont PE, et al. Visual outcomes following vitrectomy and peeling of epiretinal membrane. Clin Exp Ophthalmol. 2005;33:373-378.
- Ghazi-Nouri SMS, Tranos PG, Rubin GS, et al. Visual function and quality of life following vitrectomy and epiretinal membrane peel surgery. Br J Ophthalmol. 2006; 90:559-562.
- Zeyer JC, Parker P, Dajani O, et al. Preoperative domed macular contour correlates with postoperative visual gain after vitrectomy for symptomatic epiretinal membrane. Retina. 2021;41:505-9.
- P. Massin, Allouch C, Haouchine B, et al. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol. 2000;130:732-9.
- Kromer R, Vogt C, Wagenfeld L, et al. Predicting surgical success in patients with idiopathic epiretinal membrane using the spectral-domain optical coherence tomography segmentation module for single retinal layer analysis. Curr Eye Res.2018;43:1024-31.
- Chen X, Zhang L, Sohn EH. et al. Quantification of external limiting membrane disruption caused by diabetic macular edema from SD-OCT. Investigative Ophthalmology & Visual Science. 2012;53:13:8042-8.
- Browning DJ, Glassman AR, Aiello LP, et al., Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007:114:525-36
- Nittala MG, Velaga SB, Hu Z, et al. Relationship between dry retinal volume and visual acuity in diabetic macular edema. Ophthalmic Surg Lasers Imaging Retina. 2018;49:510-5. Jul 1 2018
- Gardner TW, Antonetti DA, Barber AJ, et al. Diabetic retinopathy: More than meets the eye. Survey of Ophthalmology. 2002;47:S253-S262.
- Browning DJ, Stewart MW, Lee C. Diabetic macular edema: Evidence-based management. Indian J Ophthalmol. 2018;66:1736-50.