Research Article - Journal of Clinical Ophthalmology (2018) Volume 2, Issue 1
Changes of corneal endothelial cell density after EX-PRESS® Glaucoma shunt implantation: 2-year follow-up study.
Noriko Toyokawa1, Kaoru Araki-Sasaki1,2, Hiroyuki Nambu3, Hideya Kimura1 and Shinichiro Kuroda1
1Nagata Eye Clinic, Nara, Japan
2JCHO, Hoshigaoka Medical Center, Osaka, Japan
3Nambu Eye Clinic, Nara, Japan
- *Corresponding Author:
- Noriko Toyokawa, MD, PhD
Nagata Eye Clinic, 1147 Kitayamada Hourai
Nara-City, Nara 6310844, Japan
Tel: +81-742-45-2230
E-mail: noritama0620@topaz.ocn.ne.jp
Accepted on February 12, 2018
DOI: 10.35841/clinical-ophthalmology.2.1.41-46
Visit for more related articles at Journal of Clinical OphthalmologyAbstract
Purpose: To evaluate effects of the EX-PRESS® glaucoma filtering device on the corneal endothelial cell density (ECD) in eyes with open angle glaucoma (OAG). Designs: A prospective, non-comparative study. Methods: We prospectively evaluated the changes in the ECD, hexagonality, and coefficient of variation (CV) in 20 eyes of 19 patients who had an implantation of the EX-PRESS®. The type of glaucoma was exfoliation glaucoma in 6 eyes, uveitic glaucoma in 5 eyes, secondary glaucoma following vitrectomy in 4 eyes, primary OAG in 3 eyes, and neovascularization glaucoma in 2 eyes. Corneal specular microscopy was performed at the central cornea before, 1, and 2 years after the EXPRESS ® implantation. Results: The mean ECD was 2008 cells/mm2 before the surgery, 1956 cells/mm2 at 1 year, and 1846 cells/mm2 at 2 years after the surgery which represent a decrease of 5.0% at 1 year and a further decrease of 9.4% at 2 years. The decrease in the ECD from baseline to 1 year was not statistically significant, however the decreases from the baseline to 2 years (P<.0001) and from 1 year to 2 years (P=.0001) were significant. There was a significant change in the CV between the baseline and 1 year (P=0.03), and the change between baseline and 2 years was close to a statistically significant difference (P=0.07). There was no significant change in hexagonality during the 2 years. Two eyes with low preoperative ECD had a marked decrease in the ECD at 2 years. Conclusions: There is a slow decrease in the ECD after the EX-PRESS® implantation.
Keywords
Corneal endothelial cell density, Glaucoma filtering device, EX-PRESS®, Corneal morphology.
Introduction
The number of filtering surgery using glaucoma drainage devices (GDDs) as an alternative to trabeculectomy has increased significantly in the past decade [1]. However, it is known that filtering surgery with or without a GDD can cause corneal endothelial cell loss after the surgery [2-14]. Generally, the implantation of a long tube GDD such as the Ahmed glaucoma valve in the anterior chamber (AC) leads to a greater decrease in the corneal endothelial cell density (ECD) than conventional trabeculetomy [2-7]. The decrease in the ECD is a serious consequence of GDD implantation and is becoming a greater concern along with its frequent use in glaucoma surgeries [1].
The EX-PRESS® glaucoma filtering device is a small and is made of stainless steel and has two advantages; less inflammation because sclerectomy and iridectomy are not needed and lower frequency of postoperative hypotony due to controlled outflow through the unified lumen of the drainage device [16-18]. Although there is evidence that an implantation of the EX-PRESS® device does not affect the ECD in the shortterm [11,15] there have been reported only a few studies of the longer-term (1 year and 2 years) results [12,13].
Thus, the purpose of this study was to determine changes in the ECD and morphology of the corneal endothelial cells after the EX-PRESS® implantation in the long term and compare the results of 1 year and 2 years after the surgery. We prospectively studied 20 eyes of 19 patients with open angle glaucoma (OAG) who underwent the EX-PRESS® implantation. The ECD, hexagonality, and coefficient of variation (CV) were determined before, and at 1 and 2 years after the implantation.
Materials and Methods
Study design
This was a prospective, non-comparative study of 20 eyes of 19 patients with different types of glaucoma.
Institutional review and recruitment
The procedures used were approved by the Institutional Review Board of the Nagata Eye Clinic, and they conformed to the tenets of the Declaration of Helsinki. A signed informed consent form was obtained from each of the patients for the surgical procedures, and the use of any data for future publications. The patients were assured of anonymity.
Patient eligibility
Filtering surgery using the EX-PRESS® Glaucoma Filtration Device (Alcon, Fort Worth, Texas, USA) was performed on patients with OAG with uncontrolled intraocular pressure (IOP) requiring surgical treatment. All patients underwent filtering surgery with an implantation of the EX-PRESS® device between February 2013 and February 2014 at Nagata Eye Clinic, Japan. During this period, filtering surgery using the EX-PRESS® device was performed on 28 eyes of 24 patients. Six eyes of 5 patients were lost to follow-up after the surgery. In the 22 eyes of 19 patients, 2 eyes were excluded because of difficulty in taking a clear image of corneal endothelium with a specular microscope. In the end, 20 eyes of 19 patients were studied. Five eyes with uveitic glaucoma were included, but the inflammation in the AC was silent at the time of surgery in all eyes.
Investigations
The corneal morphology and the position of the EX-PRESS® device within the anterior AC were documented clinically.
Corneal endothelial cells by specular microscopy
Specular microscopy with a noncontact-type specular microscope (Tomey EM-3000, Nagoya, Japan) was performed by 2 experienced examiners before, and 1 and 2 years after the EX-PRESS® implantation. All examinations were carried out on the central cornea. Several clear and high-contrast focused images were taken, and the image with the best clarity was used for the quantitative analyses. The same examiners performed a manual endothelial cell analyses in a masked fashion. After tracing at least 60 cell borders, the ECD, coefficient of cell size variation (CV) or polymegethism, and the percentage of hexagonal cells (hexagonality) or pleomorphism were calculated by a computer software.
Anterior segment optical coherence tomography (ASOCT)
AS-OCT (CASIA SS-1000, Tomey Corporation, Nagoya, Japan) was used to determine the location and orientation of the EX-PRESS® device in the AC. The single scanning mode was performed. The scanning axis was aligned longitudinally over the EX-PRESS® device in the AC so that the device was clearly visible. The position of the EX-PRESS® device in the AC and the central AC depth were measured.
Surgical procedures for implantation
All surgeries were performed by 3 experienced surgeons at the Nagata Eye Clinic with an implantation of a model P-50 EXPRESS ® Glaucoma Filtration Device (Alcon Laboratories, Fort Worth, TX, USA). The surgery was performed using a standard technique. In brief, a fornix-based conjunctival flap was made, and a 3.5 mm square flap was dissected into the clear cornea. Then, 0.04% solution of mitomycin-C (MMC) was applied under the scleral flap and conjunctiva for 3 to 4 min and rinsed with balanced salt solution. A model P-50 EX-PRESS® device was inserted into the AC parallel to the iris. The scleral flap was closed with 4 interrupted 10-0 nylon sutures and the conjunctiva was closed with 10-0 nylon sutures.
Other documented parameters
The baseline data recorded included the age at the time of surgery, sex, type of glaucoma, the number of antiglaucoma medications, number of previous intraocular surgeries, and lens status. The postoperative examinations were made on days 1 and 3, week 1, and 1, 6, 12, and 24 months after surgery. At each follow-up visit, Goldmann tonometry and slit-lamp biomicroscopy were performed. Any complications, e.g., hypotony, were also recorded. Hypotony was defined as an IOP less than 5 mmHg. Laser suture lysis and needling of a bleb were not considered to be additional surgery.
Statistical analysis
All values are expressed as the means ± standard deviations. Wilcoxon’s signed rank test was used to determine the significance of differences in the ECD, polymegathism, and pleomorphism, IOP, and number of antiglaucoma medication before and after surgery. The Fisher exact test was used to compare the demographic data between subjects. Mann- Whitney U tests were used to compare the IOP, the number of medications, and percentage decrease of the ECD between the groups. A P <0.05 was considered statistically significant.
Results
We studied 20 eyes in 19 patients (8 women, 11 men) with a mean age of 71 ± 12 years with a range of 45 to 88 years. The preoperative demographics of the patients are shown in Table 1. The average number of previous intraocular surgeries was 1.6 ± 0.9 including 1 eye that did not have any ocular surgery. All of the eyes that had prior surgery were pseudophakic, and all prior cataract operations were performed using phacoemulsification with intraocular lens implant more than 1 year before the EX-PRESS® implantation.
| No. of patients (eyes) | 19 (20) |
| Age (year) | 71 ± 12 |
| Gender | |
| Male/Female | 11/8 |
| Lens status | |
| Phakia/Pseudophakia | 1/19 |
| Number of prior intraocular operations | 1.6 ± 0.9 |
| Intraocular pressure (mmHg) | 27.1 ± 7.1 |
| Number of antiglaucoma medications | 3.0 ± 1.0 |
| Type of glaucoma (eyes) | |
| Exfoliation glaucoma | 6 |
| Uveitic glaucoma | 5 |
| Secondary glaucoma following vitrectomy | 4 |
| Primary open angle glaucoma | 3 |
| Neovascularization glaucoma | 2 |
Values are presented as mean ± standard deviation
Table 1. Patient’s preoperative demographic and clinical characteristics.
The mean preoperative IOP was 27.1 ± 7.1 mmHg, and the mean IOP was decreased significantly to 13.6 ± 4.1 mmHg at 2 years after the EX-PRESS® implantation (P<0.001). The mean number of preoperative antiglaucoma medications was 3.0 ± 1.0, and 1 patient was taking oral acetazolamide before the EXPRESS ® implantation, and it was counted as 2 medications. The mean number of antiglaucoma medications decreased significantly to 0.8 ± 1.1 at 2 years postoperatively (P<0.001).
A postoperative transient hypotony was observed in 5 eyes (25%), and a transient shallow AC was present in 2 eyes (10%) within 1 month. Persistent hypotony with choroidal effusion and shallow anterior chamber was observed in 2 eyes (cases 1 and 14) (Table 2), and Case 1 required drainage of the choroidal effusion at 1 month after the EX-PRESS® implantation. One eye (case 19) (Table 2) underwent bleb revision at 4 months after the EX-PRESS® implantation. Two eyes underwent additional surgery during the follow-up period.
| Type of glaucoma | ECD baseline | ECD at at 2 years | ECD loss (%) | Persistent hypotony or shallow AC | |
|---|---|---|---|---|---|
| Case 1 | EXG | 1839 | 1677 | 8.8 | YES |
| Case 2 | Uveitic | 2041 | 1693 | 17.1 | NO |
| Case 3 | EXG | 1795 | 1812 | 0 | NO |
| Case 4 | SOAG | 2363 | 2201 | 6.9 | NO |
| Case 5 | EXG | 1436 | 1072 | 25.3 | NO |
| Case 6 | EXG | 1167 | 1082 | 7.3 | NO |
| Case 7 | POAG | 2316 | 2040 | 11.9 | NO |
| Case 8 | POAG | 1463 | 1488 | 0 | NO |
| Case 9 | NVG | 2631 | 2463 | 6.3 | NO |
| Case 10 | Uveitic | 1131 | 667 | 41 | NO |
| Case 11 | Uveitic | 2138 | 2027 | 5.2 | NO |
| Case 12 | NVG | 1958 | 1923 | 1.8 | NO |
| Case 13 | SOAG | 2251 | 2283 | 0 | NO |
| Case 14 | Uveitic | 2960 | 2940 | 0.7 | YES |
| Case 15 | EXG | 2208 | 1956 | 11.4 | NO |
| Case 16 | Uveitic | 2338 | 2252 | 3.7 | NO |
| Case 17 | POAG | 1502 | 1240 | 17.4 | NO |
| Case 18 | EXG | 1935 | 1848 | 4.5 | NO |
| Case 19 | SOAG | 2419 | 2273 | 6 | NO |
| Case 20 | SOAG | 2263 | 1977 | 12.6 | NO |
Cases 7 and 8 are the same patient’s both eyes; ECD: Endothelial Cell Density; AC: Anterior Chamber; EXG: Exfoliation Glaucoma; SOAG: Secondary Open Angle Glaucoma Following Vitrectomy; POAG: Primary Open Angle Glaucoma; NVG: Neovascularization Glaucoma.
Table 2. Details about ECD changes before and after the EX-PRESS® implantation of all eyes.
The location and orientation of the EX-PRESS® device in the AC was good in all eyes as confirmed by slit-lamp and ASOCT examinations. None of the eyes had a touching of the cornea or iris by the EX-PRESS® device. The mean depth of the AC was 3.8 ± 0.4 mm at 6 months after the EX-PRESS® implantation.
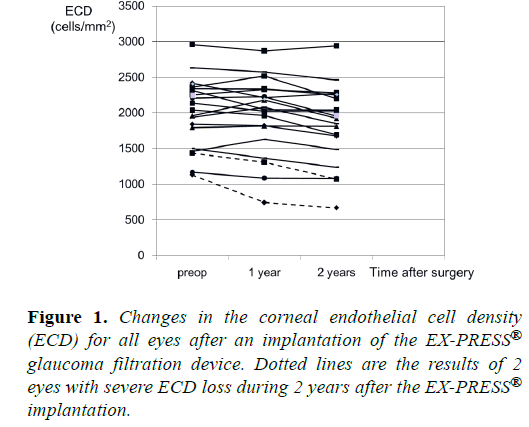
The mean ECD was 2008 ± 482 cell/mm2 before the EXPRESS ® implantation and 1956 ± 537 cells/mm2 at 1 year and 1846 ± 537 cells/mm2 at 2 years after the EX-PRESS® implantation. These represent a decrease of the ECD of 5.0% at 1 year and 9.4% decrease at 2 years. The change between the baseline and 1 year was not statistically significant (P=0.39), however the change between the baseline and 2 years (P<0.001) and between 1 year and 2 years (P=0.001) were both statistically significant. The changes in the ECD of all eyes after the EX-PRESS® implantation are presented (Figure 1). The details about the changes in the ECD of all eyes are shown (Table 2). There were no significant changes in ECD of case 1 and case 14 that developed persistent hypotony and shallow AC.
The morphologic evaluations of the cornea showed no significant changes in the hexagonality index from the baseline to 2 years. In contrast, there was a significant change in CV in the cell area between the baseline and 1 year after the EXPRESS ® implantation (P=0.03), and the change in the CV index between the baseline and at 2 years was not statistically significant (P=0.07; Table 3).
| Hexagonality | Mean ± SD | P value |
|---|---|---|
| Baseline | 48.2 ± 7.1 | |
| 1 year | 48.4 ± 9.3 | 0.7 |
| 2 years | 46.3 ± 11.3 | 0.18 |
| Coefficient of variation | ||
| Baseline | 38.0 ± 7.7 | |
| 1 year | 42.0 ± 7.4 | 0.03 |
| 2 years | 42.2 ± 8.5 | 0.07 |
Table 3. Hexagonality and Coefficient of Variation.
An extensive decrease of more than 25% in the ECD was observed in 2 eyes at 2 years after the EX-PRESS® implantation. A comparison of these two patients, Case 5 and 10 (Table 2), to those without an extensive decrease in the ECD showed that the differences in the sex distribution, age, lens status, previous glaucoma surgery, IOP, number of antiglaucoma medications, and type of glaucoma were not significant. However, these 2 eyes had low ECD preoperatively. A summary of the characteristics of these 2 eyes is presented (Table 4). In addition, these 2 eyes had no persistent postoperative hypotony or shallow AC after the EXPRESS ® implantation.
| Age (years) | 70 | 72 |
|---|---|---|
| Glaucoma Type | Uveitic glaucoma | Exfoliation glaucoma |
| Preop IOP (mmHg) | 22 | 30 |
| Preop number of medication | 3 | 3 |
| IOP at 2 years (mmHg) | 10 | 12 |
| Preop ECD (cells/mm2) | 1131 | 1436 |
| ECD at 1 year (cells/mm2) | 743 | 1309 |
| ECD at 2 years (cells/mm2) | 667 | 1072 |
| ECD loss for 2 years | 464 (41%) | 364 (25%) |
| Prior surgery | PEA-IOL | PEA-IOL |
| Viscocanalostomy | Trabeculotomy with | |
| Deep screlectomy | Deep sclerectomy |
Preope: Preoperative; IOP: Intraocular Pressure; ECD: Endothelial Cell Density; PEA-IOL: Phacoemulsification, Aspiration, and Intraocular Lens Implantation
Table 4. Characteristics of the two eyes with the excessive ECD loss after the EX-PRESS® implantation.
Discussion
Our results showed that there was a non-significant reduction of the ECD at 1 year after the EX-PRESS® implantation, but the decrease continued so that the ECD was then significantly decreased relative to the baseline at 2 years after the EXPRESS ® implantation. The percentage reduction of the ECD was 5% at 1 year and 9.4% at 2 years. There were no specific complications during the operations, and the OCT imaging studies confirmed that the EX-PRESS® device was implanted properly in all eyes. Thus, all of the eyes had a successful implantation of the EX-PRESS® filtering device with minimal insult on the ECD during the surgery. Because of the gradual decrease in the ECD, we suggest that the decrease was not caused by surgical trauma.
An earlier longitudinal study on normal human corneas showed that the corneal endothelial cell reduction rate was 0.6 ± 0.5%/ year throughout the adult life [19]. Because the corneal endothelial cells cannot reproduce, the ECD will continue to decrease irrespective of the surgery. Therefore, we were concerned whether the corneal endothelial decrease after the EX-PRESS® implantation was an ongoing event in addition to the physiological events such as aging process. Previous studies demonstrated that the EX-PRESS® implantation showed no side effects on the ECD in eyes with primary OAG for a short-time periods [11,15]. Thus, the EX-PRESS® implantation is suggested to be appropriate for patients especially with significantly low ECD preoperatively [11]. However, great attention should be paid in the long-term periods, particularly in case that EX-PRESS® was applied to younger patients.
Ishida et al. reported that the ECD decreased significantly from 2529 ± 327 cells/mm2 preoperatively to 2471 ± 356 cells/mm2 (2.2%) at 1 year and to 2428 ± 315 cells/mm2 (4.0%) at 2 years after the EX-PRESS® implantation [13] In Ishida et al.’s study, there was no significant difference in the ECD between the baseline and 1 year, however there was a significant decrease from the baseline to 2 years [13] in agreement with the results of our study. However, the degree of reduction in the ECD in Ishida et al.’s [13] study was smaller than ours which may be due to differences in the experimental protocol. First, Ishida et al. investigated only eyes with primary OAG and they excluded eyes with ECD <2000/mm2. On the other hand, we studied eyes with different kinds of glaucoma and also included eyes with ECD <2000/mm2. Considering the larger loss in corneal endothelial cell in our study, we suggest that type of glaucoma could have affected the corneal endothelium. Second, our findings suggested that low preoperative ECD could be a risk factor for corneal endothelial cell loss. In fact, 2 eyes with preoperative low ECD (Cases 5 and 10) (Table 2) had a greater decrease in the corneal endothelial cells of more than 25% at 2 years after the EX-PRESS® implantation. Although the slight difference was observed, our results are similar to that of Ishida et al.’s results that the EX-PRESS® implantation will affect the ECD in the longer term.
Our observations showed that the CV was significantly increased at 1 year after the implantation compared to the baseline value (P=0.03), and the increase in the CV at 2 years was close to a statistically significant difference (P=0.07). In contrast, there was no significant change in hexagonality during the 2-year follow-up period. Although the hexagonality will usually decrease along with the increase of the CV [20,21], this might be because the changes in the ECD were so gradual that it affected only the CV and not the hexagonality. However, both the CV and hexagonality may be affected after longer follow-up periods.
The morphology including shapes and patterns reflects more the healing process of the corneal endothelial cells rather than cell density as the early events in endothelial damages [8,21]. Thus, we suggest that the changes in the CV was more marked than the changes in the ECD in the first year.?
Because we included the results of different types of glaucoma with comorbid conditions, it is difficult to interpret the findings. We studied 5 eyes with uveitic glaucoma and 6 eyes with exfoliation glaucoma. Eyes with uveitic glaucoma may evoke postoperative inflammation and diminish endothelial function [22]. However, in our cases, the postoperative inflammation was mild, and there was no difference in the corneal ECD before, at 1 year, and at 2 years after the EXPRESS ® implantation between eyes with and without uveitic glaucoma. In addition, some studies have reported the disturbance of ECD in eyes with exfoliation materials [23,24]. However, we found no difference in ECD loss rates at 2 years after the EX-PRESS® implantation between eyes with exfoliation materials and eyes without them.
The exact mechanism causing the decrease in the ECD after the EX-PRESS® implantation has not been determined, but it might be multiple and complex. Many suggestions have been made including the jet flow around the device, inflammation in the AC, intermittent corneal touch due to movements caused by blinking or rubbing the eye, uveal touch by the device, and a foreign body reaction to the implanted device [3,25]. Several studies have reported the risk factors for the reduction in the ECD after the EX-PRESS® implantation, that is, low preoperative ECD [5], peripheral anterior synechiae [6], and the influence of the proximity of the GDD to the corneal endothelium [4,7]. Other factors have also been suggested to affect the ECD, e.g., glaucoma [26], high IOP [26,27] toxicity of the preservatives in the anti-glaucoma drugs [26] hypotony [31], shallow AC during or after surgery [9,25,28,31] use of MMC [29,30] changes in the composition of the aqueous humor, [31] and a combination of these factors [31]. Our results that showed a gradual and continuous decrease in the ECD suggesting that the EX-PRESS® implantation might have changed the homeostasis of the anterior chamber and disturbed the environment of the corneal endothelium continuously [11]. Additional experiments are necessary to determine the factors affecting the homeostasis of the AC and the decrease in the ECD in order to make appropriate improvements of the implanted devices.
The limitations of our study include a small sample size with comorbid conditions in the type of glaucoma, and the absence of a control group composed of eyes with conventional trabeculectomy. Despite these limitations, to the best of our knowledge, this is the first study to evaluate the 1 and 2-year changes in the ECD, CV, and hexagonality after the EXPRESS® implantation. The cell shapes and patterns are more sensitive indicators of endothelial damage than ECD alone [21]. Further comparative studies including morphological changes of the endothelial cells in eyes that had undergone EXPRESS ® implantation should be helpful.
In conclusion, the ECD is significantly decreased for at least 2 years following the EX-PRESS® implantation. This decrease was more severe between 1 year and 2 years after surgery, and two cases with preoperative low ECD had a marked decrease in the ECD after the surgery. Additional long-term studies of the ECD after the EX-PRESS® implantation are needed.
Conflict of Interest
There is no Conflict to disclosure.
References
- Ramulu PY, Corcoran KJ, Corcoran SL, et al. Utilization of various glaucoma surgeries and procedures in Medicare beneficiaries from 1995 to 2004. Ophthalmology. 2007;114:2265-70.
- Minkler DS, Fransis BA, Hodapp EA, et al. Aqueous shunts in glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115:1089-98.
- Topouizis F, Coleman AL, Choplin N, et al. Follow-up of the original cohort with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1999;128:198-204.
- Lee EK, Yun YJ, LE JE, et al. Changes in corneal endothelial cells after Ahmed glaucoma valve implantation: 2-year follow-up. Am J Ophthalmol.2009;148:361-367.
- Kim CS, Yim JH, Lee EK, et al. Changes in corneal endothelial cell density and morphology after Ahmed glaucoma valve implantation during the first year of follow up. Clin Experiment Ophthalmol. 2008;36:142-7.
- Hau S, Scot A, Bunce C, et al. Corneal endothelial morphology in eyes implanted with anterior chamber aqueous shunts. Cornea. 2011;30:50-5.
- Koo EB, Hou J, Han Y, et al. Effect if glaucoma tube shunt parameters on cornea endothelial cells in patients with Ahmed valve implants. Cornea. 2015;34:7-41.
- Storr-Paulsen T, Norregaard JC, Ahmed S, et al. Corneal endothelial cell loss after mitomycin C-augmented trabeculectomy. J Glaucoma. 2008;17: 654-7.
- Smith DL, Skuta GL, Lindenmuth KA, et al. The effect of glaucoma surgery on corneal endothelial cell density. Ophthalmic Surg. 1991;22:251-5.
- Arnavielle S, Lafontaine PO, Bidot S, et al. Corneal endothelial cell changes after trabeculectomy and deep sclerectomy. J Glaucoma. 2007;16:324-8.
- Casini G, Loiuduce P, Pellegrini M, et al. Trabeculectomy versus EX-PRESS shunt versus Ahmed Valve Implant: short-term effect on corneal endothelial cells. Am J Ophthalmol. 2015;160:1185-90.
- Konopinska J, Deniziak M, Saeed E, et al. Prospective randomized study comparing combined phaco-ExPress and phacotrabeculectomy in open angle glaucoma treatment: 12-month follow-up. J Ophthalmol. 2015(E-Pub Jun 7).
- Ishida K, Moroto N, Murata K, et al. Effect of glaucoma implant surgery on intraocular pressure reduction, flare count, anterior chamber depth, and corneal endothelium in primary open-angle glaucoma. Jpn J Ophthalmol. 2017;61:334-46.
- Tojo N, Hayashi A, Miyakoshi A. Corneal decompensation following filtering surgery with the EX-PRESS® mini glaucoma shunt device. Clin Ophthalmol. 2015;9:499-502.
- Wagschal LD, Trope GE, Jinapriya D, et al. Prospective randomized studycomparing EX-PRESS to trabeculectomy: 1-year results. J Glaucoma. 2015;24(8):624-9.
- Maris PJ Jr, Ishida K, Netland PA. Comparison of trabeculectomy with EX-PRESS miniature glaucoma device implant under scleral flap. J Glaucoma. 2007;16:14-19.
- Kanner EM, Netland PA, Sarkisian SR, et al. EX-PRESS miniature glaucoma device implanted under a scleral flap alone or combined with phacoemulsification cataract surgery. J Glaucoma. 2009;18(6):488-91.
- Netland PA, Sarkisian SR, Moster MR, et al. Randomized, prospective, comparative trial of EX-PRESS glaucoma filtration device versus trabeculectomy (XVT Study). Am J Ophthalmol. 2014;157:430-4.
- Bourne WM, Nelson LR, Hodge DO. Central corneal endothelial cell changes over a ten-year period. Invest Ophthalmol Vis Sci. 1997;38:779-82.
- Mishima S. Clinical investigations on the corneal endothelium. Ophthalmology. 1982;89:525-30.
- Matsuda M, Suda T, Manabe R. Serial alterations in endothelial cell shape and pattern after intraocular surgery. Am J Ophthalmol. 1984;98:313-9.
- Sagoo P, Chan G, Larkin DF, et al. Inflammatory cytokines induce apotosis of corneal endothelium through nitric oxide. Invest Ophthalmol Vis Sci. 2004;45(11):3964-73.
- Miyake K, Matsuda M, Inaba M. Corneal endothelial changes in pseudoexfoliation syndrome. Am J Ophthalmol. 1989;108:49-52.
- Wirbelauer C, Anders N, Pham DT, et al. Corneal endothelial cell changes in pseudoexfoliation syndrome after cataract surgery. Arch Ophthalmol. 1998;116:145-9.
- McDermott ML, Swendris RP, Shin DH, et al. Corneal endothelial cell counts after Molteno implantation. Am J Ophthalmol. 1993;115:93-6.
- Gagnon MM, Boisjoly HM, Brunette I, et al. Corneal endothelial cell density in glaucoma. Cornea. 1997;16:314-8.
- Bigar F, Witmer R. Corneal endothelial changes in primary acute angle closure glaucoma. Ophthalmology.1982;89:596-9.
- Fiore PM, Ritcher CU, Arzeno G, et al. The effect of anterior chamber depth on endothelial cell count after filtration surgery. Arch Ophthalmol. 1989;107:1609-11.
- Dreyer EB, Chaturvedi N, Zurakowski D. Effect of mitomycin C and fluorouracil-supplemented trabeculectomies on the anterior segment. Arch Ophthalmol. 1995;113:578-80.
- McDermott ML, Wang J, Shin DH. Mitomycin and the human corneal endothelium. Arch Ophthalmol. 1994;112:533-7.
- Koley M, Gieser D, Kass MA, et al. Central corneal endothelial cell density and central corneal thickness in ocular hypertension and primary open-angle glaucoma. Am J Ophthalmol. 1982;94:610-6.
- Cairns JE. Trabeculectomy. Preliminary report by a new method. Am J Ophthalmol. 1968;66:673-9.