Mini Review - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 4
Changes in central corneal thickness before and after phacoemulsification cataract surgery
May D’souza, Dilon Noronha*
Department of Ophthalmology, Father Muller Medical College, Mangaluru, India
- Corresponding Author:
- Dilon Noronha
Department of Ophthalmology
Father Muller Medical College
Mangaluru
India
E-mail: dilonnoronha@gmail.com
Accepted date: April 7, 2020
Citation: Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.
Abstract
Aim: To evaluate the effect of an uneventful phacoemulsification surgery on Central Corneal thickness (CCT).
Methods: 77 consecutive patients who had an uneventful phacoemulsification surgery by the same experienced surgeon were prospectively evaluated for Intraocular Pressure (IOP) and CCT measurements 1 day preoperatively and 1 day, 1 week and 1 month postoperatively.
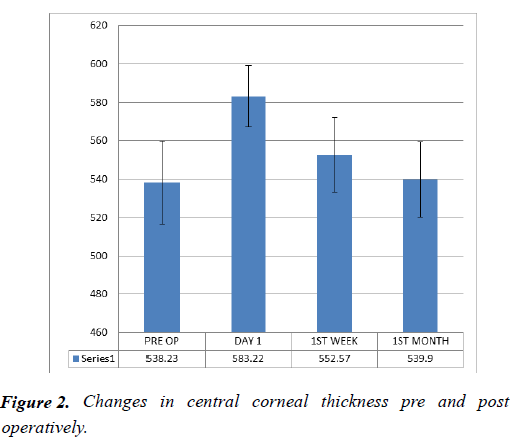
Result: A marked rise was seen in the mean CCT measured within 24 hours after surgery (583.22 μm), which gradually decreased at one week (552.57 μm) and returned to normal baseline values (539.9 μm) in almost all operated eyes in 1 month time. There is no statistically significant difference in the mea n CCT before surgery (538.23 μm) and at 1 month (p=0.685).
Conclusion: The mean CCT substantially increases after post-operative uneventful cataract surgery but returns to normal baseline values in almost all operated eyes in 1 month time. IOP measured during this period may be falsely higher than the true values due to increased CCT and thus not all IOP rises have to be treated during this period.
Keywords
Central corneal thickness, Intraocular pressure, Phacoemulsification
Introduction
The corneal endothelium plays an important role in maintaining corneal transparency. Deturgescence of the corneal stroma is controlled by the pumping action of the endothelial layer and can be monitored by measurement of central corneal thickness (CCT). Studies have shown that intraocular surgeries affect corneal endothelial density. Interest has therefore developed in the assessment of endothelial damage either by cell counts or indirectly by measuring corneal thickness postoperatively. Central corneal thickness (CCT) increases significantly immediately after cataract surgery and gradually returns to normal values over the next few weeks [1,2]. CCT is an important predictor of IOP [3,4]. Thicker the cornea, greater the false IOP readings.
The purpose of this study is to describe changes occurring in central corneal thickness before and after uneventful phacoemulsification surgery.
Materials and Methods
This Prospective observational study involved 77 patients that presented to the Department of Ophthalmology in Father Muller Medical College hospital, Kankanady. The study was conducted over a period of 2 months.
Consecutive patients aged 18 years and above enrolled for Phacoemulsification cataract surgery with intraocular lens implantation performed by the same surgeon formed the study patients.
Excluded from the study were patients with corneal degeneration, corneal dystrophy, corneal opacity, traumatic or complicated cataract and those with high pre-operative astigmatism of ≥ 2.5 D. Other excluded patients were those who have had refractive surgeries, those with only one eye, those with operative complications such as vitreous loss, and those who declined participation in the study.
A written Informed consent was obtained. Patient was explained about the procedure in their own understandable language. Brief history and clinical examination was carried out in every patient. IOP was recorded using Goldman ’ s applanation tonometer and CCT was measured using Ultrasonic Pachymeter under topical Anaesthesia (proparacaine HCl 0.5%). Measurements were taken prior to surgery and at follow-up at 1, 7, and 30 days postoperatively.
Surgical procedure
Mydriasis was obtained before surgery with Tropicacyl plus eye drops (tropicamide 0.4%, phenylephrine hydrochloride 5% and Chlorbutol 0.5%). Under topical anaesthesia with proparacaine HCl 0.5% and a peribulbar block, a clear cornea 2.8‐mm incision was performed. Sodium hyaluronate was used as viscoelastic substance. Phacoemulsification of the nucleus was performed with an Alcon Infinity unit, using phaco‐chop technique, followed by the aspiration of cortical remnants and polishing of the capsular bag. A foldable onepiece acrylic intraocular lens was implanted in the capsular bag using an injector. The viscoelastic substance was aspirated meticulously using an irrigation/aspiration tip. Main incision was left suture less.
Statistical analysis
Paired‘t’ test was used to analyse the IOP changes before and after Phacoemulsification (Table 1).
| Pre-op IOP | Post-op IOP | df | p | |
|---|---|---|---|---|
| Mean | 15.8143 | 13.2597 | 76 | <0.0001 |
Table 1. IOP changes before and after phacoemulsification.
Repeated measures ANOVA and Turkey HSD test was used to compare the changes in the mean CCT over time (Table 2).
| Anova summary: | |||||
|---|---|---|---|---|---|
| Source of variation | SS | df | MS | F | p |
| Treatment (b/w groups) | 100250.659 | 3 | 33416.9 | 376.21 | <0.0001 |
| Error | 20252.0909 | 228 | 88.825 | ||
Table 2a. Anova summary: Changes in mean CCT before and after phacoemulsification.
| Tukey HSD Test: | |
|---|---|
| Mean CCT | p |
| CCT0 Vs. CCT1 | <0.01 |
| CCT0 Vs. CCT2 | <0.01 |
| CCT0 Vs. CCT3 | Non-significant |
| CCT1 Vs. CCT2 | <0.01 |
| CCT1 Vs. CCT3 | <0.01 |
| CCT2 Vs. CCT3 | <0.01 |
*CCT0=Mean CCT preoperatively; CCT1=Mean CCT Postoperatively on day 1; CCT2=Mean CCT postoperatively after 1 week; CCT3=Mean CCT postoperatively after 1 month
Table 2B. Tukey HSD Test: Changes in mean CCT before and after phacoemulsification.
Results
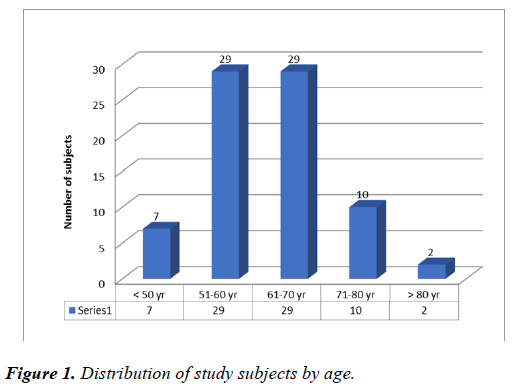
A total of 77 patients that underwent a clear corneal phacoemulsification surgery were enrolled in this study out of which 41(53%) were men and 36(47%) were women; mean age of the study population was 61. 58 ± 9.46 years (Figure 1). 44% of the patients had comorbidities-Diabetes only {8%}, Hypertension only {8%} or both{28%. Twentyfour right and Fifty-three left eyes were operated on and analysed.
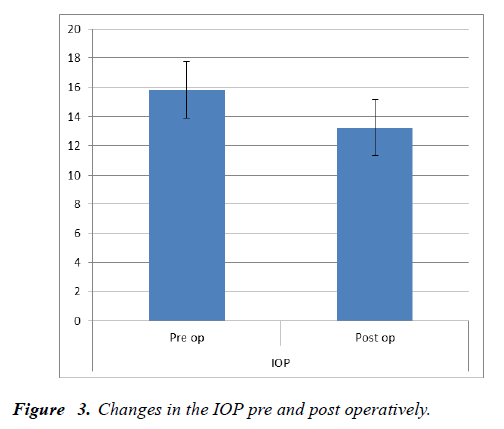
The mean CCT was 538.23 μm preoperatively, 583.22 μm 1 day postoperatively and 552.57 μm 1 week postoperatively and 539.9 μm 1 month postoperatively as depicted in Figure 2 Statistically significant differences between preoperative values and the ones in the first postoperative day and in 1 week postoperatively were found for CCT (p<.01). The mean IOP was 15.81 mmHg preoperatively and 13.25 mmHg postoperatively as shown in Figure 3.
Discussion
The cornea is composed of six layers: epithelium, Bowman’s layer, stroma, Dua ’ s layer, Descemet ’ s membrane and endothelium. The stroma has a tendency to swell under normal physiological conditions. This swelling is prevented by active fluid pumping of the endothelium, thereby assuring maintenance of normal thickness and transparency of the cornea [5].
The aim of our study was to explore the effect of uncomplicated phacoemulsification on central corneal thickness. Phacoemulsification may influence the barrier function of the endothelium due to endothelial cell loss during surgery. The transient post-operative corneal swelling that commonly occurs after phacoemulsification is probably the result of damage to endothelial cells by the surgery [6]. Many factors can cause endothelial injury during cataract surgery, such as direct mechanical trauma, ultrasound energy, and the irrigating solution [7]. Endothelial cells are non-replicative, and consequently the damaged area is covered by incomplete enlargement and migration of residual cells [5].
Michaeli et al. [8] compared CCT and endothelial cell loss after phacoemulsification with clear cornea and scleral tunnel incisions. They found that corneal thickness increased significantly in all measurements postoperative and returned to baseline by 3 months and there was no difference in the pachymetry change between the two study groups.
[3,4] Other research studies showed that CCT returned to normal in most operated eyes following an initial increase 1 week after an uneventful cataract surgery. Our study showed a marked increase in the mean CCT after uneventful phacoemulsification surgery that returned to normal baseline values in majority of the operated eyes at 1 week, touching near normal baseline values at 1 month. Compared with the baseline, there is a mean increase in CCT of 44.99 μm at 1 day, and 14.34 μm at 1 week, and 1.67 μm at 1 month. The mean increase at day 1 was higher than that reported by others like Salvi et al. [1] reported a mean increase of 3.15 μm at week 1.
Possible explanations:
• Difference in the population studied
• Duration of surgery
• Density of cataract
IOP measured postoperatively in the 1st week may be falsely elevated due to increased CCT in the immediate postoperative period; thus, not all IOP rises have to be treated in this period in healthy uncompromised eyes.
Conclusion
Our study showed:
• Mean CCT substantially increases after uneventful phacoemulsification.
• Returns to normal baseline values in almost all operated eyes in one month time.
• Caution to be taken while interpreting the results of intraocular pressure measurements during this period.
Conflicts of interest
There are no conflicts of interest.
Limitations
One of the limitations in our study was that it was not randomized. Secondly, only one technique of phacoemulsification was used; results may have varied if other techniques were used. Thirdly, Ultrasound pachymetry was taken instead of specular microscopy for documenting endothelial dysfunction. Measurements estimated by ultrasonic pachymetry are more variable.
Ethical Clearance
The Ethical clearance was obtained from Institutional Ethics Committee, Father Muller Medical College.
References
- Salvi SM, Soong TK, Kumar BV, et al. Central corneal thickness changes after phacoemulsification cataract surgery. J Cataract Refract Surg. 2007;33:1426-8.
- Falkenberg B, Kutschan A, Wiegand W. Analysis of optical parameters after cataract surgery and implantation of foldable lens. Ophthalmologe. 2005;102:587-91.
- Brandt JD. The influence of corneal thickness on the diagnosis and management of glaucoma. J Glaucoma. 2001;10:S65-7.
- Chu J, Tham YC, Liao J, et al. Ethnic differences of intraocular pressure and central corneal thickness; the Singapore Epidemiology of Eye Diseases study. Ophthalmology. 2014;121:2013-22.
- Mishima S. Clinical investigations on the corneal endothelium-XXXVIII Edward Jackson Memorial Lecture.Am J Ophthalmol. 1982;93: 1-29.
- Bolz M, Sacu S, Drexler W, et al.Local corneal thickness changes after small-incision cataract surgery.J Cataract Refract Surg. 2006;32:1667-71.
- Behndig A, Lundberg B. Transient corneal edema after phacoemulsification: comparison of 3 viscoelastic regimens.J Cataract Refract Surg. 2002;28:1551-6.
- Michaeli A, Rootman DS, Slomovic AR. Corneal changes after phacoemulsification with a corneal versus a scleral tunnel incision. Harefuah. 2006;145:191-3.