Research Paper - Archives of General Internal Medicine (2017) Volume 1, Issue 3
Assessment of Cardiovascular Disease in Rheumatoid Arthritis Patients
Daniel Li1, Alex Meara2*, Brian LaMoreaux2, Guy Brock3 and Wael Jarjour2
1College of Medicine, The Ohio State University, USA
2Department of Rheumatology, Wexner Medical Center, The Ohio State University, USA
3Department of Biomedical Informatics and Center for Biostatistics, Wexner Medical Center, The Ohio State University, USA
- *Corresponding Author:
- Alexa Meara
Rm S2056 Davis Medical Research Center
480 Medical Center Dr, Columbus
OH 43210 USA
E-mail: alexa.meara@osumc.edu
Accepted on August 30, 2017
Citation: Li D, Meara A, LaMoreaux B, et al. Assessment of cardiovascular disease in rheumatoid arthritis patients. Arch Gen Intern Med. 2017;1(3):15-22
Abstract
Introduction: The risk of cardiovascular disease is increased in patients with rheumatoid arthritis. Previous studies have compared cardiovascular disease risk factors between patients with and without rheumatoid arthritis, but none have compared rheumatoid arthritis patients with and without cardiovascular disease. To compare rheumatoid arthritis patients with and without cardiovascular disease in addition to cardiovascular disease patients without rheumatoid arthritis.
Methods: Retrospective cross sectional study from 2011-2014 of rheumatology, cardiology, internal medicine, and family medicine clinics at a multi-site academic medical center.
Participants: Rheumatoid arthritis patients had the international classification of disease code “rheumatoid arthritis”. Cardiovascular disease patients had at least one of following codes: peripheral artery disease, coronary artery disease, diabetes, stroke, abdominal aortic aneurysm, transient ischemic attack, or myocardial infarction. All eligible patients were included in the study. Patients were divided into three groups: 2,305 patients with only rheumatoid arthritis, 276 patients with rheumatoid arthritis and cardiovascular disease, and 13,473 patients with only cardiovascular disease. Descriptive statistics was performed.
Results: Only 11,490 (72%) of patients had a full lipid panel available. However, patients with and without a full lipid panel did not differ in age, gender, smoking status, body mass index, or systolic and diastolic blood pressure. Patients with only rheumatoid arthritis had low density lipoprotein levels 19% higher than patients with rheumatoid arthritis and cardiovascular disease (p<0.001, 95% CI: [1.10, 1.28],) and 16% greater than patients with only cardiovascular disease (p<0.001,95% CI: [1.12, 1.20],). Patients with only rheumatoid arthritis also had greater cholesterol and high density lipoprotein levels, but lower triglyceride levels.
Conclusion: Patients with rheumatoid arthritis without known cardiovascular disease do not undergo the same aggressive treatment to improve their lipid profile as patients with cardiovascular disease with or without rheumatoid arthritis. Healthcare profession
Keywords
Rheumatology, Arthritis, Cardiovascular disease, Chronic disease.
Introduction
Rheumatoid Arthritis (RA) is a chronic systemic inflammatory autoimmune disease that causes arthritis with joint destruction. RA occurs in about one percent of the population, most commonly around age 30-50, and affects twice as many females as males [1]. The top cause of mortality among RA patients is Cardiovascular Disease (CVD) [2,3], which occurs on average 10 years earlier in RA patients than in the general population [4].
Even when traditional risk factors such as hypertension, tobacco abuse, diabetes, and dyslipidemia are accounted for, there is still an elevated CVD risk associated with having RA [5,6]. This increased risk of CVD in RA patients is likely due to both the systemic inflammation that occurs in RA and the earlier occurrence of traditional CVD risk factors [7]. Because of the increased CVD risk in RA patients, it is also recommended that RA patients undergo CVD risk assessmentand management according to established guidelines despite the patients’ age [8,9].
CVD risk is associated with an observed increase in low density lipoprotein (LDL-cholesterol) levels and subsequently low high density lipoprotein (HDL-cholesterol) levels; inflammatory responses in RA cause patients have a low HDL-cholesterol as seen with CVD patients, but paradoxically a low LDL-cholesterol, as well [10]. This pattern has also been seen in other chronic inflammatory diseases such as sepsis and cancer [11] and several studies have even found continued increases in lipid levels in RA patients after reduction in disease activity with treatment [12]. The mechanisms which explain this pattern are not fully understood, but may include up regulation of the reticuloendothelial system increasing LDL clearance and reduced low-density lipoprotein particle synthesis [10].
While many studies have focused on differences between patients with and without RA, none to our knowledge have examined the differences between RA patients with and without high risk CVD. In this study, we examine the clinical profiles of patients with RA but no CVD, patients with both RA and CVD, and patients with CVD but no RA. We analyzed data from thousands of patients from various clinics at a single academic institution. Investigating these different populations may provide new insights into how rheumatoid arthritis patients are managed with respect to cardiovascular disease.
Methods
With Investigational Review Board (IRB) approval, retrospective data were collected from clinic encounters from the years 2011-2014 from rheumatology, internal medicine, family medicine, and cardiovascular medicine clinics at The Ohio State University Wexner Medical Center. International Classification of Disease (ICD-9) codes were used for patient selection. Patients had codes for RA and/or high-risk CVD (peripheral arterial disease, coronary artery disease, diabetes, stroke, abdominal aortic aneurysm, transient ischemic attack, and myocardial infarction). All patients were older than 17 years. Three groups were formed: one group with RA but no CVD, a second group with both RA and CVD, and a third group with CVD but not RA.
Data were gathered based on demographics and modifiable cardiovascular risk factors including age (years), sex, systolic and diastolic blood pressure (BP, mmHg), body mass index (BMI, kg/m2), and smoking status. A full lipid panel including total cholesterol, high-density lipoproteins (HDL, mg/dL), lowdensity lipoproteins (LDL, mg/dL), and triglycerides (TG, mg/ dL) was also available. Other variables included rheumatoid factor (RF, units/mL) levels, and cyclic citrullinated protein (CCP, units/mL) levels.
We performed separate analyses on i) all patients and ii) on patients with a full lipid panel available and seropositive status (defined below). Unusually high or low measurements outside the following ranges were excluded from analyses: cholesterol <50 or >400 mg/dL, HDL <10 or >150 mg/dL, LDL <20 or >300 mg/dL, TG <20 or >650 mg/dL, systolic BP <60 or >250 mmHg, diastolic BP <30 or >150 mmHg and BMI <14 or >100 kg/m2. RF positive status was defined as RF >20 and vice versa, and CCP positive status was defined as CCP >10 and vice versa. Seropositive status was defined as being RF and/or CCP positive. Seronegativity was defined as being RF and/or CCP negative while not being seropositive.
Statistical analyses were performed in R (R Core Team). Analysis of Variance (ANOVA) and chi-squared tests were used to compare the continuous and categorical variables respectively between the three study groups. We set α=0.05 and used Bonferroni’s correction to adjust for multiple testing. For variables that were statistically significant, we then compared the different study groups in a pairwise manner. For pairwise comparisons of cholesterol, HDL, LDL, and triglycerides, we looked at patients with a full lipid panel and seropositive status. For all other pairwise comparisons, we looked at all patients. The Tukey-Kramer method was used for continuous variables and chi-squared tests for categorical variables. We set α=0.05 and used Bonferroni’s correction (based on 3 total pairwise comparisons) to adjust for multiple testing for chi-squared tests. The Tukey-Kramer method automatically adjusts for multiple testing in ANOVA. A log transformation was applied as needed for skewed distributions. We also stratified each of the three groups by lipid panel availability and compared these subgroups to assess for potential bias due to missing data. Statistical methods were determined using guidelines from the Handbook of Biological Statistics [13].
Results
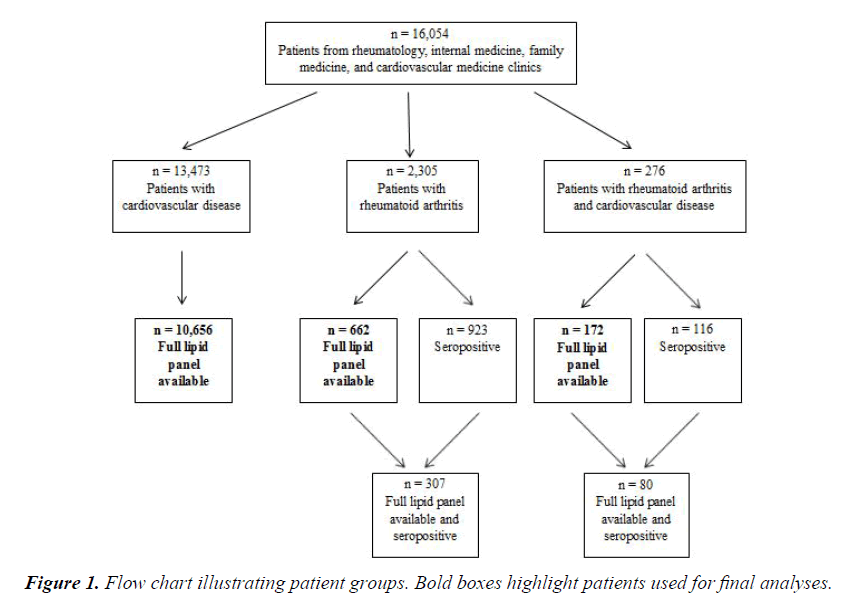
Figure 1 illustrates the patient groups in our analysis. Data were collected on 16,054 patients from rheumatology, internal medicine, family medicine, and cardiovascular medicine clinics. In total, there were 13,473 CVD patients, 2,305 RA patients, and 276 RA and CVD patients. After removing patients that did not have a full lipid panel, there were 10,656 CVD patients, 662 RA patients, and 172 RA and CVD patients.
The distributions of BMI, systolic blood pressure, diastolic blood pressure, cholesterol, HDL, LDL, and triglycerides were found to be right skewed and a log transformation was applied before statistical testing. Table 1 summarizes the characteristics of the different study populations for all patients. Statistically significant differences in age, sex, smoking status, BMI, systolic blood pressure, and diastolic blood pressure were found between the three groups. However, many patients were missing data for lipid related measurements (such as 70% rheumatoid arthritis only patients missing cholesterol measurements), so it would be inappropriate to draw conclusions concerning these measurements from this table.
| High Risk Cardiovascular Disease (n=13,473) | Rheumatoid Arthritis (n=2,305) | Rheumatoid Arthritis and Cardiovascular Disease (n=276) | P-value | |
|---|---|---|---|---|
| Age at evaluation, years | - | - | - | <0.001* |
| Mean (SD) | 60 (14) | 56 (14) | 61 (12) | |
| Gender | - | - | - | <0.001* |
| Female | 6,959 (52%) | 1,808 (78%) | 207 (75%) | |
| Smoking status | - | - | - | <0.001* |
| Never smoker | 6,024 (45%) | 1,184 (51%) | 102 (37%) | |
| Former smoker | 4,909 (36%) | 683 (30%) | 119 (43%) | |
| Current smoker | 2,454 (18%) | 429 (19%) | 51 (18%) | |
| Missing | 86 (1%) | 9 (0%) | 4 (1%) | |
| BMI, kg/m2 | - | - | - | <0.001* |
| Median (IQR) | 31.6 (10.7) | 28.6 (9.3) | 32.2 (11.2) | |
| Missing | 699 (5%) | 92 (4%) | 6 (2%) | |
| Excluded | 8 | 1 | 0 | |
| Systolic BP, mmHg | - | - | - | 0.001* |
| Median (IQR) | 126 (20) | 128 (24) | 129 (22) | |
| Excluded | 0 | 0 | 0 | |
| Diastolic BP, mmHg | - | - | - | <0.001* |
| Median (IQR) | 76 (14) | 78 (14) | 77 (12) | |
| Excluded | 2 | 0 | 0 | |
| Cholesterol, mg/dL | - | - | - | N/A |
| Median (IQR) | 163 (56) | 182 (52) | 168 (56) | |
| Missing | 2,578 (19%) | 1,618 (70%) | 99 (36%) | |
| Excluded | 11 | 2 | 0 | |
| HDL, mg/dL | - | - | N/A | |
| Median (IQR) | 43 (16) | 51 (20) | 46 (20) | |
| Missing | 2,598 (19%) | 1,620 (70%) | 100 (36%) | |
| Excluded | 10 | 3 | 0 | |
| LDL, mg/dL | - | - | - | N/A |
| Median (IQR) | 88 (44) | 100 (40) | 86 (39) | |
| Missing | 2,817 (21%) | 1,643 (71%) | 104 (38%) | |
| Excluded | 58 | 0 | 1 | |
| Triglycerides, mg/dL | - | - | - | N/A |
| Median (IQR) | 127 (102) | 100 (84) | 125 (104) | |
| Missing | 2,584 (19%) | 1,623 (70%) | 99 (36%) | |
| Excluded | 78 | 2 | 2 |
Table 1. Characteristics of all patients. *Indicates statistical significance at p<0.008.
To investigate if potential bias would be introduced if we restricted our analysis to only patients with a full lipid panel available, we compared patients with and without a full lipid panel. These analyses showed that demographic variables appear similar between patients with and without a full lipid panel. For example, the median BMIs between patients with lipid panels available and unavailable are similar between CVD patients (31.8 vs. 31.0 kg/m2 respectively), RA patients (28.1 vs. 28.8 kg/m2), and RA and CVD patients (32.5 vs. 31.4 kg/m2). Likewise, the median systolic blood pressures between patients with lipid panels available and unavailable are also similar between CVD patients (126 vs. 128) mmHg, RA patients (126 vs. 128 mmHg), and RA and CVD patients (129 vs. 129 mmHg).
Table 2 summarizes the characteristics of the different study populations for patients with a full lipid panel. There were statistically significant differences in cholesterol, HDL, LDL, and triglyceride levels between the three groups. It would be more appropriate to draw conclusions on age, sex, smoking status, BMI, systolic blood pressure, and diastolic blood pressure from Table 1 because of the larger sample size. Likewise, it would be more appropriate to draw conclusions on cholesterol, HDL, LDL, and triglycerides from Table 2 because it addresses the missing lipid data issue.
| Cardiovascular Disease (n=10,656) | Rheumatoid Arthritis (n=662) | Rheumatoid Arthritis and Cardiovascular Disease (n=172) | P-value | |
|---|---|---|---|---|
| Age at evaluation, years | - | - | - | N/A |
| Mean (SD) | 59 (14) | 58 (13) | 62 (12) | |
| Gender | - | - | - | N/A |
| Female | 5,553 (52%) | 512 (77%) | 127 (74%) | |
| Smoking status | - | - | - | N/A |
| Never smoker | 4,902 (46%) | 355 (54%) | 60 (35%) | |
| Former smoker | 3,845 (36%) | 225 (34%) | 79 (46%) | |
| Current smoker | 1,854 (17%) | 80 (12%) | 30 (17%) | |
| Missing | 55 (1%) | 2 (0%) | 3 (2%) | |
| BMI, kg/m2 | - | - | - | N/A |
| Median (IQR) | 31.8 (10.7) | 28.1 (9.5) | 32.5 (10.7) | |
| Missing | 573 (5%) | 29 (4%) | 5 (3%) | |
| Excluded | 5 | 0 | 0 | |
| Systolic BP, mmHg | - | - | - | N/A |
| Median (IQR) | 126 (20) | 126 (24) | 129 (24) | |
| Excluded | 0 | 0 | 0 | |
| Diastolic BP, mmHg | - | - | - | N/A |
| Median (IQR) | 76 (13) | 78 (13) | 76 (13) | |
| Excluded | 2 | 0 | 0 | |
| Cholesterol, mg/dL | - | - | - | <0.001* |
| Median (IQR) | 163 (55) | 181 (52) | 168 (54) | |
| Excluded | 6 | 1 | 0 | |
| HDL, mg/dL | - | - | - | <0.001* |
| Median (IQR) | 43 (14) | 51 (20) | 46 (20) | |
| Excluded | 9 | 3 | 0 | |
| LDL, mg/dL | - | - | - | <0.001* |
| Median (IQR) | 88 (44) | 100 (40) | 86 (40) | |
| Excluded | 58 | 0 | 0 | |
| Triglycerides, mg/dL | - | - | - | <0.001* |
| Median (IQR) | 126 (101) | 98 (80) | 125 (106) | |
| Excluded | 28 | 2 | 1 |
Table 2. Characteristics of patients with a full lipid panel. *Indicates statistical significance at p<0.013.
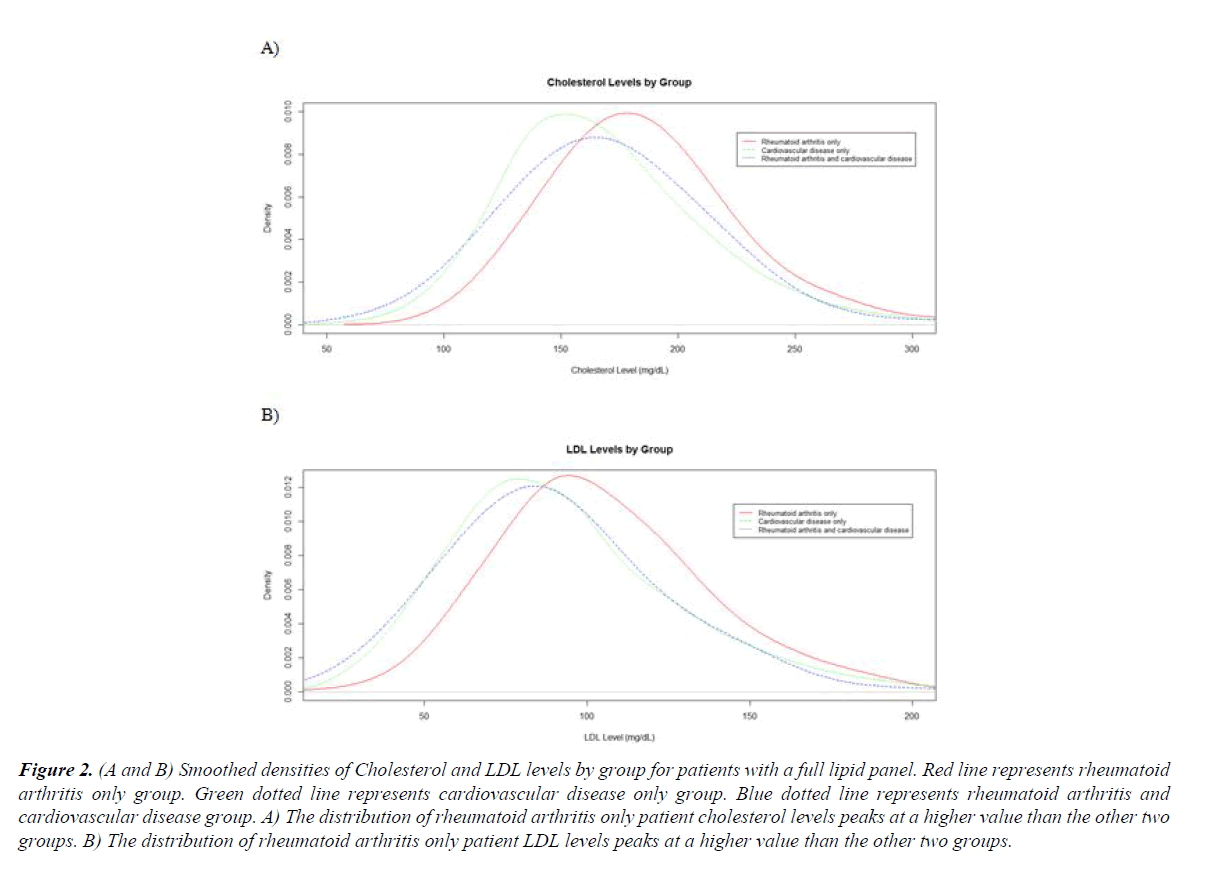
Table 3 shows group by group comparisons for the statistically significant variables described above. Compared to the RA with CVD group, the RA alone group had a statistically significant younger age (mean 56 vs. 61), greater proportion of patients who never smoked (51% vs. 37%), lower BMI (median 28.6 vs. 32.2 kg/m2), higher cholesterol (median 182 vs. 168), higher HDL (median 51 vs. 46), higher LDL levels (100 vs. 86) and lower triglyceride levels (100 vs. 125). Both the RA and RA/ CVD groups had a statistically significant greater proportion of women than the CVD group (78% and 75% respectively vs. 52%). Figure 2 presents smoothed empiric distributions of LDL and cholesterol for the 3 groups. These plots better illustrate how cholesterol and LDL levels are higher among the RA only patients.
Figure 2. (A and B) Smoothed densities of Cholesterol and LDL levels by group for patients with a full lipid panel. Red line represents rheumatoid arthritis only group. Green dotted line represents cardiovascular disease only group. Blue dotted line represents rheumatoid arthritis and cardiovascular disease group. A) The distribution of rheumatoid arthritis only patient cholesterol levels peaks at a higher value than the other two groups. B) The distribution of rheumatoid arthritis only patient LDL levels peaks at a higher value than the other two groups.
| Rheumatoid Arthritis vs. Rheumatoid Arthritis and Cardiovascular Disease | Rheumatoid Arthritis vs. Cardiovascular Disease | Rheumatoid Arthritis and Cardiovascular Disease vs. Cardiovascular Disease | |
|---|---|---|---|
| Age at evaluation, years | - | - | - |
| Absolute difference | -5.3 | -3.4 | 1.8 |
| 95% confidence interval | [-7.3, -3.2] | [-4.2, -2.7] | [-0.2, 3.8] |
| P-value | <0.001* | <0.001* | 0.082 |
| Gender | - | - | - |
| P-value | 0.220 | <0.001* | <0.001* |
| Smoking | - | - | - |
| P-value | <0.001* | <0.001* | 0.030 |
| BMI, kg/m2 | - | - | - |
| Multiplicative difference | 0.91 | 0.90 | 1.01 |
| 95% confidence interval | [0.88, 0.94] | [0.89, 0.91] | [0.95, 1.02] |
| P-value | <0.001* | <0.001* | 0.72 |
| Systolic BP, mmHg | - | - | - |
| Multiplicative difference | 0.98 | 1.01 | 1.03 |
| 95% confidence interval | [0.96, 1.00] | [1.00, 1.01] | [1.01, 1.04] |
| P-value | 0.063 | 0.081 | 0.005* |
| Diastolic BP, mmHg | - | - | - |
| Multiplicative difference | 1.02 | 1.04 | 1.01 |
| 95% confidence interval | [1.00, 1.04] | [1.03, 1.04] | [0.99, 1.04] |
| P-value | 0.042* | <0.001* | 0.23 |
| Cholesterol, mg/dL | - | - | - |
| Multiplicative difference | 1.09 | 1.11 | 1.02 |
| 95% confidence interval | [1.04, 1.15] | [1.08, 1.14] | [0.97, 1.06] |
| P-value | <0.001* | <0.001* | 0.73 |
| HDL, mg/dL | - | - | - |
| Multiplicative difference | 1.10 | 1.17 | 1.07 |
| 95% confidence interval | [1.03, 1.16] | [1.14, 1.20] | [1.02, 1.13] |
| P-value | <0.001* | <0.001* | 0.007* |
| LDL, mg/dL | - | - | - |
| Multiplicative difference | 1.19 | 1.16 | 0.98 |
| 95% confidence interval | [1.10, 1.28] | [1.12, 1.20] | [0.91, 1.05] |
| P-value | <0.001* | <0.001* | 0.73 |
| Triglycerides, mg/dL | - | - | - |
| Multiplicative difference | 0.84 | 0.83 | 1.00 |
| 95% confidence interval | [0.75, 0.93] | [0.79, 0.88] | [0.90, 1.10] |
| P-value | <0.001* | <0.001* | >0.99 |
Table 3. Pairwise comparisons of statistically significant variables. *Indicates statistical significance as defined in the methods (p<0.05 for continuous variables, p<0.017 for categorical variables).
There were also concerns if RA patients needed to have positive laboratory values to be included in analyses. Supplemental Table 2 compares patients with and without seropositive status as defined in the methods in both groups of RA patients. Patients with and without seropositive status were similar in terms of all our measured variables. There were no substantial differences in results when analyses were restricted to seropositive status RA patients.
Conclusion
We looked at differences between patients with only RA, only CVD, and both RA and CVD in this study. The patients with only RA had a statistically significant lower mean age than the other two groups. This may be because CVD is more common in older patients, regardless of RA status [2]. It is well documented that a greater proportion of RA patients are female, 1 and as expected, both the RA and RA/CVD groups have a greater proportion of women than the CVD group. The proportion of women in both the RA and RA/CVD groups are similar too, suggesting that among RA patients neither gender is more likely to develop cardiovascular disease. There were a greater proportion of patients with RA and CVD who smoked which is consistent as smoking is a well-known risk factor for increasing CVD. 3. The rheumatoid arthritis only group also had on average a lower BMI than the other two groups as patients with chronic inflammatory disease tend to be thinner and have a lower BMI [14,15].
Arguably the most significant finding in our study is that RA patients have on average higher cholesterol and LDL levels than RA and CVD disease patients. This may be because the RA/CVD and CVD patients are being more aggressively managed due to CVD risk stratification and thus regular checking of cholesterol panels to treat these patients with medications. Our study also found that RA patients have higher HDL and lower triglyceride levels than the RA/CVD and CVD patients, despite thinking that patient with chronic inflammatory disease should have lower HDLs10. Since most cardiovascular disease management prioritizes cholesterol and LDL management over that of HDL and triglyceride levels, HDL and triglyceride levels may remain uncorrected in many RA/CVD and CVD patients. The clinical significance of these results is that RA patients without CVD need to be more aggressively treated to prevent future CVD, as have been noted by many previous studies [16-18].
Attention should also be given to younger patients with RA. For example, most traditional CVD risk assessment tools focus on older patients, such as the popular 10 year Atherosclerotic Cardiovascular Disease Risk Algorithm, which only applies to patients above 40-79 years old [19]. However some studies have found that younger RA patients have a higher relative risk of developing coronary artery disease relative to older patients [20], highlighting the need for an increased awareness of screening for lipid abnormalities in younger RA.
In addition, attention should be given to treating dyslipidemia in RA patients already receiving immunosuppressive therapies. For example, the humanized monoclonal antibody tocilizumab has been shown to increase lipid levels, and the concomitant use of statins has been shown to improve these observed tocilizumab related increases. However, a large proportion of patients receiving tocilizumab are still not treated by statins [21]. In addition to having a lower threshold for screening for lipid abnormalities, practitioners should also have a lower threshold for initiating statin therapy in all RA patients, particularly those of younger age and those on medications such as tocilizumab.
The most important limitation in this study is the dramatic drop in patients who have a full lipid panel available; bias may be introduced from looking at this subset of patients. However, we found similar demographics and vital signs between patients with and without a full lipid panel available. For example, the mean BMI and systolic blood pressure were similar between patients who did and did not have a full lipid panel. We postulate that because BMI and systolic blood pressure are also correlated with lab values such as cholesterol and LDL, it is likely that our estimates of cholesterol, HDL, LDL, and triglycerides are still representative of the general population. Moreover, with a younger patient population the guidelines for tradition lipid treatment and Framingham scores do not apply.
Treating the inflammation in early RA does improve lipid profiles [22]. However, to our knowledge there are no studies placing patients on statin therapy or other cholesterol lowering therapy early in the disease and following these patients long term to see if the cardiovascular disease outcomes improve. Furthermore, in Arthritis Research and Care in 2013, patients given statin therapy early with RA did not achieve LDL goals [23]. Thus, more research needs to be performed to look at statin therapy long term in early RA patients and cardiovascular risk factors. It is evident that pathogenic mechanisms associated with dyslipidemia in RA is not well understood and undertreated [24,25]. In terms of statins being an adjunct therapy to RA, this has been reviewed in few studies with improvement of inflammatory markers, but there are no long term studies confirming this [26,27].
Another drawback is that patient data were only collected from a single academic institution in this study, limiting the generalizability of findings. Future studies should include patients from multiple institutions in various geographic revisions. To verify RA diagnoses in this study, we only looked at RF and CCP serum levels. However, these criteria may have been too restrictive and removed eligible patients from analyses, further reducing sample sizes. Future studies could use patient medication lists, which were not explored in this study, to broaden selection criteria and increase sample sizes. Lastly, there were many challenges dealing with missing data, as many patients had missing lab values and did not have a full lipid profile. This missing data is an inherent characteristic of retrospective observational data obtained from medical records though, as not every patient will have every lab test.
Future research may follow RA patients without CVD over time to see who develops CVD. This would allow physicians to determine which characteristics are more associated with disease progression, and thus those requiring better follow up. Future studies may also see if more aggressive management of cholesterol and LDL levels in RA patients or if different kinds of RA medications (methotrexate vs. biologics) reduce the risk of developing future cardiovascular disease. Finally, work may also compare academic vs. community based practices to see if the findings in this study are applicable in a different medical environment.
In summary, RA patients are at an increased risk of developing CVD, and clinicians need to be more proactive in preventing CVD in patients with rheumatoid arthritis. It is not enough to wait until cardiovascular disease has developed before beginning treatment.
Acknowledgements
The authors would like to thank Bristol Meyers Squib for the grant support and funding this project. The author would also like to support the Division of Rheumatology and Department of Internal Medicine at The Ohio State University Wexner Medical Center for their support.
Conflict of Interest
The authors have no conflicts of interest to state.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
- http://www.cdc.gov/arthritis/basics/rheumatoid.htm
- Crowson CS, Liao KP, Davis JM, et al. Rheumatoid arthritis and cardiovascular disease. Am Heart J. 2013;166(4):622-8.
- Davis JM, Roger VL, Crowson CS, et al. The presentation and outcome of heart failure in patients with rheumatoid arthritis differs from that in the general population. Arthritis Rheum. 2008;58:2603-11.
- Francis ML, Varghese JJ, Mathew JM, et al. Outcomes in patients with rheumatoid arthritis and myocardial infarction. Am J Med. 2010;123:922-8.
- Peters MJ, van Halm VP, Voskuyl AE, et al. Does rheumatoid arthritis equal diabetes mellitus as an independent risk factor for cardiovascular disease? A prospective study. Arthritis Rheum. 2009;61:1571-9.
- Toms TE, Symmons DP, Kitas GD. Dyslipidaemia in rheumatoid arthritis: the role of inflammation, drugs, lifestyle and genetic factors. Curr Vasc Pharmacol. 2010;8:301-26.
- Myasoedova E, Crowson CS, Maradit Kremers H, et al. Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann Rheum Dis. 2010;69:495.
- Peters MJ, Symmons DP, McCarey D, et al. EULAR evidence based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis. 2010;69(2):325-31.
- Yael L, Baron M, Bardakjian S, et al. The role of Rheumatologists vis-à-vis assessment of traditional cardiovascular risk factors in rheumatoid arthritis. Clin Rheumatol. 2014;33(6):769-74.
- Choy E, Sattar N. Interpreting lipid levels in the context of high-grade inflammatory states with a focus on rheumatoid arthritis: a challenge to conventional cardiovascular risk action. Ann Rheum Dis. 2009;68:460-9.
- Baenke F, Peck B, Miess H, et al. Hooked on fat: the role of lipid synthesis in cancer metabolism and tumour development. Dis Model Mech. 2013;6(6):1353-63.
- Daien Cl, Duny Y, Barnetche T, et al. Effect of TNF inhibitors on lipid profile in rheumatoid arthritis: a systemic review with meta-analysis. Ann Rheum Dis. 2012;71:862-8.
- McDonald, John H. Handbook of biological statistics. Baltimore, MD: Sparky House, 2009.
- Bhloe VM, Choi HK, Burns LC, et al. Differences in body mass index among individuals with PsA, psoriasis, RA and the general population. Rheumatology. 2012;51(3):552-6.
- Wesley A, Bengtsson C, Elkan AC, et al. Association between body mass index and anti-citrullinated protein antibody-positive and anti-citrullinated protein antibody-negative rheumatoid arthritis: results from a population-based case-control study. Arthritis Care Res. 2013;65(1):107-12.
- Panoulas VF, Metsios GS, Pace AV, et al. Hypertension in rheumatoid arthritis. Rheumatology. 2008;47(9):1286-98.
- Bartels CM, Kind AJH, Everet C, et al. Low primary lipid screening among medicare patients with rheumatoid arthritis. Arthritis Rheum. 2011;63(5):1221-30.
- Keeling SO, Teo M, Fung D. Lack of cardiovascular risk assessment in inflammatory arthritis and systemic lupus erythematous patients at a tertiary care center. Clin Rheumatol. 2011;30(10):1311-7.
- American College of Cardiology/American Heart Association (2013) Guideline on the assessment of cardiovascular risk.
- Fransen J, Kazemi-Bajestani SMR, Bredie SJH, et al. Rheumatoid arthritis disadvantages younger patients for cardiovascular disease: a meta-analysis. PLoS ONE 2016;11(16):e0157360.
- Soubrier M, Pei J, Durand F. Concomitant use of statins in Tocilizumab-treated patients with rheumatoid arthritis: a post hoc analysis. Rheumatol Ther 2017;4(1):133-49.
- Parveen S, Jacob R, Rajasekhar L, et al. Serum lipid Laterations in early rheumatoid arthritis patients on disease modifying therapy. Indian J Clin Biochem. 2017;32(1):26-32.
- Myasoedova E, Gabriel SE, Green AB, et al. Impact of statin use on lipid levels in statin-naive patients with rheumatoid arthritis versus non-rheumatoid arthritis subjects: results from a population-based study. Arthritis Care Res (Hoboken). 2013;65(10):1592-9.
- Breukelen-van der SDV, Zeben DV, Klop B, et al. Marked underdiagnosis and undertreatment of hypertension and hypercholesterolaemia in rheumatoid arthritis. Rheumatology (Oxford). 2016;55(6):1210-6.
- Tournadre A, Pererira B, Dubos JJ, et al. Management of dyslipidaemia in high-risk patients with recent-onset rheumatoid arthritis: targets still not met despite specific recommendations. Results from the ESPOIR cohort during the first five years of follow up. Clin Exp Rheumatol. 2017;35(2):296-302.
- Das S, Mohanty M, Padhan P. Outcome of rheumatoid arthritis following adjunct statin therapy. Indian J Pharmacol. 2015;47(6):605-9.
- McCarey DW, McInnes IB, Madhok R. Trial of atorvastatin in rheumatoid arthritis (TAR): double-blind randomized placebo-controlled trial. Lancet. 2004;363(9426):2015-21.