Research Article - Journal of Clinical Ophthalmology (2022) Volume 6, Issue 3
Assess the quality and quantity of the lipid layer by interferometry before and after SMILE surgery with the help of OSA and the OSDI questionnaire.
Susmita Banerjee*
Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
- Corresponding Author:
- Dr. Susmita Banerjee Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India; E-mail: mail2susmitabanerjee@gmail.com
Received: 25-Feb-2022, Manuscript No. AACOVS-22-50079; Editor assigned: 28-Feb-2022, PreQC No. AACOVS-22-50079 (PQ); Reviewed: 14-Mar-2022, QC No. AACOVS-22-50079; Revised: 25-Apr-2022, Manuscript No. AACOVS-22-50079 (R); Published: 02-May-2022, DOI: 10.35841/aacovs.6.3.545-549
Citation: Susmita B. Assess the quality and quantity of the lipid layer by interferometry before and after SMILE surgery with the help of OSA and the OSDI questionnaire. J Clin Ophthalmol. 2022;6(3):545-549.
Abstract
The superficial lipid layer is relatively thin, oily layer, around 100 nm in thickness, and is derived from three sources, all of which are in the eyelids. The meibomian gland situated in the upper and lower tarsal plates mainly secretes the lipid layer along with the contributions made by the glands of moll and Zeiss. The lipid layer is important in retarding evaporation of the underlying aqueous layer. The lipid layer comprises polar and non-polar lipids. The primary constituents are mixed wax esters and sterol esters. The makeup around 9% of the total lipid. The remainder consists of free sterols, free fatty acids, hydrocarbons and phospholipids
Keywords
Medical tourism, Surgical site infection, Postoperative complications, Travel medicine, Health tourism.
Introduction
The tear film
The superficial lipid layer is relatively thin, oily layer, around 100 nm in thickness, and is derived from three sources, all of which are in the eyelids. The meibomian gland situated in the upper and lower tarsal plates mainly secretes the lipid layer along with the contributions made by the glands of moll and Zeiss. The lipid layer is important in retarding evaporation of the underlying aqueous layer.
The lipid layer
The lipid layer comprises polar and non-polar lipids. The primary constituents are mixed wax esters and sterol esters. The makeup around 9% of the total lipid. The remainder consists of free sterols, free fatty acids, hydrocarbons and phospholipids [1].
Ocular surface analyser
It is a new instrument of individual analysis which allows a full assessment of the ocular surface through a combination of tests. It allows the research of all three individual layers of the tear film including, lipid, aqueous and mucin, and to identify dry eye disease by determining the affected layer [2].
Lipid layer interferometry
The lipid layer is responsible for coloured fringes seen. The classification of these fringes is divided into six types cited in Guillon and Guillon, 1994.
Small Incision Lenticule Extraction (SMILE)
SMILE is a relatively new refractive procedure designed to treat a multitude of refractive errors. The procedure involves using a femtosecond laser to create a corneal lenticule which is extracted whole through a small incision without the use of an excimer laser [3].
The Ocular Surface Disease Index (OSDI)
The instrument, introduced in 1997 by the Outcomes Research Group, consists of 12 items that assess symptoms, functional limitations, and environmental factors related to dry eye. The questionnaire has 3 subscales: ocular symptoms, vision-related function, and environmental triggers.
Materials and Methods
To assess the quality and quantity of the lipid layer by interferometry before and after SMILE surgery with the help of OSA and the OSDI questionnaire.
As limited data is available of the lipid layer thickness in patients undergoing SMILE surgery assessed by an ocular surface analyser, the present study will provide more information on the lipid layer thickness in patients undergoing SMILE surgery and provide validation with the subjective assessment by OSDI [4].
Main objectives:
- To assess the quality and quantity of the lipid layer by interferometry before and after Small Incision Lenticule Extraction (SMILE) surgery.
Specific objectives:
- To assess lipid layer thickness and type (Interferometry pattern) using OSA
- To measure dryness with the help of the OSDI questionnaire
We assume that the lipid layer is affected by any ocular surface procedure. We hypothesize that the lipid layer may be reduced post SMILE (refractive surgery). However, since the SMILE incision is relatively small and the corneal nerve plexuses are preserved, we believe the effect on the lipid layer is relatively less affected by this form of refractive surgery.
- Study design: Prospective and Longitudinal Study
- Study site: Conducted at Natasha Eye Care and Research Centre, Pune
- Sampling method: Universal sampling
- Sample size: Forty eyes of 20 patients.
- Study population: All healthy myopic and myopic astigmatic patients who are suitable for SMILE surgery.
- Subjects:
Inclusion Criteria
- Patients whose age is more than 18 and less than 40 years
- Patients with myopia or myopic astigmatism
Exclusion Criteria
- Patients whose age is less than 18 or more than 40 years
- Patients who have undergone any ocular surgery
- Any patient who had any uncontrolled systemic disease or disability that affected his or her activities of daily living (including ocular allergy, infection, or irritation that was not related to dry eye disease)
Instruments
- Ocular surface analyser
- Ocular surface disease index questionnaire
Clinical Procedure
- Subjects willing to undergo Refractive surgeries were included in the study. Comprehensive optometric and ophthalmic examinations were performed in all patients. SMILE was performed using the VisuMax femtosecond laser system (Carl Zeiss Meditec).
- OSA was used to assess Interferometry pattern of the lipid layer. This was performed before surgery and 1 week, 1 month after the surgery. Patients were told to fill the Ocular surface disease index questionnaire before the surgery and after 1 month of the surgery.
Data analysis
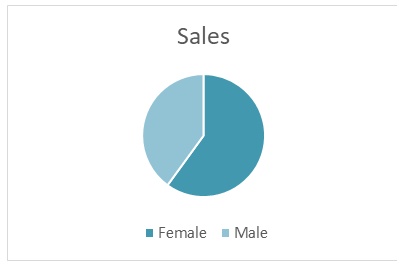
All the data were analysed using primer bio stat software. Shapiro-Wilk normality test, descriptive statistic, repeated measure ANOVA, paired t test was used (Table 1). The significance level was set as 5% throughout the study [5] (Figure 1).
Table 1. The mean age of the patients was 23.85 ± 3.897 ranges from 18 to 31 years. Age is normally distributed as P is greater than 0.05.
| Mean age | P value |
|---|---|
| 23.85 ± 3.87 | 0.252 |
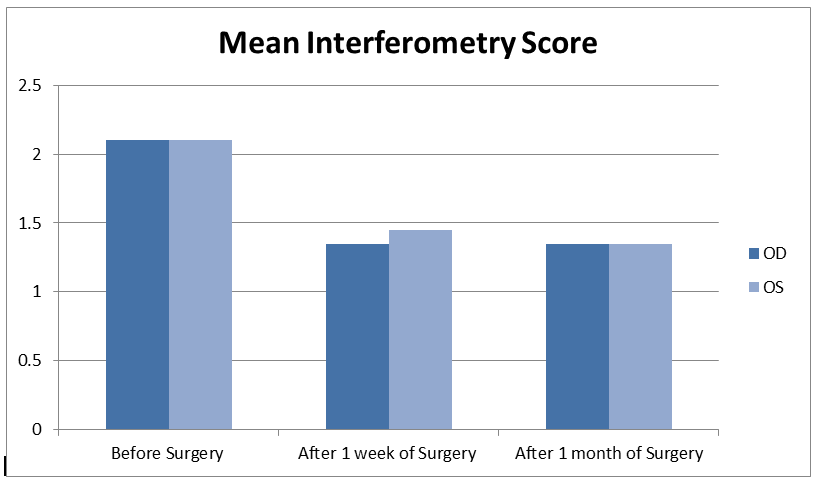
The mean interferometry score for right eye before the surgery was 2.1 ± 0.85, after 1 week of surgery was 1.3 ± 0.587 and after 1 month was 1.3 ± 0.587, which was statistically significant (P=0.00) (Figure 2).
The mean interferometry score for left eye before the surgery was 2.1 ± 0.933, after 1 week of surgery was 1.45 ± 0.75 and after 1 month was 1.3 ± 0.75, which is statistically significant as P is less than 0.05 (P=0.00) (Table 2) and (Table 3).
Table 2. OS and OD mean and value.
| OD Mean | OS Mean | OD P value | OS P value | |
|---|---|---|---|---|
| Before Surgery | 2.1 ± 0.85 | 2.15 ± 0.85 | P=0.00 | P=0.00 |
| After 1 week of Surgery | 1.35 ± 0.587 | 1.45 ± 0.587 | ||
| After 1 month of Surgery | 1.35 ± 0.587 | 1.35 ± 0.587 |
Table 3. Number of patients.
| Lipid Layer Type | Lipid Layer Thickness | Number of Patients | |||||
|---|---|---|---|---|---|---|---|
| Before Surgery | After 1 week | After 1 month | |||||
| OD OS | OD OS | OD OS | |||||
| Not Present | <15 nm | 0 | 0 | 0 | 0 | 0 | 0 |
| Open Meshwork | ~15 nm | 5 | 4 | 14 | 14 | 14 | 15 |
| Close Meshwork | ~30 nm | 10 | 13 | 5 | 4 | 4 | 4 |
| Wave Pattern | ~30 nm-80 nm | 7 | 5 | 2 | 2 | 1 | 1 |
| Amorphous | ~80 nm | 1 | 0 | 0 | 0 | 0 | 0 |
| Colour Fringes | ~80 nm-120 nm | 0 | 1 | 0 | 0 | 0 | 0 |
| Abnormal Colour | ~120 nm-160 nm | 0 | 0 | 0 | 0 | 0 | 0 |
OSDI Score
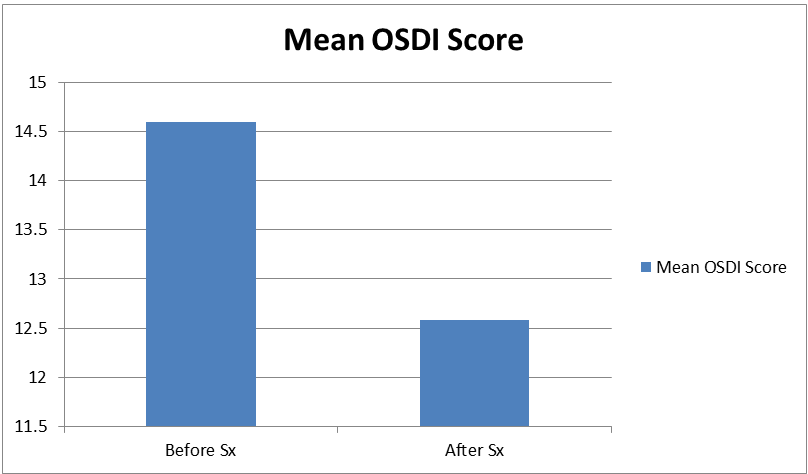
The difference in OSDI Score was not statistically significant as p is greater than 0.05 (Table 4).
Table 4. The mean OSDI Score before the surgery and after the surgery was 14.65 ± 11.35 and 12.58 ± 9.84 respectively (P=0.467)
| Mean | P value | |
|---|---|---|
| OSDI before Surgery | 14.65 ± 11.35 | |
| OSDI after Surgery | 12.58 ± 9.847 | P=0.467 |
Results and Discussion
Dry eye disease continues to be a typical complication of refractive surgery, affecting the ocular comfort of the patients. Prior studies have long-established that the decrease in corneal sensitivity after CRS reduced the tear film stability, thus affecting the health of the ocular surface. However, the role of the LLT in tear film stability after CRS was largely unnoticed. The resistance of the lipid layer to evaporation was reported to rely on its thickness. Therefore, evaluating LLT might facilitate investigate the explanation for tear film instability after CRS. Therefore, we tend to assume that the LLT may play a vital role in tear film stability after CRS, and there is a significant correlation of LLT with alternative signs used for dry eye diagnosis. Although the role of the lipid layer on the tear film is complicated because thickness, distribution, and composition of the lipid layer all contribute to its function, the interaction between LLT and blinking might be an important factor in tear film stability [6].
Dry eye like, corneal sensation reduction is fairly common after refractive surgery. The postulated difference could possibly be that corneal nerves can be cut during flap creation in LASIK, and subsequent excimer ablation further severs stromal nerve fibre bundles, resulting in decreased corneal sensation and increased dry eye symptoms. The SMILE procedure, by contrast, uses a small side cut instead of creating a flap and achieves refractive change by lenticule creation with a femtosecond laser instead of by photoablation with an excimer laser. In this study, we postulate that the lipid layer may be reduced post SMILE surgery. However, since the SMILE incision is relatively small and the corneal nerve plexuses are preserved, we believe the effect on the lipid layer is relatively less affected by this form of refractive surgery.
Evaporative dry eye is the most common form of dry eye syndrome, because of which it important to assess lipid layer before and after the surgery and treat it so that it doesn’t cause discomfort to patients. Although tear breakup time is a clinical test used for evaporative dry eye disease, we used OSA. Because to measure TBUT, fluorescein is instilled into cul-de-sac, which is an invasive method and to avoid infections after surgery we used OSA to measure lipid layer thickness and type which is a non-invasive and safe method. Subjective symptoms are necessary in the diagnosis of dry eye. The various studies used different questionnaires to compare subjective symptoms. The OSDI questions were drawn from three subscales, ocular symptoms, vision-related functions, and environmental triggers. In previous analysis, significant differences in OSDI scores between the SMILE and FS-LASIK groups existed at all-time points. Moreover, OSDI scores in the SMILE group returned to preoperative levels at six months. It thus appears that people in the SMILE groups enjoyed significantly better vision-targeted, health-related quality of life.
In previous studies, OSDI scores increased significantly, indicating more obvious symptoms. Their results additionally showed that DES after CRS chiefly caused discomfort in the eyes and could easily be aggravated by environmental factors such as wind and low humidity. To clarify the role of the LLT in tear film stability and DES, we tend to perform OSDI questionnaire. The sum of the 3 parameters measured in the OSDI score also increased significantly from the preoperative to the postoperative period. The present study demonstrated decrease in OSDI score from 14.65 ± 11.35 to 12.58 ± 9.847 from the preoperative to postoperative period. Possible reason could be that patients were on postoperative medications. This change in LLT and OSDI score can have a great impact on a patients’ overall satisfaction with their surgical and visual outcome and will influence their quality of life [7].
Conclusion
Dry eye is a leading factor in determining patient satisfaction after surgery. As evaporative dry eye is most common form of dry eye syndrome it is necessary to pay attention to prevention and treatment of dry eye, so we evaluate lipid layer thickness and type before the surgery and after the surgery and treat it with medications to improve patient’s satisfaction and overall visual quality. In conclusion, LLT by interferometry using a new instrument OSA showed significant changes. And the OSDI scores decreased and the difference in OSDI score was not statistically significant, which could be because patients were on postoperative medications.
References
- Aymard G, Warot D, Demolis P, et al. Comparative pharmacokinetics and pharmacodynamics of intravenous and oral nefopam in healthy volunteers. J Pharmacol Toxicol. 2003;92:279-286.
[Crossref] [Google Scholar] [Pubmed]
- Ahmad M, Yaqoob M, Murtaza G, et al. Study of pharmacokinetics and comparative bioavailability of nefopam 30 mg tablets in twelve fasting healthy pakistani male young subjects: Single-dose, randomized, two-period,two-treatment and two-way cross-over design. Med Princ Pract. 2012;21:271-276.
[Crossref] [Google Scholar] [Pubmed]
- Seetohul LN, Paoli GD, Drummond G, et al. Nefopam hydrochloride: A fatal overdose. J Anal Toxicol. 2015;39:486-489.
[Crossref] [Google Scholar] [Pubmed]
- Huart ED, Vigneron J, Clarot I, et al. Physicochemical stability of nefopam and nefopam/droperidol solutions in polypropylene syringes for intensive care units. Eur J Hosp Pharm 2020;27:e69-e73.
[Crossref] [Google Scholar] [Pubmed]
- Shama SA, Amin AS. Spectrophotometric microdetermination of nefopam, mebevrine and phenylpropanolamine hydrochloride in pharmaceutical formulations using alizarins. Spectrochimica Acta Part A Mol Biomol Spect. 2004;60:1769-1774.
[Crossref] [Google Scholar] [Pubmed]
- Fatema K, Rahman MDZ, Biswas SK, et al. Development of UV spectroscopic method for nefopam and escitalopram as inn drugs in tablet dosage form. Stamford J Pharma Sci. 2010;3(1):4-10.
- Tracqui A, Berthelon L, Ludes B, et al. Fatal overdosage with nefopam (acupan). J Anal Toxicol 2002;26:239-243.
[Crossref] [Google Scholar] [Pubmed]