Review Article - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 1
A review of current low vision services in Alberta
Andrew Swift1*, Yejun Hong1, Colleen Schreiber2, Micah Luong3, Samuel N Markowitz4
1Cumming School of Medicine, University of Calgary, Calgary, Canada
2Rockyview General Hospital Eye Clinic, Calgary, Canada
3Section of Ophthalmology, Department of Surgery, University of Calgary, Calgary, Canada
4Low Vision Rehabilitation Fellowship Director, Ophthalmology and Vision Sciences, University of Toronto, Toronto, Ontario, Canada
- Corresponding Author:
- Dr. Andrew Swift
University of Calgary Cumming School of Medicine
Calgary AB
Canada
E-mail: andrew.swift@ucalgary.ca
Accepted date: 13 January, 2021
Citation: Swift A, Hong Y, Schreiber C, et al. A review of current low vision services in Alberta. J Clin Ophthalmol 2021;5(1):341-346.
Abstract
Purpose: To provide a thorough review of the current low vision services in the province of Alberta Canada and offer evidence-based suggestions on ways these services can be improved. It is hoped that such an overview will facilitate discussions that will ultimately result in more equitable and comprehensive services, not only within the province of Alberta, but nationally and international as well.
Methods: Information gathered for this article was obtained from organizations such as Vision Loss Rehabilitation Canada, health care professionals providing low vision services within Alberta, the Sight Enhancement Clinic in Calgary and Alberta Education. Suggestions for improving low vision services are based on a proposed tiered model for integrated low vision services in Canada.
Results: Several ways in which in which low vision services can be improved were identified within the province. These include improvement of referral practices to low vision services, unifying voices to advocate for funding, simplifying access to provincially funded subsidization for low vision devices and increasing multidisciplinary efforts between health care professionals.
Conclusions: While Alberta already provides high quality low vision services through the tireless efforts of many individuals and organizations, on-going work is needed to improve accessibility, eliminate barriers and to ensure equity of low vision care within the province.
Keywords
Low vision, Low vision rehabilitation, Low vision devices, Low vision services (LVS).
Introduction
According to the American Academy of Ophthalmology’s Preferred Practice Patterns for Vision Rehabilitation, Low Vision (LV) is defined as a visual impairment in which visual acuity is less than or equal to 20/50 in the better-seeing eye and cannot be improved with regular eyeglasses, contact lenses, medicine, or surgery [1]. LV may result from other uncorrectable factors such as loss of visual field, reduced contrast sensitivity, increased glare, or difficulty with activities of daily living (ADLs) caused by vision, even if the visual acuity is better than 20/50 [1]. LV can have many causes including ocular disease and neurological disorders. Vision impairment reduces quality of life, increases the risk of death and affects economic and educational activities [2]. In Canada, the national rate of visual impairment in 2018 was estimated at 5.7%, with lower rates in Manitoba, Quebec, and Ontario (2.4%-3.5%), and higher rates in Nova Scotia, Alberta, British Columbia, and Newfoundland and Labrador (6.9%-10.9%) [3].
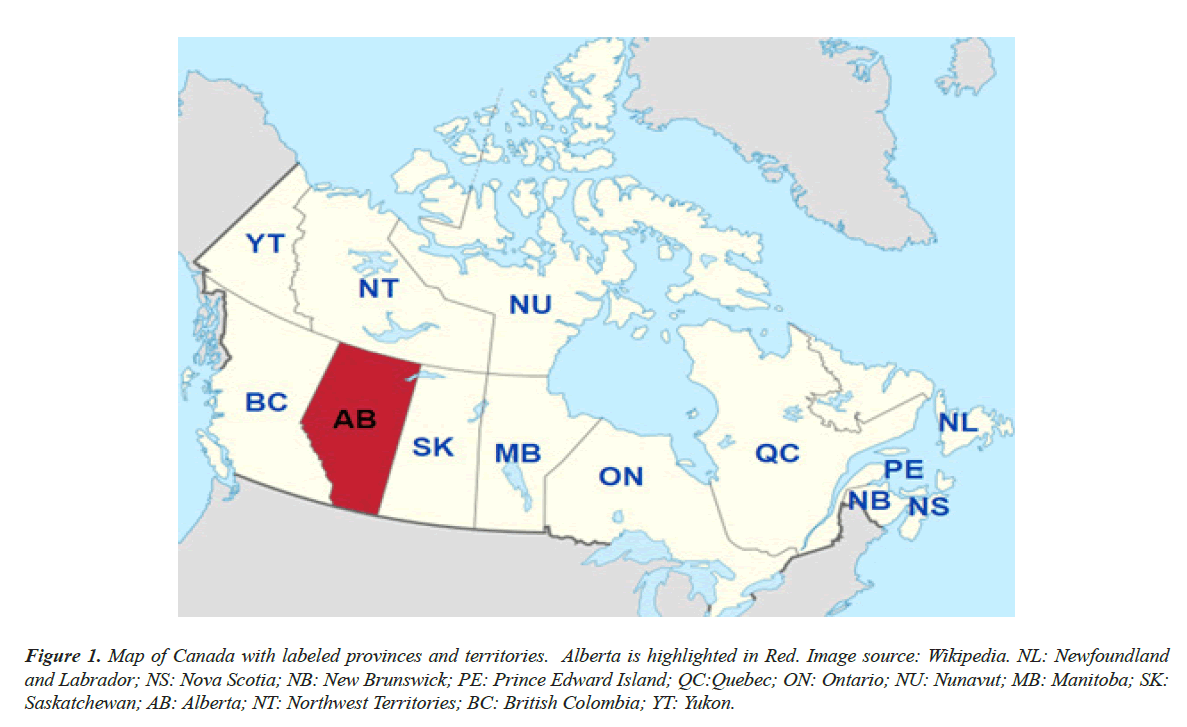
Under the Canadian Health Act, each province and territory in Canada is responsible for the delivery of health care within its jurisdiction [4]. As such, low vision services (LVS) are quite variable across Canada ranging from full provincial subsidization, Quebec being the most comprehensive, to no provincial subsidization whatsoever. In this article we will focus on the province of Alberta, one of Canada’s 13 provinces and territories located in the western portion of the country (Figure 1). In 2006, Harper et al. predicted that over the course of the next two decades the number of Albertans over the age of 40 living with age-related blindness or visual impairment would increase by 113% [5]. As the number of LV patients continues to increase in Alberta, a thorough review of current LVS in the province is a needed step towards ensuring adequate and equitable services are being provided. It is also hoped that a concise overview of LVS in Alberta will serve to facilitate discussion and reviews of models for providing LVS across Canada and internationally as well.
Figure 1: Map of Canada with labeled provinces and territories. Alberta is highlighted in Red. Image source: Wikipedia. NL: Newfoundland and Labrador; NS: Nova Scotia; NB: New Brunswick; PE: Prince Edward Island; QC:Quebec; ON: Ontario; NU: Nunavut; MB: Manitoba; SK: Saskatchewan; AB: Alberta; NT: Northwest Territories; BC: British Colombia; YT: Yukon.
Literature Review
Current status of Low Vision Services in Alberta
A not-for-profit charitable organization called the Canadian National Institute for the Blind (CNIB) has been assisting those with LV and blindness in Canada since 1918. In 2017, Vision Loss Rehabilitation Canada (VLRC) emerged from the CNIB to provide regional organizations and services that are able receive provincial funding and support to run its programs. Apart from Quebec, which uses its own internally administered organizations, all other provinces provide funding to the VLRC to administer LVS within their jurisdiction. Thus, Vision Loss Rehabilitation Alberta (VLRA) is currently the main provider of LVS within the province. At present, the most significant issue facing Alberta’s access to LVS is limited funding. In the provinces that utilize VLRC, Alberta invests less per capita than any other province in Canada (Table 1). While Alberta has more access to optometrists than any other province (20 optometrists available per 100,000 people) and is generally on par with other provinces for access to ophthalmologists (2.7 ophthalmologists per 100,000 people), it has the lowest number of Vision Loss Rehabilitation (VLR) specialists per capita (0.2 VLR specialists per 100,000 people) (Table 2).
| Province | Provincial sector per capita health spending ($ billion) | Total provincial health spending ($ billion) | VLRC government revenue per capita | Relative per capita: VLRC per capita/$1,000 per capita provincial health expenditure | $100,000 VLRC revenue per billion health spending |
|---|---|---|---|---|---|
| BC | $4,259 | $21.5 | $1.02 | $0.24 | $2.26 |
| AB | $5,187 | $20.6 | $0.41 | $0.08 | $0.87 |
| SK | $4,804 | $5.9 | $1.47 | $0.31 | $2.73 |
| MB | $4,787 | $6.7 | $1.43 | $0.30 | $2.74 |
| ON | $4,385 | 63.5 | $0.99 | $0.23 | $2.10 |
| QC | $4,343 | 38.5 | nil | - | - |
| NB | $4,691 | 2.9 | $1.76 | $0.38 | $4.54 |
| NS | $4,846 | 4.6 | $1.04 | $0.21 | $2.09 |
| PE | $5,160 | 0.7 | $1.75 | $0.34 | $3.57 |
| NL | $6,010 | 3 | $1.94 | $0.32 | $3.37 |
Table 1: Comparison of general provincial healthcare spending (CAD) and Vision Loss Rehabilitation Canada (VLRC) funding between provinces. Quebec is the exception as the majority of visual rehabilitation services are provided by government- sponsored rehabilitation centres like the Centres de réadaptation en déficience physique rather than through VLRC (Data from Canadian Institute for Health, 2019). NL: Newfoundland and Labrador; NS: Nova Scotia; NB: New Brunswick; PE: Prince Edward Island; QC: Quebec; ON: Ontario; MB: Manitoba; SK: Saskatchewan; AB: Alberta; BC: British Colombia.
| Prov. | # Ophthalmologists per 100,000 population | # Optometrists per 100,000 population | # VLR specialists per 100,000 population |
|---|---|---|---|
| BC | 4.2 | 17 | 0.3 |
| AB | 2.7 | 20 | 0.2 |
| SK | 2.6 | 14 | 0.5 |
| MB | 2.4 | 14 | 0.5 |
| ON | 3.1 | 18 | 0.7 |
| QC | 4.3 | 18 | - |
| NB | 3.7 | 16 | 0.9 |
| NS | 4.5 | 15 | 0.6 |
| PE | 3.5 | 14 | 1.4 |
| NL | 2.9 | 12 | 1 |
| Canada (excl. QC) | 3.4 | 17 | 0.4 |
Table 2: Comparison of the number of ophthalmologists, optometrists and Vision Loss Rehabilitation (VLR) specialists per 100,000 people in each province (Data from Canadian Medical Association Masterfile, 2018). NL: Newfoundland and Labrador; NS: Nova Scotia; NB: New Brunswick; PE: Prince Edward Island; QC: Quebec; ON: Ontario; MB: Manitoba; SK: Saskatchewan; AB: Alberta; BC: British Colombia.
VLRA currently has two assessment centres located in Calgary and Edmonton. Four other VLRA centres in the province have recently closed due to lack of funding. As with other provinces in Canada, a widespread client distribution and limited service locations can be a major impediment in access to LVS [6,7]. To increase accessibility and depending on the demand and time of year, VLRA specialists will travel to rural areas. For those dealing with the stress and grief associated with vision loss, the VLRA centre in Calgary offers specialized clinical counselling. This is an important service as depression, social isolation and increased risk of suicide are directly correlated with vision loss in older adults [5,8].
Like several other provinces in Canada, Alberta has a provincial assistance program for LV devices. This program is called the CNIB Specialized Technical Equipment Program (STEP). STEP is a cost-sharing program that covers 75% to100% of the device cost depending on the patient’s income level. Patient’s with a best-corrected visual acuity (BCVA) of ≤ 20/70 in both eyes qualify for more simple LV devices like magnifiers, while those with a BCVA of ≤ 20/200 qualify for more complex devices like closed-circuit television (CCTV). STEP is a much-needed service as cost and reduced income level can be prohibitive factors to obtaining devices for those using LVS across Canada [7]. The only organizations allowed to access STEP funding are VLRA, which performs the assessment, and the CNIB foundation, which issues the devices.
The Sight Enhancement Clinic (SEC) at Calgary’s Rockyview General Hospital (RGH) continues to have a close working relationship with VLRA and CNIB. The SEC is a specialized LV clinic that focuses on the patient’s remaining vision and seeks to enhance quality of life through counselling and LV devices. The SEC clinic sees approximately 350 patients per year experiencing vision loss, (typically range of 20/50 to 20/200) or has a reduced field of vision. Consistent with Harper et al. predictions SEC has seen a 100% increase in referrals since 2006 [5]. Appointments at the SEC are often a one-time visit and are typically two hours to allow for adequate assessment and education. The SEC team consists of an optometrist (prescribes and recommends appropriate optical devices) and a LV technician/counsellor (education, LV device training and referrals for vision rehabilitation and other community resources). Patients have the option to fill prescriptions for optical and LV devices; however there is no access to STEP funding if purchasing LV devices through the SEC. This preliminary introduction to LV devices at the SEC prepares patients for their appointment with the VLRA and increases the likelihood of success in their rehabilitation process [9]. Collaboration between SEC and VLRA allows access to LVS from a health region entry point or community entry point. This is important as patients may prefer to access LVS in a hospital over a community setting due to perceived stigma associated with their visual impairment or a misunderstanding regarding the services provided by LVRA and the CNIB [7].
For the past 6 years, the LV clinic at the Royal Alexandra Hospital (RAH) in Edmonton has not provided services. Prior to its closing, the clinic performed eye exams and LV assessments every second week with a trained optician available on-site for consultation and equipment sales [5]. The clinic was a partnership between the CNIB, who handled referrals and bookings, and the Department of Ophthalmology at the RAH. Currently there are efforts being made to establish a team model of care at the RAH clinic with an ophthalmologist as lead. In the meantime, LV patients in the Edmonton area are assessed by LVRA or a small number of local optometrists who provide LVS.
Since 2007 pediatric LV patients in Alberta have benefited from the development of several major collaborative efforts. The Southern Alberta Vision Interagency Meeting is held biannually in Calgary, coordinated and led by the provincial government. These meetings provide a forum where LV professionals can share information and coordinate services. A Travelling Low Vision Clinic (TLVC) was started in 2009 and represents collaboration between the Alberta Children's Hospital Foundation, Alberta Education, CNIB foundation and Alberta Health Services. This clinic was designed to provide comprehensive and equitable LVS for children and youth throughout Alberta. Every year there are 7-8 clinics held throughout the province. The interdisciplinary clinic team includes ophthalmology, optometry, Teachers of Students with Visual Impairments (TVIs), Orientation and Mobility (O&M) specialists and representatives from the CNIB trained in pediatric LV care. Appointments can be booked online (https://vision.alberta.ca/homepage/tlvc/). The TLVC has a library of low-tech devices that patients can trial at their appointment and keep if it provides benefit. Funding for these devices is provided exclusively by Alberta Education.
Discussion
Improving LVS in Alberta
As the demand for LVS continues to increase in Alberta, there is an ongoing need for streamlining services, removing potential barriers and expanding services to provide more equitable care throughout the province. In 2016, Leat proposed a tiered model for integrated LVS in Canada adapted from the WHO’s recommended model [10]. The model includes three levels of As the demand for LVS continues to increase in Alberta, there is an ongoing need for streamlining services, removing potential barriers and expanding services to provide more equitable care throughout the province. In 2016, Leat proposed a tiered model for integrated LVS in Canada adapted from the WHO’s recommended model [10]. The model includes three levels of care which include, Level 1: Screening and recognition followed by appropriate triage; Level 2: Management of patients with minimum visual impairment; Level 3: Comprehensive LVS for patients with more severe LV and greater disabilities. The following are several suggestions to improve LV services within Alberta based on Leat’s proposed model:
Improvement of referral practices to LVS
Improving referral practices is needed to improve all three levels of care in Alberta. Currently VLRA has the second lowest rate of referrals from ophthalmologists and the third lowest rate from optometrists compared to the rest of the provinces (Table 3). This trend reflects a need for improved communication and collaboration between VLRA and eyecare professionals in Alberta. In the Montreal Barriers study, Over bury and Wittich found a significant relationship between a patient’s awareness of LVS and their level of visual acuity, as doctors often waited to initiate referrals until vision had declined significantly [11]. They also found that ophthalmologists, who refer their patients to LVS regularly, tend to refer earlier in the disease process. It is not uncommon for patients who attend the SEC, for example, to express that they did not realize there were so many services and aids for people with LV and wished their doctor would have referred them sooner. Early intervention is important so that patients can receive the appropriate counselling and rehabilitation before they experience depression, give up on ADLs, or abandon other enjoyments [10,12]. Thus, increased education and promotion aimed at eyecare providers regarding the nature of LVS and the ideal time for referral is needed in Alberta.
| Prov. | Population | # of licenced ophthas | # of ophthas who referred to VLRC (2018) | % of ophthas referring | # of licensed optoms | # of optoms referring to VLRC (2018) | % of optoms referring |
|---|---|---|---|---|---|---|---|
| BC | 47,48,000 | 199 | 149 | 75% | 785 | 125 | 16% |
| AB | 40,67,000 | 109 | 76 | 70% | 794 | 176 | 22% |
| SK | 10,98,000 | 28 | 28 | 100% | 182 | 60 | 33% |
| MB | 12,78,000 | 31 | 31 | 100% | 177 | 79 | 45% |
| ON | 1,34,48,000 | 423 | 349 | 83% | 2424 | 550 | 23% |
| QC | 81,64,000 | 351 | - | - | 1,510 | - | - |
| NB | 7,47,000 | 28 | 19 | 68% | 122 | 26 | 21% |
| NS | 9,24,000 | 42 | 33 | 79% | 138 | 33 | 24% |
| PE | 1,43,000 | 5 | 5 | 100% | 21 | 8 | 38% |
| NL | 5,20,000 | 15 | 14 | 93% | 62 | 15 | 24% |
| Total Canada (excludes Territories) | 3,51,37,000 | 1231 | 704 | 80% | 6215 | 1072 | 23% |
Table 3: Comparison of the number of referrals to VLRC to the number of licenced ophthalmologists and optometrists by province in 2018. Ophthas: ophthalmologists; Optoms: optometrists (Data from Canadian Medical Association Masterfile, 2018). NL: Newfoundland and Labrador; NS: Nova Scotia; NB: New Brunswick; PE: Prince Edward Island; QC: Quebec; ON: Ontario; MB: Manitoba; SK: Saskatchewan; AB: Alberta; BC: British Colombia.
Unifying voices to advocate for funding
Increased funding to LVS in Alberta is especially needed for levels 2 and 3 of care. Currently Albertans enjoy robust coverage for screening depending on age as yearly comprehensive examinations with an optometrist are completely covered by the provincial health care plan for those under 19 years of age and 65 years or older. In levels 2 and 3 of care, comparatively low provincial funding of LVS has resulted in the lowest number of VLR specialists per capita (Table 2) and necessitated the closure of 4 out of the 6 provincial VLRA centres in 2019. It is particularly difficult to recruit and retain LVR specialists in Alberta as there is only one training program in Canada, located far away in Quebec, and because LVR specialists are paid more in other provinces. Additionally, fewer VLRA centres presents a unique challenge to those with LV as transportation and cost can be barriers to accessing LVS [7]. A major barrier faced by health care professionals providing care at levels 2 and 3 is the relatively low remuneration and the additional equipment costs associated with providing LV examinations [13,14]. These were factors in the disappearance of the LV clinic at the RAH in Edmonton and the reasons why few optometrists in the province provide LVS. Interestingly, Alberta currently has provincial LV billing codes for optometry but not for ophthalmology. For an optometrist to be reimbursed by the province for a LV examination requires they prove that they have a minimum set of more specialized LV equipment and devices. Even with access to billing for LV exams, an optometrist in Edmonton providing LVS reports that profitability is low due to gaps in provincial coverage for patients between the ages of 19-64, additional costs associated with LV examination equipment, and difficulty selling LV devices for a profit as the CNIB and VLRA control the government subsidy for devices. For these reasons, their office only offers LV exams once a week and the current waitlist is several months long. With a widespread distribution of patients over a large geographical area in Alberta, increased funding and remuneration to incentivize more communitybased delivery of level 2 care would dramatically improve accessibility and equity across the province. Additional funding would also allow the SEC clinic to maintain and update their aging equipment and expand the library of LV devices available for patients to trial prior to their LV rehabilitation appointment. Thus, engaging provincial leaders of government in a unified voice with Alberta Health Services, VLRC members, healthcare professionals and others involved in LVS is needed to bring increased awareness to the current funding gaps.
Simplifying Access to STEP Subsidization for low Vision devices
Simplifying access to provincially subsidized LV devices would improve levels 2 and 3 of care in Alberta. The current contract to administer STEP funding for subsidized LV devices in Alberta rests exclusively with CNIB and VLRA. While these organizations have done much to further the work of LVS in the province, having STEP funding exclusive to these groups may create barriers for some patients seeking aid. Cost, income level, comorbidities, location and transportation are all known factors that can prevent access to LV care [7]. A possible solution to minimize duplicate appointments, increase accessibility and streamline the process would be to allow centres like the SEC, or community eyecare providers, limited access to STEP funding for more simple LV devices. This is also important as individuals are more likely to utilize LVS and devices when provided at the same location where other ophthalmic services are provided [15].
Increasing unification and multidisciplinary efforts
Increasing multidisciplinary efforts is important at all levels of care, particularly at the third level. Multidisciplinary rehabilitation is currently recognized as the ideal means of delivering LVR [10]. In Alberta, when the VLRA is separate from ophthalmology and optometry neither provides the most optimum and efficient care while often duplicating recommendations and assessments [16]. Models of LVS delivery where ophthalmologists, optometrists, opticians, occupational therapists, rehabilitation teachers, and instructors work together in one clinic are currently available in the provinces of Quebec and Ontario, as well as the United States and Europe [10,16]. Multidisciplinary centres (MDCs) facilitate ongoing relationships with patients and increase the range of services provided [10]. While multidisciplinary models of care are currently benefiting the pediatric population in Alberta through th TLVC and the Southern Alberta Vision Interagency Meetings, LVS for adults in the province would benefit greatly from a more unified approach. Currently the SEC in Calgary is the only centre in the province providing LVS to adults that could be described as an MDC. The team at the SEC is limited to optometry and LV technicians/counsellors.
The addition of an occupational therapist (OT) was trialed a few years ago at the SEC with great success but has since been discontinued due to funding cuts. Incorporating experienced OTs into MDCs like the SEC would help patients become more confident and proficient users of LV technology while increasing their ability to secure or maintain employment and other ADLs. To address a higher prevalence of depression and other mental health problems among adults with vision impairment, the addition of specialized psychologists and social workers would also provide great benefit [12,17,18]. While the VLRA centre in Calgary has access to one social worker trained in counselling (who is on maternity leave at the time of writing this paper) they no longer have a psychologist due to funding cuts. As a result, many LV patients who need counselling are referred by VLRA and SEC to services like the Calgary Counselling Center and the Alberta Health Link for counselling support. While these are great resources, they are not specifically trained in the unique challenges associated with vision loss.
Of note, there is a major collaborative effort currently underway in Alberta that is seeking to develop clinical pathways and system-wide strategies for neurological vision loss due to stroke and other causes. A multidisciplinary group, involving the SEC, optometry, neurology, ophthalmology, neuro-ophthalmology, OT, VLR specialists and others, is working together to improve VLR outcomes. So far, the SEC has been successfully fitting Fresnel prisms and promoting eye-search scanning therapy to improve quality of life of patients with hemianopias.
Conclusion
Alberta continues to provide high quality LVS through the tireless efforts of individuals combined with the many systems and organizations already in place. While important progress has been made, ongoing work is needed to ensure LVS continues to expand and be more accessible for Albertans with vision loss. Improvement of referral practices to LVS, unifying voices to advocate for funding, simplifying access to STEP funding and devices and increasing multidisciplinary efforts are some of the ways LVS can be improved in the province.
Acknowledgements
We thank Rachel Kobelt (Manager VLRA) for providing comments and reviewing the document to ensure accuracy. We also acknowledge Matthew Kay (Executive Director VLRA) and Li Liu (LV specialist with VLRA) for their contributions.
Declarations of competing interests
None of the authors has any competing interests, financial or otherwise.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for -profit sectors.
References
- Fontenot JL, Bona MD, Kaleem MA, et al. Vision Rehabilitation Preferred Practice Pattern®. Ophthalmology. 2018;125:228-78.
- Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:888-97.
- Aljied R, Aubin M-J, Buhrmann R, et al. Prevalence and determinants of visual impairment in Canada: cross-sectional data from the Canadian Longitudinal Study on Aging. Can J Ophthalmol. 2018;53:291-7.
- Government of Canada. Canada Health Act, 2020.
- Harper K, McFee C, Macdonald I, et al. Low vision service models in Alberta: Innovation, collaboration, and future opportunities. Can J Ophthalmol. 2006;41:373-7.
- Basilious A, Basilious A, Mao A, et al. Trends in low vision care provided by ophthalmologists in Ontario between 2009 and 2015. Can J Ophthalmol. 2019;54:229-36.
- Lam N, Leat SJ. Barriers to accessing low-vision care: the patient’s perspective. Can J Ophthalmol. 2013;48:458-62.
- Hinds A, Sinclair A, Park J. Impact of an interdisciplinary low vision service on the quality of life of low vision patients. Br J Ophthalmol. 2003;87:1391-6.
- Siemsen W, Bergstrom A, Hathaway J. Efficacy of a low vision patient consultation. Journal of Visual Impairment & Blindness 2005;99:426-30.
- Leat SJ. A Proposed Model for Integrated Low-Vision Rehabilitation Services in Canada. Optom Vis Sci. 2016;93:77-84.
- Overbury O, Wittich W. Barriers to Low Vision Rehabilitation: The Montreal Barriers Study. Invest Ophthalmol Vis Sci. 2011;52:8933-8.
- Holloway E, Sturrock B, Lamoureux E, et al. Can we address depression in vision rehabilitation settings? Professionals’ perspectives on the barriers to integrating problem-solving treatment. Disabil Rehabil. 2018;40:287-95.
- Malkin AG, Ross NC, Chan TL, et al. U,S. Optometrists' Reported Practices and Perceived Barriers for Low Vision Care for Mild Visual Loss. Optom Vis Sci. 2020;97:45-51.
- Wittich W, Canuto A, Overbury O. Overcoming barriers to low-vision rehabilitation services: Improving the continuum of care. Can J Ophthalmol. 2013;48:463-7.
- Goldstein JE, Guo X, Boland MV, et al. Low Vision Care – Out of Site. Out of Mind. Ophthalmic Epidemiology. 2020;27:252-8.
- Lam N, Leat SJ, Leung A. Low-vision service provision by optometrists: A Canadian nationwide survey. Optometry and Vision Science. 2015;92:365-74.
- Margrain TH, Ryan B, Wild JM. A revolution in Welsh low vision service provision. Br J Ophthalmol. 2005;89:933-4.
- Sabel BA, Wang J, Cardenas-Morales L, et al. Mental stress as consequence and cause of vision loss: the dawn of psychosomatic ophthalmology for preventive and personalized medicine. EPMA J. 2018;9:133-60.