Mini Review - Journal of Clinical Ophthalmology (2023) Volume 7, Issue 2
A novel dichoptic home treatment for amblyopia
Oren Yehezkel*, Tamara Wygnanski Jaffe, Michelle Dalton
Department of Ophthalmology, Bar-Ilan University, Ramat Gan, Tel Aviv, Israel
- Corresponding Author:
- Oren Yehezkel
Department of Ophthalmology,
Bar-Ilan University,
Ramat Gan Tel Aviv Israel
E-mail: oren.yehezkel@gmail.com
Received: 26-Dec-2022, Manuscript No. AACOVS-23-84658; Editor assigned: 28-Dec-2022, AACOVS-23-84658 (PQ); Reviewed: 11-Jan-2023, QC No. AACOVS-23-84658; Revised: 10-Mar-2023, Manuscript No. AACOVS-23-84658 (R); Published: 17-Mar-2023, DOI:10.35841/aacovs.7.2.634-636
Citation: Yehezkel O, Jaffe TW, Dalton M. A novel dichoptic home treatment for amblyopia. J Clin Ophthalmol. 2023;7(2): 634-636.
Abstract
Patching for the treatment of amblyopia is the current “gold standard” but a new clinical study suggests that using a binocular eye tracking based home treatment system may be as efficacious in appropriate cases. In “an eye tracking based dichoptic home treatment for amblyopia: A multicenter randomized clinical trial” authors Wygnanski-Jaffe, et al. compared NovaSight’s novel CureSight system with traditional patching in children between the ages of 4>9 years who had been diagnosed with anisometropic, small angle strabismic or mixed mechanism amblyopia. The device was an investigational device when this study was performed and received an FDA clearance based on the outcomes of this study (K221375, September 29, 2022).
Keywords
Anisometropic, Investigational, Gold standard, NovaSight’s novel, CureSight system
Introduction
Patching has several us limitations, including poor adherence, residual amblyopia and amblyopia recurrence that affects almost 25% of patients [1-3]. Clinicians treating this disease are likely familiar with binocular amblyopia therapy with dichoptic presentation in an attempt to overcome some of the limitations with patching as well as to improve visual outcomes [4-6].
In general, binocular treatments adjust the visual stimuli between the amblyopic and non-amblyopic eye, which in turn reduces interocular suppression [7-13]. To date, dichoptic therapy has met with mixed results in various randomized controlled trials and had yet to be found either noninferior or superior when compared to patching therapy. In this study, 103 children (50% female) were randomized 1:1 to either the CureSight system or patching for 16 weeks, beginning in August 2020 and with the last child exiting the study in February 2022 [14-19].
The CureSight system allows children to watch licensed streamed video content to achieve its treatment goals. According to the authors, the treatment algorithm “blurs the central vision of the nonamblyopic (dominant eye in real time using continuous gaze tracking and is less obtrusive than conventional patching.” The developers programmed the device to work on virtually any content available on the internet so that the child’s home treatment is as enjoyable as possible (there are exceptions for parental control, etc.). The device incorporates eye gaze tracking and separation of streamed visual stimuli presented on a monitor into two separate digital channels, one for each eye. There are four main components to the device: A computer/monitor for stimulus presentation, an eye tracker, anaglyph glasses worn over the child’s glasses during the treatment time to separate stimuli presented to each eye and proprietary software that uses the data to blur the central vision area (details on the device are available in the published paper). It is important to note that since the time of the study, the device has received US food and drug administration clearance and is currently marketed in the US and Italy.
Literature Review
Children in the CureSight treatment group (“treatment”) were expected to watch a video for 90 minutes per day, 5 days a week for 16 weeks (120 hours total). A positioning algorithm automatically guided the child to sit at a viewing distance of ~60 cm, deemed the optimal distance for optimal treatment); then a brief eye tracking calibration was performed and the child could begin with the treatment session. Children in the patching group (“control”) wore an adhesive patch (Ortopad- Pietrasanta pharma, Italy) over the dominant eye for 2 hours per day, 7 days per week for 16 weeks (for a total of 224 hours). The primary outcome was the mean improvement from baseline Visual Acuity (VA) to 16 weeks in the amblyopic eye, allowing a noninferiority of no more than one logMAR line.
Monocular and binocular distance VA testing was performed based on the child’s age, with younger children (4 to <7 years) were assessed by the HOTV protocol using the Lea symbols optotype, while the older children (7 to <9 years) were assessed with the electronic early treatment for diabetic retinopathy study protocol using the lea numbers optotype. Children remained in their initial assessment group regardless of age during the follow-up periods. Secondary and additional outcomes included the change from baseline to week 16 in the stereoacuity test score, the amblyopic eye Near VA (NVA), the binocular VA and the binocular NVA. Adverse Events (AEs) were assessed via questionnaires for both parents and participants including symptoms pertaining to diplopia, headaches and eyestrain.
Results
There were no statistically significant differences between the two groups at baseline, including age, gender and patching history. The overwhelming majority of children were diagnosed with anisometropic amblyopia (92%).
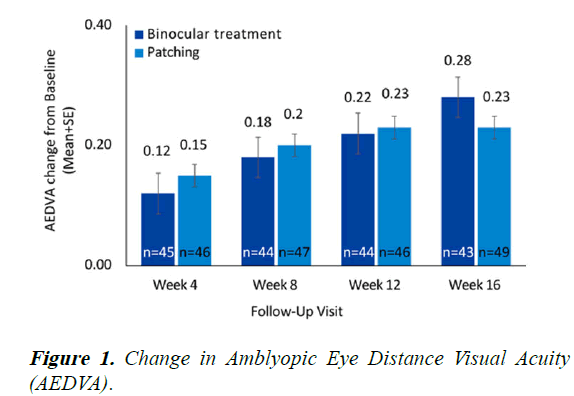
At baseline, the mean ± SD amblyopic eye VAs in the binocular and patching treatment groups were 0.37 ± 0.15 logMAR and 0.37 ± 0.14 logMAR, respectively. There was a statistically significant improvement in the amblyopic eye VA from baseline at weeks 4, 8, 12, and 16 in both treatment groups (P<0.001). The mean ± SD improvement from baseline at 16 weeks was 0.28 ± 0.13 logMAR in the binocular treatment group (P<0.0001) and 0.23 ± 0.14 logMAR in the patching group (P<0.0001) (Figure 1). The difference between groups in LSmean improvement from baseline at 16 weeks was smaller than 0.1 logMAR that was defined as the success criterion of non-inferiority in relation to controls 0.034 logMAR (90% CI (-0.008, 0.076)), indicating that binocular treatment is noninferior to the “gold standard” patching treatment. Moreover, there were no significant differences in the improvement in amblyopic eye VA when subdivided by the covariates of the age group (younger or older than 7 years, with an even distribution), the type of amblyopia (refractive, strabismic or combined), previous amblyopia treatment (none, patching, atropine, patching and binocular treatment) or the baseline VA levels (<0.3, 0.3 to 0.5, >0.5 logMAR). At 16 weeks, the proportion of children with an improvement from baseline of amblyopic eye VA of 2 lines or more was 79% in the binocular treatment group and 61% in the patching group, with no significant difference between the 2 groups difference of 17.9% 95% CI (-0.43%, 36.1%); chi-square test P=0.06.
Change in ADEVA from the baseline at each follow-up visit, at 4, 8, 12 and 16 weeks for participants in the binocular treatment group, compared with the patching group. The binocular treatment group AEDVA improvement at 16 weeks was found noninferior to the patching group improvement (0.28 ± 0.13 (P<0.0001) and (0.23 ± 0.14 logMAR (P<0.0001), respectively.
Discussion
At baseline, the median Randot stereoacuity was 2.3 log arcseconds in both groups. Stereoacuity improvement of 0.40 log arcseconds (P<0.0001) and improved binocular VA of 0.13 LogMAR (P<0.0001) was observed in the binocular treatment group, with similar improvements in the patching group in preschool Randot stereoacuity (0.40 log arcseconds, P<0.0001) and binocular VA (0.09 logMAR, P<0.0001), with no significant difference between improvements in the 2 groups in either Randot stereoacuity (difference 95% CI (-0.27,-0.27; p=0.76)) and binocular VA (difference 0.041 95% CI (-0.002, 0.085; p=0.07)). Moreover, at 16 weeks, 75% of the children had a Randot stereo acuity of better than 2.3 log arcseconds in the binocular treatment group and 2.6 log arcseconds in the patching group.
Last but not least, adherence monitoring in the binocular treatment group was accurately monitored by using the eye tracking system data. Moreover, only the actual screen watching time was taken into account in calculating adherence. If the child’s eye gaze was not on the screen or if the treatment glasses were not worn, the treatment was paused, the child was alerted and the pause time was not calculated as the overall treatment time. Adherence in the patching group was recorded by subjective logbook reporting performed by the guardians. Adherence was found to be significantly higher in the binocular treatment group compared to the control group median (91% vs. 83%; P=0.011). Mean adherence in the binocular treatment group was also greater than that of the patching group (93% vs. 78%).
Safety data shows that no serious adverse events were reported, with no notable changes were found in the nonamblyopic eye VA (no significant linear trend was found for the VA change in the nonamblyopic eye for the type of treatment, binocular treatment or patching (P>0.05 at all visits; the Cochran- Armitage trend test), regardless of treatment group (specifically monitored theoretical risks of a digital dichoptic system treatment included diplopia, eye strain and seizures). Moreover, at 16 weeks, 3 participants in the patching group had a worsening of the nonamblyopic eye VA of >1 line, as opposed to no participants in the binocular treatment group.
In summary, it seems as though a novel digital, eye tracking based dichoptic eye tracking based home treatment system is as effective as patching for the treatment of amblyopia (anisometropic, small angle strabismus or both), as reported in an evaluator masked multicenter randomized clinical trial in children aged 4 to 9 years of age. As opposed to some prior studies showing a relation of a younger age and no prior treatment with a better outcome for binocular therapy, there was no statistically significant effect of age and prior amblyopia therapy in this study.
Further, the amount of time spent on treatment can be substantially shorter with this newer system compared to patching (120 hours over 16 weeks compared to 224 hours over 16 weeks, respectively), which may also improve compliance and adherence to therapy. In this study, adherence for the treatment group was 91% at 16 weeks, compared to 83% in the patching group and the treatment group gained 2.8 lines over 16 weeks. More importantly, 79% of those in the treatment group achieved a 2 line visual acuity gain, compared to only 61% in the patching group. The treatment group also gained a larger improvement in VA than the patching group did for those with a 3 line or more difference at baseline (3.1 ± 1.6 lines in the treatment group compared to 2.6 ± 1.4 lines in the patching group).
It is noteworthy that both groups improved similarly until week 12, however after 16 weeks only the binocular treatment group continued to demonstrate a significant improvement compared to 12 weeks (P=0.0003), whereas the patching group had reached a plateau (P=0.62). Based on these findings, the study authors suggest the potential for greater improvements with longer binocular treatment periods in the distance VA of amblyopic eyes. This suggests future studies to evaluate the potential of longer treatment durations.
In light of the inconsistent outcomes for stereoacuity in the literature on both the conventional patching therapy and the newer binocular amblyopia treatments, the study authors suggest that the observed improvement in both the stereopsis and the binocular VA may indicate a beneficial effect of treatment on the binocular interaction.
Conclusion
Finally, since adherence is crucial for amblyopia treatment effectiveness, with higher regimen adherence shown to be associated with greater amblyopic eye VA gains, whereas, on the other hand, poor adherence with patching is an important risk factor affecting the child’s final VA improvement, the study authors believe that the higher rates of adherence reported for the binocular treatment can be attributed to the unlimited streamed visual content available to the child, thereby maintaining engagement and interest and thus supporting noninferior outcomes for a fraction of treatment time. The study authors conclude by noting that “this approach to amblyopia treatment represents a safe, engaging and personalized alternative to patching.”
References
- Wygnanski-Jaffe T, Kushner BJ, Moshkovitz A, et al. An eye tracking based dichoptic home treatment for amblyopia: A multicenter randomized clinical trial. Ophthalmology. 2023;130(3):274-85.
[Crossref] [Google Scholar] [PubMed]
- Wang J. Compliance and patching and atropine amblyopia treatments. Vision Res. 2015;114:31-40.
[Crossref] [Google Scholar] [PubMed]
- Holmes JM, Beck RW, Kraker RT, et al. Impact of patching and atropine treatment on the child and family in the amblyopia treatment study. Arch Ophthalmol. 2003;121(11):1625-32.
[Crossref] [Google Scholar] [PubMed]
- Felius J, Chandler DL, Holmes JM, et al. Evaluating the burden of amblyopia treatment from the parent and child’s perspective. J AAPOS. 2010;14(5):389-95.
[Crossref] [Google Scholar] [PubMed]
- Group PEDI. Risk of amblyopia recurrence after cessation of treatment. J Am Assoc Pediatr Ophthalmol Strabismus. 2004;8(5):420-8.
[Crossref] [Google Scholar] [PubMed]
- Birch EE, Jost RM, de La Cruz A, et al. Binocular amblyopia treatment with contrast rebalanced movies. J Am Assoc Pediatr Ophthalmol Strabismus. 2019;23(3):160.
[Crossref] [Google Scholar] [PubMed]
- Jost RM, Hudgins LA, Dao LM, et al. Randomized clinical trial of streaming dichoptic movies versus patching for treatment of amblyopia in children aged 3 to 7 years. Sci Rep. 2022;12(1):4157.
[Crossref] [Google Scholar] [PubMed]
- Birch EE, Li SL, Jost RM, et al. Binocular iPad treatment for amblyopia in preschool children. J Am Assoc Pediatr Ophthalmol Strabismus. 2015;19(1):6-11.
[Crossref] [Google Scholar] [PubMed]
- Xiao S, Gaier ED, Mazow ML, et al. Improved adherence and treatment outcomes with an engaging, personalized digital therapeutic in amblyopia. Sci Rep. 2020;10(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Knox PJ, Simmers AJ, Gray LS, et al. An exploratory study: Prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol Vis Sci. 2012;53(2):817-24.
[Crossref] [Google Scholar] [PubMed]
- Li SL, Reynaud A, Hess RF, et al. Dichoptic movie viewing treats childhood amblyopia. J AAPOS. 2015;19(5):401-5.
[Crossref] [Google Scholar] [PubMed]
- Hess RF, Thompson B. Amblyopia and the binocular approach to its therapy. Vision Res. 2015;114:4-16.
[Crossref] [Google Scholar] [PubMed]
- Levi DM. Rethinking amblyopia 2020. Vision Res. 2020;176:118-29.
[Crossref] [Google Scholar] [PubMed]
- Birch EE, Jost RM, Kelly KR, et al. Baseline and clinical factors associated with response to amblyopia treatment in a randomized clinical trial. Optom Vis Sci. 2020;97(5):316.
[Crossref] [Google Scholar] [PubMed]
- Kelly KR, Jost RM, Dao L, et al. Binocular iPad game vs. patching for treatment of amblyopia in children: A randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1402-8.
[Crossref] [Google Scholar] [PubMed]
- Holmes JM, Manh VM, Lazar EL, et al. Effect of a binocular iPad game vs. part time patching in children aged 5 to 12 years with amblyopia: A randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1391-1400.
[Crossref] [Google Scholar] [PubMed]
- Holmes JM, Manny RE, Lazar EL, et al. A randomized trial of binocular dig rush game treatment for amblyopia in children aged 7 to 12 years. Ophthalmology. 2019;126(3):456-66.
[Crossref] [Google Scholar] [PubMed]
- Gao TY, Guo CX, Babu RJ, et al. Effectiveness of a binocular video game vs. placebo video game for improving visual functions in older children, teenagers and adults with amblyopia: A randomized clinical trial. JAMA Ophthalmol. 2018;136(2):172-81.
[Crossref] [Google Scholar] [PubMed]
- Xiao S, Angjeli E, Wu HC, et al. Randomized controlled trial of a dichoptic digital therapeutic for amblyopia. Ophthalmology. 2022;129(1):77-85.
[Crossref] [Google Scholar] [PubMed]