Short Communication - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 6
A brief note on visconeedling.
Vicente Mascarenhas Menna Barreto*, Carlos Mascarenhas Menna Barreto, Vitor Menna Barreto, Pedro Kern Menna Barreto, Roberta Kern Menna Barreto
Department of Ophthalmology, Medical School of Universidade Federal do Rio Grande do Sul (R.K.M. Barreto), Porto Alegre, Rio Grande do Sul, Brazil
- Corresponding Author:
- Dr. Vicente Mascarenhas Menna Barreto
Department of Ophthalmology
Medical School of Universidade Federal do Rio Grande do Sul
Porto Alegre
Rio Grande do Sul,
Brazil
E-mail: vicente@mennabarreto.med.br
Accepted date: 22 October, 2021
Citation: Barreto, et al. A brief note on visconeedling. J Clin Ophthalmol 2021;5 (6):476-477.
Description
Visconeedling is a new technique that delivers a 6.0 polypropylene suture inside the eye with only a 30 gauge needle and an OVD syringe.
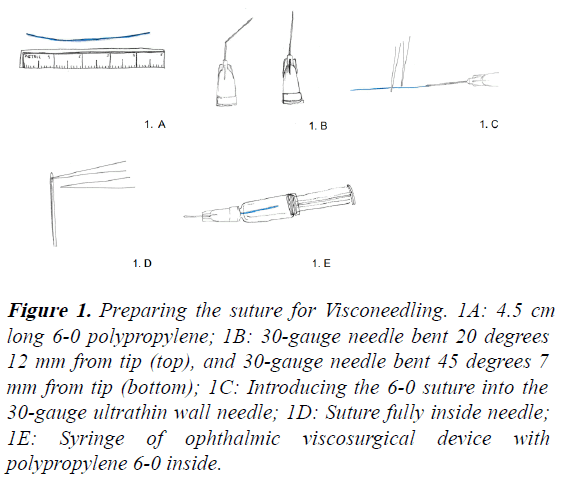
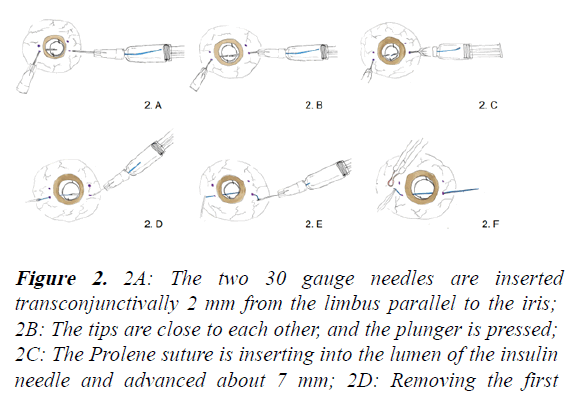
Two 30 gauge needles are used: One attached to an OVD syringe, bent 20 degrees at 12 mm from tip, and the other attached to an insulin syringe, and bent 45 degrees at 7 mm from tip. A 4-5 cm long 6.0 polypropylene suture is fully introduced inside the OVD syringe (Figure 1). The needles are inserted inside the eye 2 mm from limbus. The two tips are put close to each other and, then, the plunger of the OVD syringe is pushed until the suture starts to penetrate the lumen of the insulin needle at least 7 mm (Figure 2).
Figure 1: Preparing the suture for Visconeedling. 1A: 4.5 cm long 6-0 polypropylene; 1B: 30-gauge needle bent 20 degrees 12 mm from tip (top), and 30-gauge needle bent 45 degrees 7 mm from tip (bottom); 1C: Introducing the 6-0 suture into the 30-gauge ultrathin wall needle; 1D: Suture fully inside needle; 1E: Syringe of ophthalmic viscosurgical device with polypropylene 6-0 inside.
Figure 2: 2A: The two 30 gauge needles are inserted transconjunctivally 2 mm from the limbus parallel to the iris; 2B: The tips are close to each other, and the plunger is pressed; 2C: The Prolene suture is inserting into the lumen of the insulin needle and advanced about 7 mm; 2D: Removing the first needle from the eye; 2E: Holding the end of the suture and removing the other needle outside the eye; 2F: With a hightemperature ophthalmic cautery deform, at least 2 mm of the suture builds a flange.
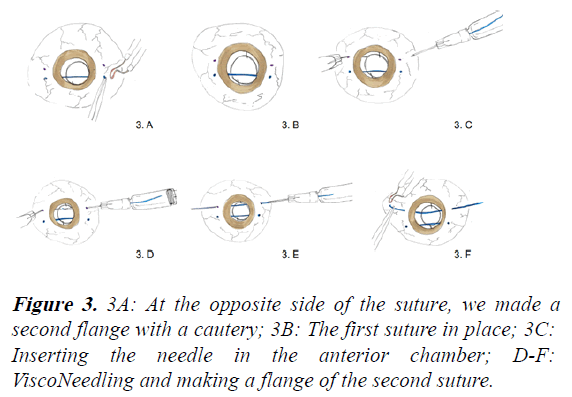
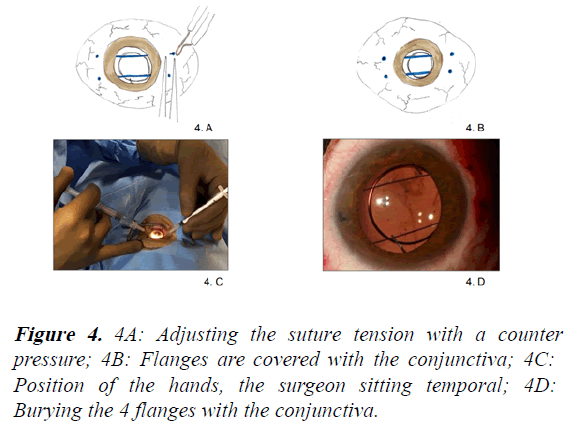
After that, the 30 gauge needle attached in an insulin syringe is removed from the eye. It is important to hold the end of the suture when it comes out before removing the other needle, so that the suture remains inside the eye. With the help of a hightemperature ophthalmic cautery, the tips of the suture are deformed in order to create a flange (Figures 3 and 4).
This principle of injecting a suture in the eye without any special needle or micro forceps could be a good alternative for many steps of surgeries that involve passing a suture inside the eye. This study, explain a procedure used in two cases after several attempts to minimize iris capture of the IOL (iridotomy, miotic medicine, and mechanical push) failed to result in permanent iris capture reduction. The Yamane procedure was used in the first case on a 58-year-old man who had been injured and had his capsular bag–IOL complex dislocated. The second procedure was carried out on a 49-year-old man who had undergone vitrectomization and was suffering from the same problem.
We have been using visconeedling for 2 years in cases of IOL iris capture, the most common complication of Yamane’s technique [1,2] (Figures 2-4).
It is also possible to use it in “Safety-Basket Suture” technique, by Masket and Nicole Fram, where a safety net is used for surgical management of malpositioned PC IOL in postvitrectomy eyes [3].
We think that, with visconeedling, it could be quicker and simpler to pass the horizontal and vertical sutures of 6.0 polypropylene than the way proposed by the authors.
Considering the “Novel Double-Flanged technique for managing Marfan syndrome and Microspherophakia” by Canabrava, et al. we believe that it’s possible to place the 5.0/6.0 polypropylene into the lumen of 30 gauge needle using only visconeedling instead of microforceps [4,5].
Conclusion
Furthermore, we suppose that visconeedling could facilitate to penetrate the iris and to manage the 6.0 suture inside the eye, regarding Masayuki Akimoto’s technique, “Repairing iridodialysis by riveting”. In all these techniques that use flanges it is of paramount importance to adjust the tension of the suture and cover them with conjunctiva and tenon in order to avoid the exposure of the flanged sutures.
References
- Barreto VM, Barreto CM, Barreto PK, et al. Correcting optic capture with 2 flanged 6-0 sutures after intrascleral haptic fixation with visco needling. J Cataract Refract Surg. 2021; 47:1234-6.
- Yamane S. Double needle technique: Rationale and results. 2019; 345–349.
- Masket S, Fram NR. Safety-basket suture for management of malpositioned posterior chamber intraocular lens. J Cataract Refract Surg. 2013; 39:1633-5.
- Canabrava S, Lima AC, Arancibia AE, et al. Novel double-flanged technique for managing marfan syndrome and microspherophakia. J Cataract Refract Surg. 2020; 46:333-9.
- Kusaka M, Miyamoto N, Akimoto M. Repairing iridodialysis by riveting with a double-flanged polypropylene suture. J Cataract Refract Surg. 2019; 45:1531-4.