Case Report - Biomedical Research (2018) Volume 29, Issue 11
Primary lumbar spinal epidural b-lymphoblastic lymphoma: A case report
Hongyuan Liu1#, Lin Wang2#, Ying Ren3#, Qi Zhong1, Zongping Li1* and Mingqi Qu4*
1Department of Neurosurgery, Mianyang Central Hospital, Mianyang, Sichuan, PR China
2Department of Neurosurgery, Nanchong Central Hospital, Sichuan, PR China
3Department of Pathology, the People’s Hospital of Zhengzhou University, Zhengzhou, Henan, PR China
4Department of Neurosurgery, the People’s Hospital of Zhengzhou University, Zhengzhou, Henan, PR China
#These authors contributed equally to this work
- *Corresponding Author:
- Zongping Li
Department of Neurosurgery
Mianyang Central Hospital, PR China
Mingqi Qu
Department of Neurosurgery
The People’s Hospital of Zhengzhou University
Zhengzhou, P.R. China
Accepted on April 11, 2018
DOI: 10.4066/biomedicalresearch.65-17-2361
Visit for more related articles at Biomedical ResearchAbstract
Background: Primary spinal epidural non- Hodgkin’s lymphoma (PSENHL) is an uncommon disease. Most PSENHL are diffuse large B-cell lymphomas, and thoracic spine is the most common site of involvement. Primary spinal epidural B-Lymphoblastic Lymphoma (LBL) is particularly rare. So far only one case at thoracic segment was reported.
Case presentation: A 16-year-old female presented with a history of pain in her lower back and lower extremities for 7 d, pain aggravated and weakness for 4 d, urinary incontinence for 2 d. Magnetic Resonance Imaging (MRI) scan revealed an extradural mass lesion at L3 to L5 level, which was at first suggestive of a neurogenic tumor. L4-L5 laminectomy was performed and tumor was totally resected. Histopathological examination after surgery revealed B-lymphoblastic lymphoma (LBL)/-Acute Lymphoblastic Leukemia (ALL). Postoperative blood counts, bone marrow biopsy and aspiration were negative. The final diagnosis of primary spinal epidural B-LBL was made. Patient was treated with vincristine, daunorubicin, cyclophosphamide, L-asparaginase and prednisone after surgery. After 2 months of follow up, all the symptoms were relieved.
Conclusion: Primary spinal epidural non-Hodgkin’s lymphoma should be considered in the differential diagnosis of the patients who present with spinal cord or cauda equina compression. This is the first primary spinal epidural B-LBL at lumbar reported as we known.
Keywords
Primary spinal, Epidural, B-Lymphoblastic lymphoma, Non-Hodgkin’s lymphoma.
Introduction
Primary Spinal Epidural Non-Hodgkin’s Lymphoma (PSENHL) is an uncommon disease, accounting for 9% of epidural spinal tumors and for 0.1% to 3.3% of all lymphomas [1]. In clinical, patients with PSENHL presented with symptoms of spinal Compression, such as upper or lowed limb weakness, back or neck pain, sensory deficits, bladder or bowel functions lost, etc. [2]. Most PSENHL are diffuse large B-cell lymphomas, and thoracic spine is the most common site of involvement [3-5]. Primary spinal epidural B-Lymphoblastic Lymphoma (B-LBL) is particularly rare. So far only one case at thoracic segment was reported [6]. Here we present a case of lumbar spinal epidural B-LBL at L3-L5 in a 16 y old female, which was at first suggestive of a neurogenic tumor.
Case Presentation
Written informed consent was obtained from the parent of the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
A 16-year-old female presented to the Department of Neurosurgery at the People’s Hospital of Zhengzhou University, with 7 d history of pain in her lower back and lower extremities. She also had developed weakness of her left legs for 4 d and urinary retention for 2 d. Pain got worse after movement, bending forward was relieved. The medical history indicated no abnormalities. On examination patient was in good general condition, no enlarged nodes or viscera, L3-L5 spinous tenderness and no percussion. Central nervous systemic examination revealed decreased muscular strength with grade 4/5 and decreased sensation in the left lower limb.
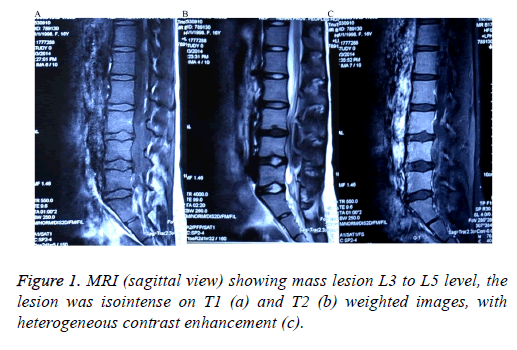
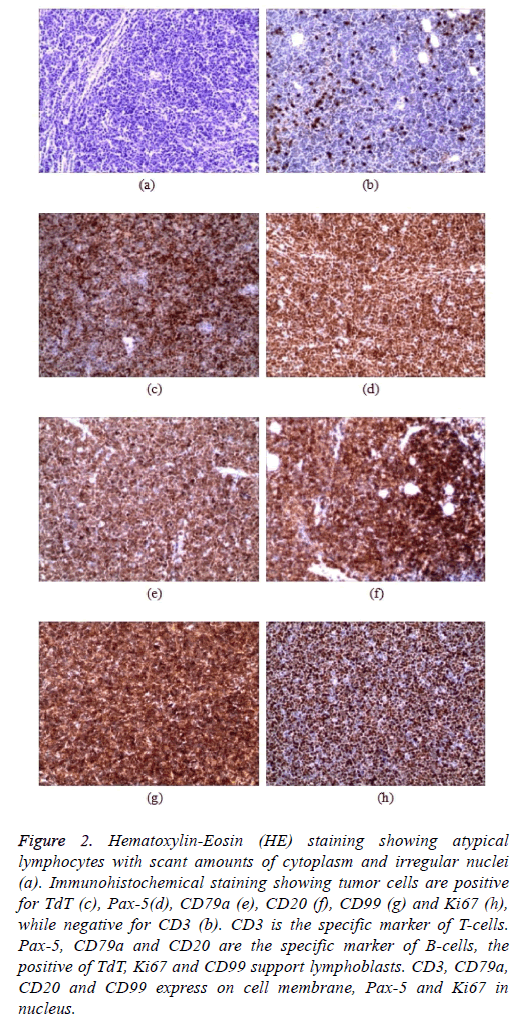
Chest and abdominal Computed Tomography (CT) were normal. Magnetic Resonance Imaging (MRI) scan showed an extradural mass lesion of size 1.5 cm × 5.7 cm at L3 to L5 level. On T1 and T2 weighted images, the lesion was isointense and grown to the L3/4 and L4/5 intervertebral, and heterogeneous contrast enhancement after intravenous gadolinium administration (Figure 1). She was operated with L3-L5 laminectomy and complete resection of the tumor. Intraoperatively, the tumor was extradural, fleshy, pale, suckable, moderately vascular, without dura infiltration. Histopathology specimen showed soft tissue heavily infiltrated by sheets of atypical lymphocytes with scant amounts of cytoplasm and irregular nuclei. Mitoses were easily identified. Immunohistochemistry showed the tumor cells to be strongly positive for CD10, TdT, CD99, Pax-5, CD20, CD79a and Ki67, while negative for CD3, CD2, CD30, CD34 and CD138 (Figure 2). The morphologic and immunophenotypic profile was most consistent with a diagnosis of B-lymphoblastic lymphoma (LBL)/-Acute Lymphoblastic Leukemia (ALL). After surgery, the patient’s muscular strength and sensation in the left lower extremities improved greatly. Postoperative blood counts, bone marrow biopsy and aspiration were negative. She was treated with systemic chemotherapy with vincristine, daunorubicin, cyclophosphamide, L-asparaginase and prednisone (VDCLP). After 2 month of follow up, she was relieved of urinary incontinence, pain in back and lower limb.
Figure 2: Hematoxylin-Eosin (HE) staining showing atypical lymphocytes with scant amounts of cytoplasm and irregular nuclei (a). Immunohistochemical staining showing tumor cells are positive for TdT (c), Pax-5(d), CD79a (e), CD20 (f), CD99 (g) and Ki67 (h), while negative for CD3 (b). CD3 is the specific marker of T-cells. Pax-5, CD79a and CD20 are the specific marker of B-cells, the positive of TdT, Ki67 and CD99 support lymphoblasts. CD3, CD79a, CD20 and CD99 express on cell membrane, Pax-5 and Ki67 in nucleus.
Discussion
PSENHL is defined as Non-Hodgkin’s Lymphoma (NHL) arising within the spinal epidural space. NHL is a heterogeneous collection of lymphoproliferative malignancies. There are over 40 different NHL histologies [1]. LBL, including B-LBL and T-LBL is an uncommon one, accounting for approximately 2% of all NHL. B-lineage LBL comprises 10% of all LBLs, it occurs most frequently in childhood [6]. Compression of the spinal cord as the first manifestation of primary spinal B-LBL is particularly rare. To the best of our knowledge, only one case at T2-T5 has been reported to date [7]. The patient reported in the present case was a 16-year-old female with primary lumbar spinal epidural B-lymphoblastic lymphoma, presenting with back and lower limb pain, lower limb weakness and sensory deficits, and urinary incontinence.
In clinical, patients with PSENHL presented with unspecific performance in symptoms and imaging procedure. It is quite often confused with other spinal tumors. PSENHL is negative in the X-ray and lack specific performance in CT examination, however, CT examination is useful on NHL in mediastinal and retroperitoneal. MRI is a most valuable adjunct examination to spinal disease, primary spinal lymphomas are general iso/ hypointense on both T1/T2 weighted images and abnormal enhancement on postcontrast images. The patient reported has no exception in chest and abdominal CT, lesion shown isointense on T1 and T2 weighted images in MRI led to the misdiagnosis of neurogenic tumor, which incidence much more commonly than PSENHL. However, histopathological examination after surgery revealed B-lymphoblastic lymphoma (LBL)/-Acute Lymphoblastic Leukemia (ALL).
Accordingly, LBL and ALL were considered the same disease with different clinical presentations for decades. By convention, the word “lymphoma” is used if there is a bulky lesion in the mediastinum or elsewhere, with no or minimal evidence of peripheral blood and bone marrow involvement. In general, a threshold of <25% bone marrow blasts is used for defining lymphoma [8]. Because blood counts and bone marrow biopsy were negative in our patient, a diagnosis of primary spinal epidural B-LBL was made.
As primary spinal epidural B-LBL are very rare, there are no set guidelines for treatment. PSENHL is sensitive to radiotherapy and chemotherapy like other NHL. Chemoradiotherapy was recommended to the patient after surgery. However, considering the risk for side effects of radiationrelated, the patient refused radiation treatment. Chemotherapeutic option for LBL patients is based on intensive multi-drug leukemia chemotherapy protocols [9]. The regimens contain several drugs, such as fractionated cyclophosphamide, vincristine, adriamycin, L-asparaginase, prednisone, methotrexate, cytarabine, thioguanine, nitrosoureas and etoposide. Several studies showed that treatment with ALL-type chemotherapy regimens could improve complete response and disease-free survival rates of the LBL patients [9-11], such as Hyper-CVAD (fractionated cyclophosphamide, vincristine, adriamycin and dexamethasone). In our case, the patient received chemotherapy with VDCLP after surgery. After one cycle of treatment, the patient recover form urinary incontinence, pain in back and lower limb.
The present case demonstrated that primary spinal epidural non-Hodgkin’s lymphoma should be considered in the differential diagnosis of the patients who present with spinal cord or cauda equina compression with prodrome of back pain. Surgery followed by chemotherapy can result in significant neurological improvement in younger patients.
Conclusion
Primary lumbar lymphoma should be considered as one of the differential diagnosis of neurogenic tumor.
References
- Maxwell SA, Mousavi-Fard S. Non-Hodgkins B-cell lymphoma: advances in molecular strategies targeting drug resistance. Exp Biol Med 2013; 238: 971-990.
- Monnard V, Sun A, Epelbaum R, Poortmans P, Miller RC, Verschueren T, Scandolaro L, Villa S, Majno SB, Ostermann S, Ozsahin M, Mirimanoff RO. Primary spinal epidural lymphoma: patients profile, outcome, and prognostic factors: a multicenter rare cancer network study. Int J Rad Oncol Biol Phys 2006; 65: 817-823.
- Boukobza M, Mazel C, Touboul E. Primary vertebral and spinal epidural non-Hodgkins lymphoma with spinal cord compression. Neuroradiology 1996; 38: 333-337.
- Sachdev RK, Sen A, Pathak A, Jangid DR. Primary extradural non-hodgkins lymphoma. Ind J Nucl Med 2012; 27: 185-186.
- Zheng JS, Wang M, Wan S, Zhou YQ, Yan M, Chen QF, Zhan RY. Isolated primary non-Hodgkins lymphoma of the thoracic spine: a case report with a review of the literature. J Int Med Res 2010; 38: 1553-1560.
- Soslow RA, Baergen RN, Warnke RA. B-lineage lymphoblastic lymphoma is a clinicopathologic entity distinct from other histologically similar aggressive lymphomas with blastic morphology. Cancer 1999; 85: 2648-2654.
- Khalid I, Rival J, Salama ME, Banghar PK, Janakiraman N. Unusual presentations of hematologic malignancies: CASE 2. Precursor B-cell lymphoblastic lymphoma presenting as spinal cord compression. J Clin Oncol 2004; 22: 1331-1333.
- Recine M, Castellano-Sanchez AA, Sheldon J, Schwartz M, Cabello-Inchausti B. Precursor B-cell lymphoblastic lymphoma/leukemia presenting as osteoblastic bone lesions. Ann Diagn Pathol 2002; 6: 236-243.
- Cortelazzo S, Ponzoni M, Ferreri AJ, Hoelzer D. Lymphoblastic lymphoma. Crit Rev Oncol Hematol 2011; 79: 330-343.
- Hoelzer D, Gokbuget N, Digel W, Faak T, Kneba M, Reutzel R, Romejko-Jarosinska J, Zwolinski J, Walewski J. Outcome of adult patients with T-lymphoblastic lymphoma treated according to protocols for acute lymphoblastic leukemia. Blood 2002; 99: 4379-4385.
- Thomas DA, OBrien S, Cortes J, Giles FJ, Faderl S, Verstovsek S, Ferrajoli A, Koller C, Beran M, Pierce S, Ha CS, Cabanillas F, Keating MJ, Kantarjian H. Outcome with the hyper-CVAD regimens in lymphoblastic lymphoma. Blood 2004; 104: 1624-1630.