Case Report - Archives of General Internal Medicine (2023) Volume 7, Issue 4
Unusual presentation of Takayasu Arteritis as a Non-Aneurysmal bleed
Devarsh N Shah*, Harshal Prakashbhai Chorya, Palak PatelDepartment of General Medicine, Medical College Baroda, Vadodara, India
- *Corresponding Author:
- Devarsh N Shah
Department of General Medicine
Medical College Baroda, Vadodara, India
E-mail: devshah980@gmail.com
Received: 26-Jul-2023, Manuscript No. AAAGIM-23-110168; Editor assigned: 28-Jul-2023, PreQC No. AAAGIM-23-110168(PQ); Reviewed: 11-Aug-2023, QC No. AAAGIM-23-110168; Revised: 16-Aug-2023, Manuscript No. AAAGIM-23-110168(R); Published: 23-Aug-2023, DOI:10.35841/aaagim-7.4.184
Citation: Shah DN. Unusual presentation of Takayasu Arteritis as a Non-Aneurysmal bleed. Arch Gen Intern Med. 2023;7(4):184
Abstract
Takayasu Arteritis is a large and medium vessel vasculitis mainly affecting the aorta and its branches. The early stages of the disease pose a diagnostic challenge due to the absence of specific symptoms, but as the condition progresses, patients may present with more recognizable signs such as the absence of a pulse and a range of other cardiovascular and neurological manifestations, some of which can be fatal. One such manifestation, which this patient presented with, is Subarachnoid Haemorrhage (SAH). SAH typically occurs as a result of the rupture of aneurysmal dilatation of the cerebral arteries due to chronic inflammatory changes to the vessel wall. However, in some cases, it can also manifest spontaneously, as observed in this particular patient without any evidence of cerebral aneurysms. The underlying mechanism for this finding is poorly understood but can be attributed to the rupture of newly developed collateral blood vessels, which form as a compensatory response to chronic hypo perfusion caused by the abnormal narrowing of cranial arteries. The condition can be managed conservatively with corticosteroids, and worsening prevented with modern surgical interventions. In conclusion, it is important to reach the diagnosis of Takayasu Arteritis and initiate subsequent management at the earliest to prevent fatal outcomes. Also importantly, further research is required into understanding the pathophysiology behind the development of non-aneurysmal subarachnoid haemorrhage in Takayasu Arteritis which can aid in developing preventive and treatment options for the same
Keywords
Hypo perfusion, Subarachnoid haemorrhage, Takayasu arteritis, Supraclinoid segment.
Introduction
Vasculitis is a condition due to chronic inflammation of the blood vessels which leads to abnormalities of the vessel wall and lumen. One such condition affecting the large as well as medium sized arteries and their branches is called Takayasu Arteritis. This condition mainly affects young Asian females but can also present later in life. Patients primarily present with fever, anorexia and weight loss, lethargy and generalized fatigue, and often also present with hypertension and an absence of peripheral pulses due to claudication of the upper limb. Common neurologic symptoms include dizziness and disturbance in vision but rarely patients can also present with headache due to subarachnoid hemorrhage [1,2]. Subarachnoid hemorrhage can be explained by the rupture of aneurysmal dilatation of the cerebral arteries but spontaneous hemorrhage without any aneurysms is highly infrequent. Here we report a case of non-aneurysmal subarachnoid hemorrhage as a complication of Takayasu Arteritis.
Case Presentation
A 46 year old female presented with a complaint of severe Headache for the past 4-5 days along with mild weakness and lethargy during the same period. The patient did not have any other complaints apart from those presented with, and was referred from another clinic where she was managed conservatively but without any relief. The patient was diagnosed with Takayasu Arteritis 9 months prior to the current presentation when she presented with long-standing recurring constitutional symptoms and mild headache which was followed-up with radiologic confirmation. The presentation during the current visit was unusual as the patient experienced a severe headache like never before. In addition, she had experienced new onset episodes of dizziness and low blood pressure since the past few days. On examination, there was presence of a feeble pulse bilaterally but blood pressure was not measurable in either of the brachial arteries. Subsequently on admission, blood pressure reading on the monitor ranged from 110-120 mmHg systolic to 70-80mmHg diastolic which was normal.
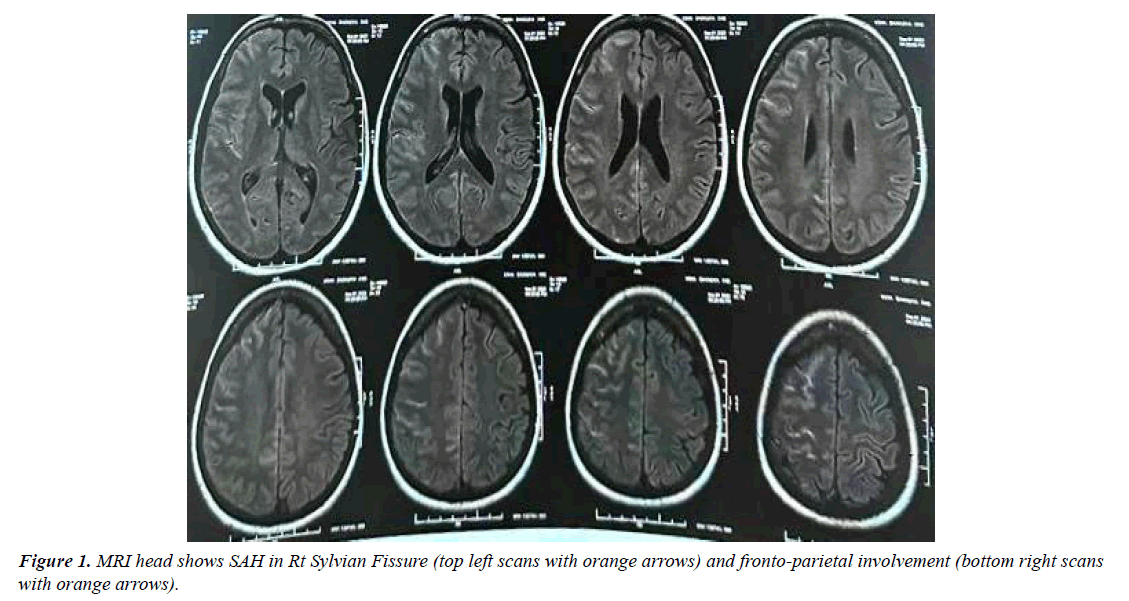
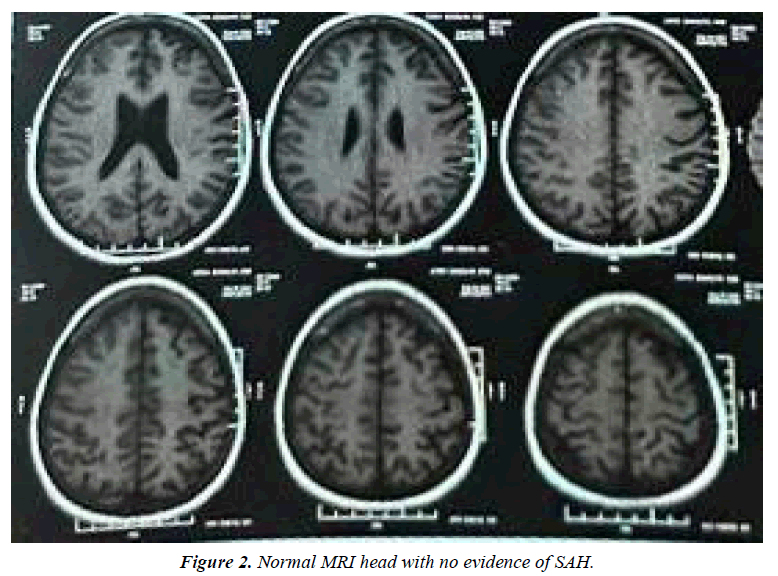
Blood and Radiologic investigation was ordered for further evaluation where blood work-up did not show any major findings apart from elevated ESR but MRI scan of the brain showed a Subarachnoid Hemorrhage (SAH) in the Right Cerebral hemisphere [Figure 1]. SAH was present in the right Sylvian fissure suggesting right MCA involvement, with minimal subdural hematoma in the right fronto-parietal area. Mild cerebral edema was also noted with cerebral sulcus spaces more affected on the right. A previous T1/T2 weighted MRI scan of the brain 9 months prior showed no acute infarct, intracranial hemorrhage or any evidence of venous sinus thrombosis [Figure 2].
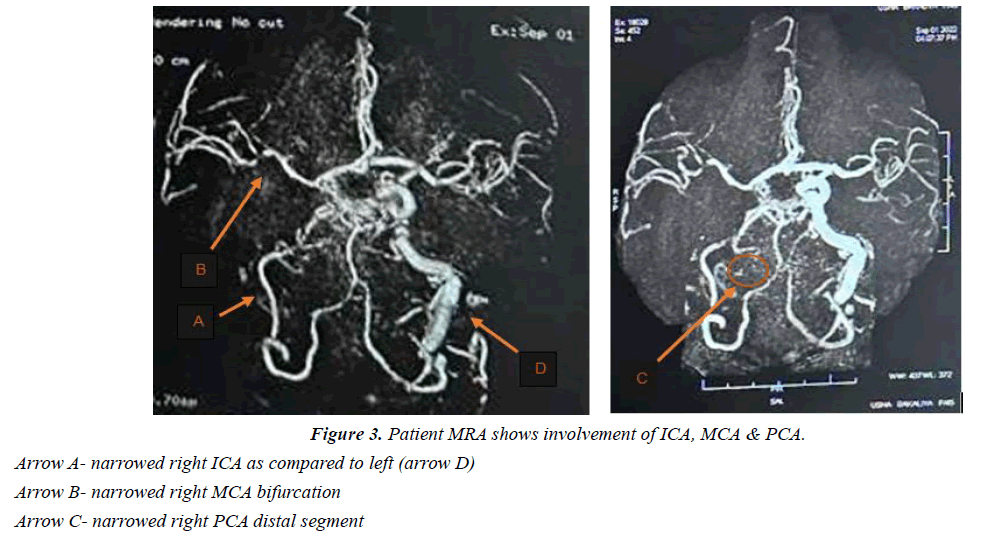
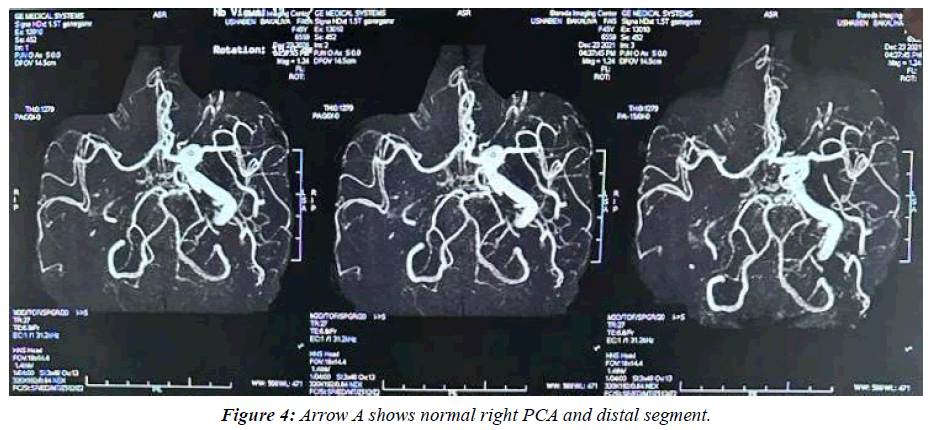
MRA of the brain was also done which showed narrowing of various segments of Right PCA, MCA and ICA without any aneurysmal dilatations [Figure 3]. There was presence of diffuse narrowing of distal segment of right PCA with mild narrowing present at right MCA bifurcation level and recanalization of insular segment of MCA, as well as reduced caliber of basilar artery along with diffuse wall thickening and narrowing of petrosal, cavernous and supraclinoid segment of right ICA. No associated evidence of aneurysms, mass effect or midline shift was seen in this patient. MRA scan at the time of diagnosis also showed a presence of narrowing in the petrosal, cavernous and supraclinoid segment of right ICA, along with mild narrowing of insular segment but without any involvement of PCA [Figure 4].
Patient was admitted and managed conservatively. She was prescribed Prednisone 10mg a day after initial diagnosis which was presently increased to 20mg a day with significant improvement, stalling the need for immunotherapy. After 2 days of medical and conservative management, a plain CT scan of the head was done which showed presence of sulcal effacement in the right cerebral hemisphere suggestive of mild cerebral edema without any evidence of intracranial hemorrhage.
Discussion
Takayasu Arteritis (TA), also known as pulseless disease, is a large vessel vasculitis which usually involves the aorta and its branches. The pathophysiology of this condition is not well understood but it is mainly due to granulomatous inflammation of the large and medium sized arteries. The chronicity of the inflammation leads to subsequent fibrosis and thickening of the entire thickness of the arterial wall, which eventually causes narrowing of the vessel and ischaemic manifestations. There is also an associated breakdown of the elastic fibers and smooth muscles of tunica media which in turn aids in development of aneurysms. These aneurysms can rupture and cause intracranial bleeding, but cerebral hemorrhage in the absence of abnormal vessel dilation is a very rare and poorly understood presentation.
Initial phase of the disease (pre-pulseless phase) presents with non-specific symptoms such as fever, bone and muscle pain, generalized fatigue, and loss of weight which makes it difficult to diagnose at the early stage which is summated with patient’s hesitance in seeking medical help due to its mild and remitting nature. This was probably the case with this patient who directly presented with late stage findings requiring urgent medical attention. In the later stages of the disease, patients develop vascular and neurologic findings (pulseless phase) including hypertension due to stenosis of renal vessels, dizziness and syncope due to occlusion of carotid arteries, upper limb claudication responsible for “pulselessness” and ischaemic changes in the upper arm, and also sometimes eventual heart failure. Very few cases have been reported with Subarachnoid Hemorrhage (SAH) occurring spontaneously in the absence of cerebral vessel aneurysmal dilation [3,4].
It is established that pulseless disease involves large and medium sized arteries but one study done by Shuaib UA et al, also suggested small vessel involvement in Takayasu which can possibly explain the development of non-aneurysmal SAH [5]. They theorized its mechanism to be similar to that of the recurrent relapsing and remitting presentation of erythema nod sum in TA. Another proposed mechanism by them suggested growth of new collateral arterioles due to hypoxia and prolonged hypo perfusion in TA, which in turn could easily rupture and bleed attributing to their fragile nature. The latter concept was possibly evident in this case as the SAH likely occurred due to the rupture of collaterals developing around the MCA branch supplying the sylvian fissure territory. The previous brain scans showed narrowing of the insular segment that was not overtly evident during the patient’s recent scans which suggest recanalization and angiogenesis as an outcome of chronic hypo perfusion in that region. However, this is conjectural without establishing confirmatory evidence. The rupture of these collateral vessels in Takayasu Arteritis-related SAH can be attributed to multiple factors. The current understanding suggests chronic inflammation and ongoing damage to blood vessels which weaken the collaterals, making them more susceptible to rupture. Additionally, the hemodynamic stress placed on these vessels due to the compensatory blood flow through collaterals can further contribute to their vulnerability.
American College of Rheumatology had previously given clinical criteria’s for classifying TA but lately the diagnosis is mainly based on the radiologic (especially angiographic) findings. Imaging techniques such as angiography can show arterial wall thickening, lumen changes, development of collateral vessels, and perfusion [6,7]. First line management includes corticosteroids, and immunosuppressive can also be added but there is very little evidence of their additional benefits. Surgical revascularization has also gained recognition recently and has even become the primary choice of management in majority of the cases, showing significantly improved outcomes. Another surgical modality includes arterial reconstruction which is predominantly preferred for aortic involvement. Surgical therapy is preferred commonly due to the younger age of presentation, which provides better tolerability and helps avoid side effects due to long term medical therapy [8].
Conclusion
The diagnosis of Takayasu Arteritis is difficult when presented with general constitutional symptoms, requiring a high level of suspicion. The complications can be life threatening and hence, the patient should be closely observed for the development of cardiovascular and neurologic manifestations such as cerebral hemorrhage. Subarachnoid hemorrhage can happen due to rupture of the abnormal dilations in cranial arteries but spontaneous SAH is very uncommon. More such studies can help establish confirmatory explanations of the speculated causes of spontaneous SAH, which would subsequently aid in the development of preventive and therapeutic measures against such life threatening incidents.
References
- Malu A, Kolate DS, Patvekar M, et al. Takayasu Arteritis In Pregnancy. J Pharm Negat. 2023:665-9.
- Joshi H, Allen J, Qiu D, et al. Spontaneous non-aneurysmal subarachnoid hemorrhage in Takayasu arteritis: A case implicating hyperperfusion and cerebral dysautoregulation. BMJ Case Rep. 2019;5(2):20180113.
- Dal Soo Kim JK, Do Sung Yoo PW, et al. Takayasu's Arteritis Presented with Subarachnoid Hemorrhage. J Korean Med Sci. 2002;17:695-8.
- Seung-Jae HY, Sung-Nam HW, Taek-Kyun NA, et al. Takayasu's Arteritis Complicated With Subarachnoid Hemorrhage and Hematomyelia-Case Report. Neurol Med Chir. 2011;51(2):119-22.
- Shuaib UA, Kate M, Homik J, et al. Recurrent non-aneurysmal subarachnoid haemorrhage in Takayasu arteritis: is the cause immunological or mechanical?. Case Rep. 2013:bcr2013008825.
- Angeli E, Vanzulli A, Venturini M, et al. The role of radiology in the diagnosis and management of Takayasu's arteritis. J Nephrol. 2001;14(6):514-24.
- Zhu FP, Luo S, Wang ZJ, et al. Takayasu arteritis: imaging spectrum at multidetector CT angiography. Brit J Radiol. 2012;85(1020):e1282-9.
- Misra DP, Wakhlu A, Agarwal V, et al. Recent advances in the management of Takayasu arteritis. Int. J Rheum Dis. 2019;22:60-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref