Review Article - Journal of Pain Management and Therapy (2022) Volume 6, Issue 2
The role of early pain management referral in the oncology population.
Michelle L. Hulman*
Department of Graduate Nursing, University of Wisconsin at Oshkosh, Oshkosh, Wisconsin, USA
- *Corresponding Author:
- Michelle L. Hulman
Department of Graduate Nursing
University of Wisconsin at Oshkosh
Oshkosh, Wisconsin, USA
E-mail: hulmam80@uwosh.edu
Received: 23-Feb-2022, Manuscript No. AAPMT-22- 56854; Editor assigned: 25-Feb-2022, PreQC No. AAPMT-22- 56854 (PQ); Reviewed: 11-Mar-2022, QC No. AAPMT-22- 56854; Revised: 14-Mar-2022, Manuscript No. AAPMT-22- 56854 (R); Published: 21-Mar-2022, DOI: 10.35841/aapmt- 6.2.106
Citation: Hulman LM. The role of early pain management referral in the oncology population. J Pain Manage Ther. 2022;6(2):106
Abstract
Background: Inadequately managed pain in the oncology patient is common occurrence that should not be accepted as the norm. A literature review has uncovered the need to address and control this issue. Facilitating an early partnership between oncology and pain management has proven beneficial for quality-of-life indicators, exclusively in adult oncology management. By providing a team-based approach to care, oncology patients can become mutual decision-makers and drivers of their healthcare trajectory.
Purpose: To determine the impact of early referral to pain management specialists compared to oncology managed pain control.
Method: Oncology patients with cancer-related pain completed the Brief Pain Inventory (BPI) (Short Form) pain diary during their initial consultation and with subsequent routine follow-up visits with a pain management specialist. At least three months of data were collected on each participant.
Results: A total of four patients were included in this study. Requirements included an active therapy plan of radiation and/or chemotherapy. Each participant consistently rated improvements in metrics of pain, mood, and sleep by the end of the data collection timeframe.
Conclusion: Integrating a pain management consultation within routine oncology care was shown to improve pain management in the four participants by means of properly addressing pain and providing additional means of support during their cancer journey.
Keywords
Cancer, Pain management, Oncology, Disease.
Introduction
Uncontrolled pain in oncology patients is, unfortunately, a regular occurrence. Up to 90% of advanced-stage cancer patients admit to experiencing pain that is moderate to severe at some point during their disease course, [1]. Medical oncologists are responsible for creating and facilitating a treatment plan and initial management of disease-related symptoms. This includes placing referrals for other specialties, such as radiation oncology, palliative care, and surgical oncology, as clinically indicated. A missing component in this list is pain management. Pain management can offer other modalities and interventional procedures that another specialist cannot accomplish.
Problem statement
With the sheer number of oncology patients who experience pain, early intervention from pain management specialists is crucial. Pain management specialists can offer a variety of care that cannot be obtained while under oncology services alone. Coordination between oncology and pain management ensures patients receive high-quality supportive care during their oncology journey. With much of the medical oncologist's time consumed by management focused on active cancer treatments, little time is left for the provider to adequately manage the patient's pain. Pain management is a separate and distinct entity that can offer treatment modalities, other than solely medication, to promote minimization of pain and improved quality of life. Pain management specialists should be referred to as a standard of care practice in a similar fashion to social services, nutrition consultations, or therapies.
Need and Significance
Need
Well-rounded, holistic care for oncology patients is essential to their overall wellbeing. Pain impacts all aspects of the oncology patient's life, so every effort should be put forth to prevent and manage this issue. As it currently stands, this need is not being met for every patient. Pain, especially as it pertains to cancer, is a highly complex, unique, and individualized concern, so a referral to a pain specialist is an appropriate modality to manage pain-related symptoms and guide care plans for the oncology patient.
Significance
With the success of the project, oncology patients have quick turnaround time to see a pain specialist. Opening a line of communication between two separate specialized clinics would break down the barrier for the oncology patient. Patients have more resources and opportunities for pain control assistance during their cancer journey, thus improving their quality of care and overall pain control. By providing a team approach to care, oncology patients can become mutual care-plan decision-makers and drivers of their healthcare trajectory.
Literature Review
A literature review yielded evidence to uncover the benefits of adding pain management specialists to the oncology population's care plan. When conducting the literature review, keywords including "oncology care”, "pain management", "cancer pain", and "pain management referral" were utilized through the John Hopkins Model tool for literature review.
Oncology population
Early referral to pain management is essential to oncology patients and their families. This service has a host of benefits, to include symptom control, coping strategies, and emotional support. The pain management team can assist in breaking down communication barriers, determining risk assessments regarding opioids, managing breakthrough pain, and offering non-opioid pain control options [2]. Involving pain specialists in the oncology care plan in an upfront manner may change how oncology patients perceive their overall quality of life and pain symptoms.
Central concept
Untreated pain, communication barriers, risk assessment, and non-opioid versus opioid management of pain are central concepts in pain management for this population. A pain management group offers different modalities to assist with pain control, which are not available outside of this specialty. To gain access to these tools pain management specialists need to be directly involved in driving this care [1].
Untreated pain
Providers in the field of pain management have extensive training regarding pain control in different settings, including oncology. Adding pain management into the equation benefits the patient's perception of rounded holistic care from a specialist [3]. They aim to reduce morphine milligram equivalence, widespread opioid use, and possible associated risks from utilizing such modalities. The benefit of shared decision-making, discussion of benefits, risks, and limitations of chronic opioid use must be at the forefront of the patient and provider discussions [1].
Risk assessment
By offering integrated care, including pain specialists, a risk assessment to identify medications that offer significant concerns with fatal and nonfatal opioid incidences can be offered. According to the Center for Disease Control and Prevention (CDC) (2020), "70% of the 67,367 deaths in 2018 involved an opioid". The CDC describes specific recommendations while prescribing opioid medication, to include initiating or continuing opioids for chronic pain, suggestions follow-up, and discontinuation of opioid therapy, assessing risk, and addressing harms of opioid use. Specific risks and benefits while co-prescribing benzodiazepines and opioids need to be discussed with patients of risks and benefits of this conjunct (CDC, 2020).
Morphine Milligram Equivalence (MME)
Morphine milligram equivalence has not been discussed during research regarding this topic. MME is not a standard evaluation done by oncology services when prescribing opioids. To provide narcotic pain management with decreased risks, providers should evaluate MME to decrease fatal overdose risks (CDC, 2020).
Illicit drugs use
One barrier to pain management referral includes illicit drug use, such as marijuana. Pain management requires a urine drug screen when opioids are prescribed. Illicit drugs within urine require automatic discontinuation of opioids and dismissal from a pain management program. Fear of violation of narcotic contracts will make patients hesitant to make pain management referrals [3]. When the oncologist is prescribing narcotics, the oncology patients do not typically sign contracts or do urine drug screens. Pain management specialists ensure patients are aware of the requirement of illicit drugs non-use when prescribing opioids and evaluating the risk. According to Zoberi et al., (2018) [3], an open discussion should be had during the referral process. Education provided to the oncology patient about safety and risks regarding the combination of dual medications could help alleviate these concerns, thus breaking the barrier.
Inadequate knowledge among health professionals that will influence pain management has been identified as one of those barriers. Oncologists have working knowledge in pain management. Identifying referrals from oncology to pain management is unclear, as each oncologist has been trained differently. An automatic referral trigger would help in identification, screening, and eligibility processes.
Project Design
The patients completed a BPI during their initial consult with pain management, and with each subsequent visit. Comparisons were made between the responses provided within the context of this tool and trended from the initial consult to distinguish if the pain management specialist had added benefit to their care. If pain management added to the team-approached care is successful, the quality initiative pilot will advance to implantation phase. Developing a nurse driven protocol for referral to pain management an automatic process would be the overall quality improvement project.
Setting and Resources
The pilot study for this quality improvement project was conducted in Aspirus, Wisconsin, which is a rural community home to approximately 11,000 individuals. The Langlade Pain Management and Aspirus Langlade Oncology Clinic were the primary sites of collaboration and facilitation. Of note, patients who seek care in both clinics may come from other communities in Northern Wisconsin.
Study Population
With the assistance of medical and radiation oncologists, patients from Aspirus Langlade Oncology Clinic were chosen to participate in this quality improvement project with the following inclusion criteria:
1. Alert and oriented to person, place, time, and situation. Must be their own person and able to make independent medical decisions without an activated power of attorney for healthcare.
2. Undergoing active treatment with chemotherapy and/or radiation therapy
3. Have active cancer diagnosis(es) made through an oncology provider 4. Have had at least three follow-up appointments with medical oncology.
4. Discussion of pain management at those visits was documented by a physician.
Sources of Data
Brief Pain Inventory (BPI) (Short Form) pain diary includes the intensity of pain, type of pain, time of distress, site of pain, and activity at the time of pain. The BPI has been validated and the copyright is held by Dr. Charles S. Cleveland (1991). Permission is not needed to use the U.S. federal government created measures.
Data Analysis
Data was compiled through the survey method and BPI. The survey was filled out on initial consultation and each subsequent visit. Microsoft Excel for reported data to include each question with consult and follow up. Analyzing the data and trending to statistically to decide if early pain management changes patient outcomes regarding pain and other quality of life indicators.
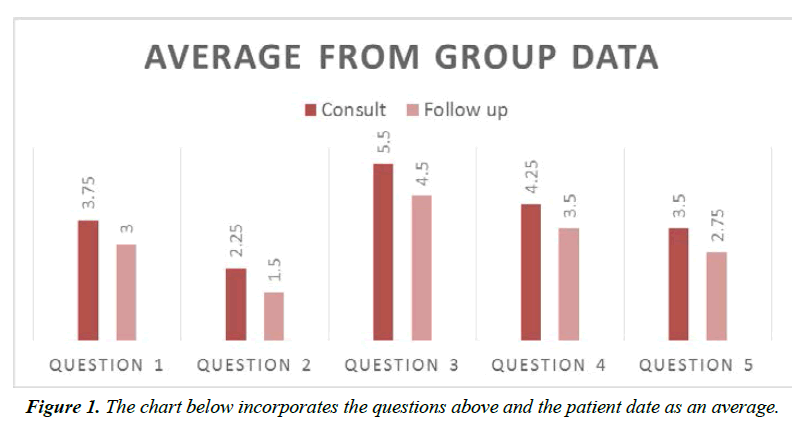
With the small number of participants in this quality improvement project, statistical interpretation was unfortunately limited. The average of the four patient’s responses on at consult and follow up are listed as the following:
1. Question number one: “Please rate your pain by circling the one number that best describes you pain on the average.”
2. Question number two “Please rate your pain by circling the one number that best describes your pain at its least in the last 24 hours.”
3. Question number three “Please rate your pain by circling the one number that best describes your pain at its worst in the last 24 hours.”
4. Question number four “Circle the one number that describes how, during the past 24 hours, pain has interfered with your sleep.”
5. Question number five “Circle the one number that describes how, during the past 24 hours, pain has interfered with your mood.” (Figure 1)
Limitations
Multiple unforeseen limitations occurred during this project. The first surge of the COVID-19 virus restricted the number of referrals to the project, especially within the cohort of immunocompromised patients. Mandates for screening upon entering the clinic may have swayed patients to opt out of making additional visits to a new provider specialty.
The geographical location of the clinic also posed as a challenge. Long distant commute of up to an hour away can be a barrier for many patients not only from a transportation perspective, but also potentially financially. Although the staff did their best to group appointments together, that did not always happen.
The limited study design, including at least three visits with oncologist that discussed pain, was a downfall. Early intervention is important, so waiting the total of threeappointment delayed referrals to pain management. Follow up was not consistent and patients may have started with consultation with or without follow up. The BPI form was not given out consistently to the consultations and follow up appointments as well [4-6].
Conclusion
Literature review and research has uncovered the benefits of adding pain management specialists to the plan of care for the oncology patient. Early referral to pain management offers many benefits to include managing untreated pain, breaking down the communication barrier, risk assessment regarding opioid use and non-opioid options, and adequate pain control using other modalities only offered by pain management. Central concepts regarding pain control include improved quality of life, decreased overall pain, and enhanced sleep quality. Thinking outside the box and looking for solutions when other first and second-line treatments have failed is important to the patients and their families. Providing the oncology population with early referrals to pain management clinics will make a difference in their life as having options available quickly is important.
Author’s Note
No conflicts of interest to disclose. Correspondence concerning this article should be addressed to Michelle L. Hulman, College of Graduate Nursing, University of Wisconsin at Oshkosh, 800 Algoma Boulevard, Oshkosh, WI 54901.
Author’s Contributions
M. Hulman was involved in literature review, study design, data collection, data analysis, and writing the manuscript. DNP Scholarly Project Chair and editor: Molly Schumacher DNP, FNP-BC, University of Wisconsin at Oshkosh, Department of Nursing.
References
- McAuliffe Staehler TM, Palombi LC. Beneficial opioid management strategies: A review of the evidence for the use of opioid treatment agreements. Subst Abuse. 2020;41(2):208-15.
- Abd-Elsayed A, Schiavoni N, Sachdeva H. Efficacy of spinal cord stimulators in treating peripheral neuropathy: a case series. J Clin Anesth. 2016;28:74-7
- Zoberi K, Everard K. Teaching chronic pain in the family medicine residency. Family Med. 2018;50(1):22-7.
- Cowperthwaite SM, Kozachik SL. Improving the Pain Experience for Hospitalized Patients with Cancer. In Oncol Nursing Forum 2019;46(2).
- Chatterjee A, Nimje G, Jain PN. Referral pattern to a tertiary care cancer pain clinic in India. Pain Palliative Care Pharmacol. 2019;33(1-2):6-14
- Cleeland CS. The MD Anderson symptom inventory user guide. Houston, TX: The University of Texas MD Anderson Cancer Center. 2016.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref