Review Article - Journal of Biochemistry and Biotechnology (2023) Volume 6, Issue 2
The high incidence of sickle cell syndrome and its associated issues in children
Glory Bondula*Gitam Deemed University, Visakhapatnam, Andhra Pradesh, India
- *Corresponding Author:
- Glory Bondula
Gitam Deemed University
Visakhapatnam, Andhra Pradesh, India
E-mail: Glorybondula0@gmail.com
Received: 23-Feb-2023, Manuscript No. AABB-23-89924; Editor assigned: 25-Feb-2023, PreQC No. AABB-23-89924(PQ); Reviewed: 11-Mar-2023, QC No AABB-23-89924; Revised: 15Mart-2022, Manuscript No. AABB-23-89924(R); Published: 22-Mar-2023, DOI:10.35841/aabb-6.2.136
Citation: Bondula G. The high incidence of sickle cell syndrome and its associated issues in children. J Biochem Biotech 2022;6(2):136
Abstract
Sickle Cell Anaemia or Sickle Cell Disease as it is also known is a fairly common haematological disease which can be passed on from generation to generation. Up until the early half of the 20th century, the disease was somewhat obscure in the sense that while it was affecting individuals in substantial numbers, a clear diagnosis couldn’t be made. Dr. Herrick’s interaction with a patient of sickle cell anaemia and the subsequent case findings related to the same, introduced the world to the existence of a new disease, one which was prevalent in far off lands of Africa and Asia. The characteristic sickle like shape of the cells is seen as a response to physiological stress and is contributory to the onset of anaemia and hypoxia. There are various signs and symptoms of Sickle Cell Anaemia and these can aggravate and precipitate numerous sequlae. Upon observing the prevalence of the disease, we can observe a scattered distribution with African countries, India, Middle Eastern and Mediterranean countries showing greater number of cases. The first case of Sickle Cell Anaemia in India was reported in 1952. A large numbers of cases are seen in the central and coastal states of India and less than 5 age groups is most commonly affected with the disease. Onset of complications may be acute or chronic and are an indication of worsening of the condition. This review article aims to encapsulate and provide a brief overview of sickle cell anaemia with greater emphasis on the complications in children
Keywords
Sickle Cell, Anaemia, Prevalence, Complications, Children.
Introduction
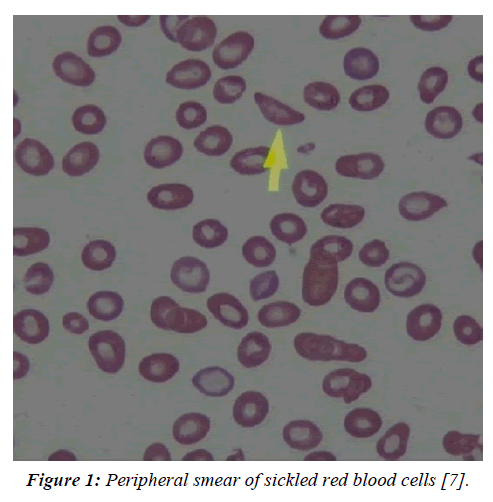
Sickle Cell Anaemia, which is alternatively also known as Sickle Cell Disease, is a genetic disorder (autosomal recessive). Those who are afflicted with the disease have an abnormality in their haemoglobin [1]. The anomaly in the haemoglobin is as a result of a point mutation wherein the purine adenine is replaced by a pyrimidine thymine corresponding to the sixth codon located on the beta globulin gene. Subsequently, valine replaces glutamic acid at the 6th position [2]. This causes the appearance of a haemoglobin tetramer Hbs which is mutated, in the erythrocytes of patients with sickle cell anaemia [3]. Delving into the origin of the disease leads to the year 1910, when an African American male of 20 years presented before Dr. James B. Herrick with respiratory symptoms. Upon blood examination, the presence of unusually shaped erythrocytes seemed to confound the physician [4]. Further studies in 1949, revealed that sickle cell anaemia is a molecular disease and under the influences of environmental stresses , the red blood cells possess the capacity to alter their shape from the normal biconcave to an abnormal sickled shape [5]. As a result of this sickling, the capacity of cells to carry haemoglobin is reduced and thus can lead to development of anaemia. Families belonging to areas which are endemic to malaria have greater possibility of possessing the sickle cell trait. The highest sickle cell trait (HbAS) carrier rate is present in families who trace their ancestry to malaria endemic regions. Most red blood cells have a life cycle lasting 120 days, but sickled red blood cells are different in that they last for only an approximate of 12-16 days [2]. Fatalities in the new born age group are most commonly attributed to either stroke or infection [6].
The reason for doing this review is to obtain knowledge and disseminate information regarding sickle cell anaemia from a public health point of view. Since Sickle Cell Anaemia is a highly common disease in India, it is all the more essential to ensure efforts made by the community at a grassroots level, and to achieve the same educating members of the society is imperative.
Objective
Through the means of this review article, we aim to provide an insight into the various trends pertaining to the prevalence as well as complications of this disease specifically in the children.
Mode of Inheritance
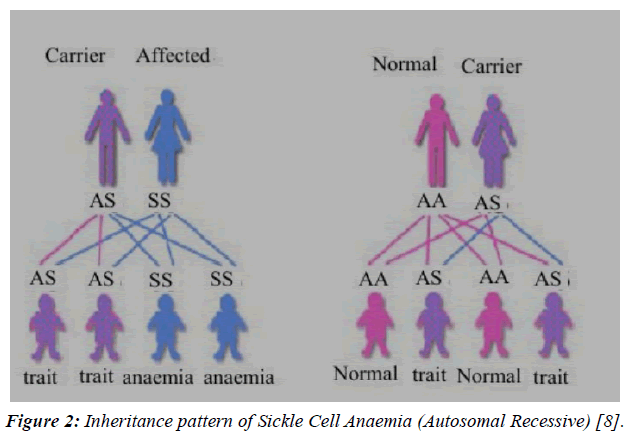
As shown in the above Figure 1 & 2, sickle cell anaemia follows an autosomal recessive pattern of inheritance. This implies, that in a hypothetical situation, wherein the father is a carrier (AS genotype) and the mother is afflicted by the disease (SS) there is an equal or 50-50 chance of the offspring acquiring the disease. Therefore half the children will have the trait for sickle cell anaemia while the remaining will remain as carriers, with the potential of transferring the disease to their offspring.
Figure 1: Peripheral smear of sickled red blood cells [7].
Figure 2: Inheritance pattern of Sickle Cell Anaemia (Autosomal Recessive) [8].
Conversely, while envisioning a situation where one of the parents is a carrier and other is normal, the probability of the children being carriers is 50%, with the remaining 50% being normal. Here, none of the children will be suffering from the disease.
Methodology
The official website of the World Health Organization as well as search engines like Public Health Medical Search, Google Scholar and other publication sites were searched, keeping the topic of prevalence and complications of sickle cell anaemia in mind. A myriad of MeSH terms were added which included: Sickle Cell Anaemia, Prevalence and complications. Textbooks of Pathology were also accessed in an attempt to garner further information about the topic while also enabling presentation of the matter in a cohesive fashion. To further build upon the creditability of this article, we have scoured through an extensive and comprehensive list of scientific research and reviews related to our topic. Appropriate bodies of work by eminent scientists and fellow members of the scientific community have also been included. A chronological list of the varied references has been added at the end of this review article.
Clinical Manifestations
Sickle cell anaemia can manifest in various forms. Some of the common manifestations include:
1) Anaemia – As is evident from the name of the disease itself, the most common symptom is anaemia which is usually chronic, extravascular and interspersed with episodes of aplastic crisis.
2) Vaso– occlusive crisis / phenomena – In the event of dehydration and/or deoxygenating, the red cells become sickled. These sickled cells will occlude or block the blood vessels. The obstruction to the blood flow will subsequently result in development of infarcts.
Infarcts are further sub classified into two groups based on their size.
A) (A) Micro infarcts – The most common sites which are affected are chest, abdomen, back along with joints. These can precipitate as recurring crises which are painful.
B) (B) Macro infarcts – The most common organ involved is Spleen. The pathological changes which can be seen in the spleen include sequestration and even auto splenectomy [9].
In children particularly, the occurrence of such bony crises is much more frequent. However, despite its’ common frequency it is difficult to distinguish the symptoms from those of osteomyelitis.
3) One particularly fatal example of vaso – occlusive crisis includes chest involvement. Presentations of Acute Chest Syndrome encompass symptoms including fever, chest pain and cough.
4) Systemically, tissue hypoxia can lead to impaired growth and development of young children. Even organ damage is witnessed as the disease progresses [10].
Prevalence of Sickle Cell Anaemia
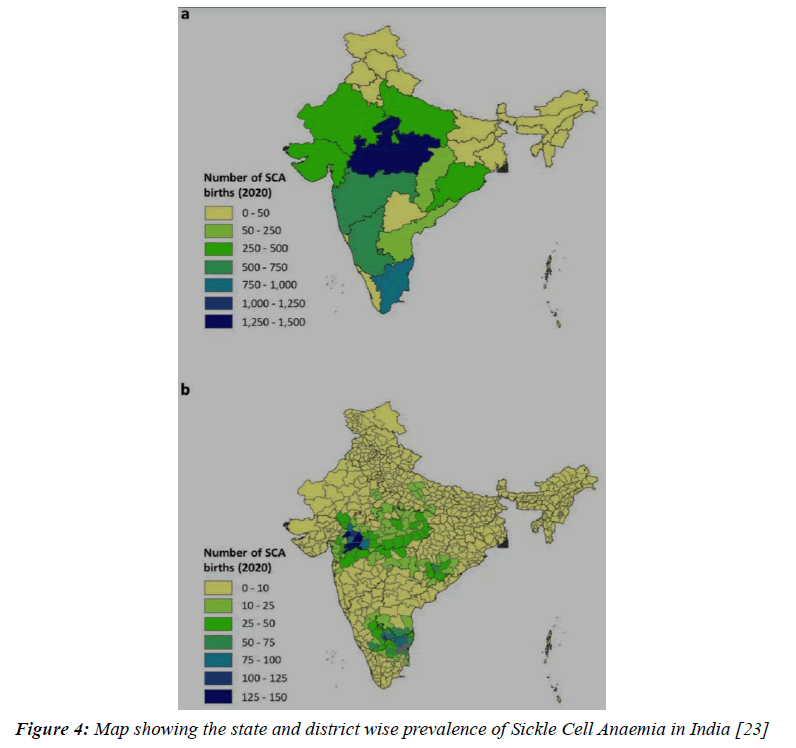
The correlation between race and prevalence of sickle cell anaemia has been made evident by the fact that certain races and ethnic groups have the homozygous trait for the disease in relatively larger numbers than others. Geographically , the areas associated with high prevalence of sickle cell anaemia consist of countries belonging to Africa ( Nigeria , Ghana , Gabon , Uganda etc. ), Saudi Arabia , India and also the countries in Mediterranean region [11].
India’s tribal population accounts for about 8.6% of the country’s overall population. Those belonging to the scheduled tribes are interspersed across various states including, but not limited to Rajasthan, Gujarat, Maharashtra, Madhya Pradesh, Chhattisgarh, Odisha, Jharkhand, West Bengal, Andhra Pradesh and Karnataka [12,13].
In the year 1952, Hermann Lehman, a physicist and biochemist, along with Marie Cutbush highlighted the presence of individuals containing the haemoglobin associated with sickle cell anaemia, in the hills of Nilgiri, Tamil Nadu [14]. This evidence was further complemented by Dunlop and Mazumdar, who conducted studies in north eastern state of Assam and found HbS in workers from Bihar and Odisha [15].
When speaking of the paediatric age group, the most common genetic haematological disease with which children are inflicted is sickle cell anaemia [16]. The worldwide prevalence with respect to various age groups doesn’t show much variation and higher incidence rates in children are seen in the aforementioned geographical regions. In the continent of Africa, which has the highest number of cases, the mortality and morbidity rate is staggering [17-19].
With the locus of Sickle Cell Anaemia being found in Central India, with special emphasis on Vidarbha region, it comes as no surprise that prevalence of this disease lies anywhere between a meagre 4% to an astonishing 40 %(18).In India, studies conducted in the central state of Chhattisgarh revealed not only a high prevalence of patients, but also showed the importance of socio-economic status in occurrence of the same. Out of the tested participants, a whopping 79 % were residing in underdeveloped rural homes (19). Screening of new born in the southern districts of Gujarat revealed that the tribal ethnic groups are more likely to be afflicted with the disease, with the trait for sickle cell being highest in Warli tribe and disease being highest in Dhodia Patels [20]. In a study conducted in Nagpur, Maharashtra, screening of new-borns via a solubility test and subsequently liquid chromatography led to the conclusion that there is a high number of carriers as well as sufferers of the disease [21]. In the cities and districts of Central and Western India, the Sindhi community is also prone to Sickle Cell Anaemia and other haemoglobinopathies [22,23].
Complications of Sickle Cell Anaemia
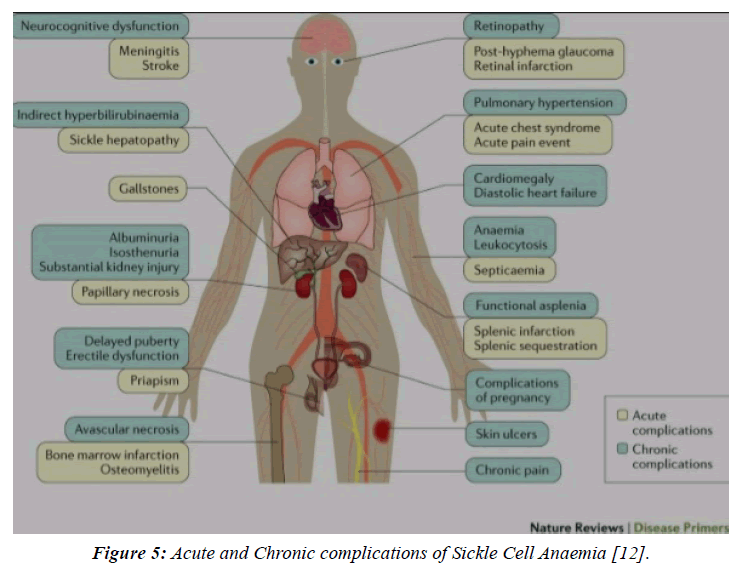
Just how there is a myriad of manifestations associated with this disease, so is there the threat of complications. These complications may range from seemingly minor inconveniences to potentially fatal ones. Majority of these complications set in during the primordial years. However, symptoms of a chronic nature are mostly noticeable in the later stages of life. Some of the most frequently observed ramifications include episodic vaso-occlusive crises, chronic pulmonary hypertension and acute chest syndrome, to name a few [24]. A study conducted by Mohanty et al. confirmed a relation between occurrence of vaso-occlusive crisis and seasonal variation. Higher incidence of the crisis is seen in monsoon, and then winter [25]. Vaso-occlusive crises are particularly dangerous and even possess a direct relationship with standard and quality of life [26].
Delving further into the systemic complications, we can observe that in the central nervous system, complications include, but are not limited to silent cerebral ischemia, stroke (which could be haemorrhagic or ischaemic) and thrombosis of the cerebral venous sinus [27]. Roughly 6 to 17 % of juvenile population across the globe falls prey to stroke after acquiring sickle cell anaemia [28].Though stroke can strike at any time; it is mostly seen during the first 10 years of life, predominantly from 2 to 5 years [29]. There exists a variation even between the two types of stroke, with cases of the more common ischaemic stroke being reported in the first decade and haemorrhagic stroke making an appearance in the age group of 20 to 30 years (28).
In the respiratory system the most common sequlae is Acute Chest syndrome. As a consequence of the same, the pulmonary function test of patients is affected and progressively asthma can develop in such children [30]. In the excretory system, the kidneys are the organs most likely to be affected. Micro albuminuria precedes any other symptom and if it remains unchecked, can even lead to severe damage to the kidneys. Other nephrological manifestations involve nephrotic syndrome and glomerulosclerosis [31]. Ocular complications include sickle cell retinopathies which if allowed to progress may even lead to blindness. Iris atrophy [32] is another indicator which is useful in diagnosis as is hyphema and secondary glaucoma [33].
Treatment
Owing to the numerous health related advantages, Hydroxyurea may be thought of as an essential mode of treatment for Sickle Cell Anaemia [34]. A study conducted by Quarmyne and others, revealed the effectiveness of the drug on young children with positive results being observed with respect to incidence of painful crises and subsequent hospitalization [35]. However, with advantages come disadvantages and Hydroxyurea is absolutely contraindicated in pregnancy. Additionally, leukopenia can also emerge as a unforeseen complication (Figures 3-5).
Figure 3: Worldwide prevalence of Sickle Cell Anaemia [12].
Figure 4: Map showing the state and district wise prevalence of Sickle Cell Anaemia in India [23]
Figure 5: Acute and Chronic complications of Sickle Cell Anaemia [12].
Other medicines which can be prescribed include [36] –
(1) Voxelotor – This is a new drug which has been introduced by the Food and Drug Administration of the United States of America, and has been approved for all over the age of 12 years. The route of administration is oral and the mechanism of action involves prevention of sickling coupled with reduced fragmentation. The disadvantages of this drug which prevent it from being the ideal drug of choice comprise of nausea, headache, pain in the abdomen, fever and others. Anaphylactic reactions may also be seen.
(2) Crizanlizumab– tmca– The continual search for medicinal treatment of sickle cell anaemia has resulted in introduction of another new medicine, this time with the ideal mode of administration being intravenous. Plausible side effects consist of fever, joint pain and back pain.
(3) Penicillin– The probability of a severe secondary infection due to pneumococci may be decreased after taking a prescription of penicillin tablet twice daily. Tablets should only be provided to elder children and in case of newborns we can give liquid penicillin. The duration of course of medication is variable and differs from physician to physician. On one end of the spectrum, treatment is stopped before a child’s 5th birthday while on the other, lifelong prescription has been advised.
Transfusions [36]
Transfusions are another alternative option and are of many types. Some of the more commonly employed are enlisted as follows –
(1) Acute transfusion – These are of prime importance in treating complication as and when they arise especially in case of stroke.
(2) Red Blood Cells Transfusion – This type of transfusion is carried out in attempt to replace the pre-existing sickled cells by fresh blood cells which have greater flexibility and can better respond to ordinary environmental stresses.
(3) Regular Transfusions – These transfusions are held periodically with the of preventing onset of complications like stroke and are even useful as a substitute to Hydroxyurea in the event of development of complications due to the latter.
Transplant [36]
Despite bone marrow and blood transfusion being considered as the epoch of all the available cures, the procedure is not a bed of roses. Unpleasant obstacles may spring up in the form of inappropriate age, wherein the patient is too old for carrying forward the transplant or in the unavailability of suitable donor.
There is a high success percentage of transplant and the greater the compatibility between human leukocyte antigens, the greater is the chance of patient survival. Unfortunately, complications like anaphylaxis and infections may appear which are grouped under the umbrella of Graft versus Host reactions.
Gene therapy [36]
In recent times the importance of gene therapy has increased as a useful tool in combating the effects of sickle cell anaemia and providing respite from the same.
Discussion
Based on the review findings, we can see that sickle cell anaemia is a disease that has widespread prevalence. Most of the countries in Africa particularly the western and sub Saharan countries like Nigeria have very high prevalence of the disease. Meanwhile countries in the same continent can have different rates of incidence. An example of this is Asia, wherein majority of the continent is not too greatly affected by the disease but for India and Middle Eastern countries. When speaking of India, the disease is spread over a multitude of states with Madhya Pradesh on pole position followed closely by Tamil Nadu, Maharashtra, and Karnataka. The age group which is most susceptible to procuring sickle cell anaemia is 0 to 5 years, with the average age being close to about 2 years [37]. The numerous sequalae which may appear as a result of increase in severity of disease affect nearly every system [38-43] of the body and if not nipped in the bud initially can have vastly debilitating effects that can eventually culminate in mortality.
Conclusion
At the end of this review article, we have been able to arrive at the conclusion that sickle cell anaemia has scattered distribution. This implies that while certain parts of the world have shockingly high number of cases being reported, others have next to none. When talking about India, we see that the disease is endemic to various states. A breakdown of the number of cases reveals that majority of the cases are reported in the scheduled caste and tribes, as well as the Sindhi community. Based on the socio- economic status, an overwhelmingly large number of afflicted individuals belong to rural areas as compared to urban. Neurological complications take precedence among other systemic complications and stroke is the most common of the lot. Despite the numbers which seem to startle us, hope still persists that someday in the near future efficacious treatment which can not only prolong the life span if such individuals but also improve their quality of living.
References
- Alkot M, Almaghrabi WA, Al-Najdi N, et al. Prevalence of complications of sickle cell disease at Makkah Al-Mukaramah, Saudi Arabia, 2017. Ann Clin Lab Res. 2018;6(1):226.
- Meier ER, Miller JL. Sickle cell disease in children. Drugs. 2012;72:895-906.
- Sundd P, Gladwin MT, Novelli EM. Pathophysiology of sickle cell disease. Annual review of pathology: mechanisms of disease. 2019 Jan 24;14:263-92.
- Herrick JB. Peculiar elongated and sickle-shaped red blood corpuscles in a case of severe anemia. Archives of internal medicine. 1910 Nov 1;6(5):517-21.
- Pauling L, Itano HA, Singer SJ, et al. Sickle cell anemia, a molecular disease. Science. 1949 Nov 25;110(2865):543-8.
- Miller ST, Sleeper LA, Pegelow CH, et al, Kinney TR. Prediction of adverse outcomes in children with sickle cell disease. New England Journal of Medicine. 2000 Jan 13;342(2):83-9.
- Shafiq M, Ali N. Bone marrow necrosis–initial presentation in sickle cell anemia. The American Journal of Case Reports. 2013;14:416.
- Urade BP. Incidence of sickle cell anaemia and thalassaemia in central India. Open Journal of Blood Diseases. 2012 Dec 5;2(04):71.
- Mohan H. Textbook of pathology. Jaypee brothers Medical Publishers; 2015.
- Robbins, Cotran. Pathologic Basis Of Diseases, South Asia Edition. (9th ed.). New Delhi: RELX India Private Limited ;2018.
- World Health Organization. Sickle-cell anaemia: report by the secretariat. InSickle-cell anaemia: report by the Secretariat 2005.
- Kato GJ, Piel FB, Reid CD, et al. Sickle cell disease. Nature reviews Disease primers. 2018;4(1):1-22.
- Colah RB, Mukherjee MB, Martin S, et al. Sickle cell disease in tribal populations in India. The Indian journal of medical research. 2015 May;141(5):509.
- Lehmann H, Cutbush M. Sickle-cell trait in southern India. British medical journal. 1952;1(4755):404.
- Dunlop KJ, Mozumder UK. The occurrence of sickle cell anaemia among a group of tea garden labourers in Upper Assam. The Indian Medical Gazette. 1952;87(9):387.
- Ware RE, de Montalembert M, et al. Sickle cell disease. The Lancet. 2017;390(10091):311-23.
- Sack FN, Njangtang DM, Chemegni BC, et al. Prevalence of sickle cell disease in newborns in the Yaounde Central Hospital. J Med Res. 2017;3:277-9.
- Balgir RS. The burden of haemoglobinopathies in India and the challenges ahead. Current science. 2000 Dec 10:1536-47.
- Mishra H, Neralwar A. Prevalence of Sickle Cell Disease Among School-age Children in Chhattisgarh, India: Predictions, Implications and Interventions. Journal of Health Management. 2019;21(4):601-11.
- Italia Y, Krishnamurti L, Mehta V, et al. Feasibility of a newborn screening and follow-up programme for sickle cell disease among South Gujarat (India) tribal populations. Journal of medical screening. 2015;22(1):1-7.
- Jain DL, Sarathi V, Upadhye D, et al. Newborn screening shows a high incidence of sickle cell anemia in Central India. Hemoglobin. 2012;36(4):316-22.
- Bhanvadia VM, Chavda A, Mehta D, et al. Study of prevalence of hemoglobinopathy in Sindhi community of Jamnagar, Gujarat: A pilot study. International Journal of Medicine and Public Health. 2015;5(4).
- Hockham C, Bhatt S, Colah R, et al. The spatial epidemiology of sickle-cell anaemia in India. Scientific reports. 2018;8(1):17685.
- Mehta SR, Afenyi-Annan A, Byrns PJ, et al. Opportunities to improve outcomes in sickle cell disease. American family physician. 2006;74(2):303-10.
- Mohanty D, Mukherjee MB. Sickle cell disease in India. Current opinion in hematology. 2002 Mar 1;9(2):117-22.
- McClish DK, Penberthy LT, Bovbjerg VE, et al. Health related quality of life in sickle cell patients: the PiSCES project. Health and quality of life outcomes. 2005;3(1):1-7.
- Farooq S, Testai FD. Neurologic complications of sickle cell disease. Current neurology and neuroscience reports. 2019;19:1-8.
- Powars D, Wilson B, Imbus C, et al. The natural history of stroke in sickle cell disease. The American journal of medicine. 1978;65(3):461-71.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood, The Journal of the American Society of Hematology. 1998;91(1):288-94.
- Chen L, Gong J, Matta E, et al. Pulmonary disease burden in Hispanic and non‐Hispanic children with sickle cell disease. Pediatric pulmonology. 2020;55(8):2064-73.
- Tejani A, Phadke K, Adamson O, et al. Renal lesions in sickle cell nephropathy in children. Nephron. 1985;39(4):352-5.
- Acheson RW, Ford SM, Maude GH, et al. Iris atrophy in sickle cell disease. British journal of ophthalmology. 1986;70(7):516-21.
- Goldberg MF. The diagnosis and treatment of secondary glaucoma after hyphema in sickle cell patients. American journal of ophthalmology. 1979 Jan 1;87(1):43-9.
- Singh A, Xu YJ. The cell killing mechanisms of hydroxyurea. Genes. 2016;7(11):99.
- Quarmyne MO, Dong W, Theodore R, et al. Hydroxyurea effectiveness in children and adolescents with sickle cell anemia: a large retrospective, population‐based cohort. American journal of hematology. 2017;92(1):77-81.
- https://www.nhlbi.nih.gov/health-topics/sickle-cell-disease
- Chukwu BF, Ezenwosu OU, Eke CB, et al. What factors influence the age at diagnosis of sickle cell anemia in Enugu, Nigeria. J Blood Disord Transf. 2014;5:233.
- Garikapati A, Kumar S, Chaturvedi A, et al. Pseudocyst of pancreas, rare crisis in sickle cell disease. J Evolution Med Dent Sci. 2020;9:2072-3.
- Garikapati A, Kumar S, Chaturvedi A, et al. Pseudocyst of pancreas, rare crisis in sickle cell disease. J Evolution Med Dent Sci. 2020;9:2072-3.
- Panjwani V, Daigavane S, Acharya S, et al. Sickle Cell Retinopathy (SCR) in a Patient with Sickle Cell Trait--A Rare Case Report. Journal of Evolution of Medical and Dental Sciences. 2020;9(28):2016-9.
- Pratapa SK, Acharya S, Gupte Y, et al. Acute B Virus Hepatitis with Fulminant Hepatic Failure Precipitating Crisis in Sickle Cell Disease.
- Pareek A, Khandekar A, Acharya S, et al. Correlation between nephropathy and ophthalmic complications in cases of sickle cell anemia: an entangled association. Indian Journal of Medical Specialities. 2019;10(2):72.
- Verghese B, Acharya S, Khandekar A, et al. Clinical profile of patients of sickle cell crisis in a rural tertiary care hospital. Journal of Evolution of Medical and Dental Sciences-JEMDS. 2019;8(42):3114-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref