Review Article - Journal of Public Health and Nutrition (2023) Volume 6, Issue 4
The effect of peppermint oil supplementation on cardiometabolic indices and other health related outcomes: A two arm placebo randomised controlled trial.
Heidi E Murray*
Department of Nutrition, University of Central Lancashire, Preston, Lancashire, United Kingdom
- Corresponding Author:
- Heidi E Murray
Department of Nutrition,
University of Central Lancashire,
Preston,
Lancashire,
United Kingdom
E-mail: heidimurray28@gmail.com
Received: 22-Apr-2023, Manuscript No. AAJPHN-23-96779; Editor assigned: 24-Apr-2023, AAJPHN-23-96779 (PQ); Reviewed: 08-May-2023, QC No. AAJPHN-23-96779; Revised: 30-Jun-2023, Manuscript No. AAJPHN-23-96779 (R); Published: 07-Jul-2023, DOI:10.35841/aajphn.6.4.156
Citation: Murray HE. The effect of peppermint oil supplementation on cardiometabolic indices and other health related outcomes: A two arm placebo randomised controlled trial. J Public Health Nutr. 2023;6(4):1-11.
Abstract
Objectives: The effects of peppermint oil on gastrointestinal ailments are well-documented; however, the benefits of peppermint oil on cardiometabolic indices are not well researched. Therefore, the present investigation examined the effects of 20 days of peppermint oil supplementation on cardiometabolic indices and other health related outcomes.
Methods: In a randomised, single blind, placebo controlled trial, 10 participants (31.70 ± 15.51; 5 M/ 5 F), consumed a peppermint oil supplement or placebo (PLA) for 20 days. Anthropometric, energy expenditure and substrate oxidation measurements as well as haematological measurements, blood pressure, resting heart rate and questionnaires were measured pre and postsupplementation.
Results: There were no statistically significant differences (p>0.05) for systolic or diastolic blood pressure. In addition, there were no statistically significant differences (p>0.05) for any of the haematological values or resting heart rate. Although, V’O2 and V’CO2 at moderate intensity exercise were significantly worse with peppermint oil intake (pre: V’O2=0.89 L/ min and V’CO2=0.66 L/min; post: V’O2=0.0.73 L/min and V’CO2=0.66 L/min) compared to placebo (pre: V’O2=0.75 L/min and V’CO2=0.78 L/min; post: V’O2=0.91 L/min and V’CO2=0.78 L/min). Moreover, psychological well-being indices measured using the beck depression inventory, state trait anxiety inventory and COOP WONCA had no statistical difference in the peppermint group compared to placebo.
Conclusion: A novel peppermint oil supplementation protocol designed for sustained improvement in cardiometabolic and other health related outcomes failed to provide any apparent advantages. The supplement is a safe and affordable treatment capable of potentially providing benefits in the long term but requires more extensive investigation.
Keywords
Gastrointestinal ailments, Oil supplementation, Extensive investigation, Cardiometabolic, Haematological values
Introduction
Cardiometabolic health is a spectrum of various conditions which impact a considerable proportion of society, consequently resulting in the leading cause of global mortality. Symptoms that can be used to identify cardiometabolic health concerns comprising of obesity, insulin resistance, hypertension, atherogenic dyslipidemia, low high density lipoproteins, high triglycerides, high levels of adiposity, high body mass index, large waist to hip ratio and poor glucose regulation [1-3]. Cardiometabolic disorders are a result of biological, demographic, dietary, behavioural and environmental factors with the most common causes; being an unhealthy lifestyle and diet, physical inactivity and smoking. Pharmaceutical methods of treatment are widely used but it is becoming increasingly more common to explore the benefits of manipulating dietary intake to enhance cardiometabolic health [4-6].
Peppermint oil is a herbal extract from peppermint leaves which is a natural combination of water mint and spearmint. As a member of the labiatae family, peppermint oil is alongside many other commonly used medicinal essential oil plants, such as spearmint, lavender and rosemary. Given the increased research and knowledge of the benefits of peppermint oil, ‘mint essential oils market size’ expects the annual growth rate of mint essential oils globally to increase by 9.2% from 2019 to 2025 [7]. Peppermint oil is thought to have spasmolytic properties and subsequently positive health benefits. The supplement can be universally purchased across the counter making it accessible and affordable for the wider population.
Literature Review
Peppermint oil is widely available and affordable but there is limited research on the cardiometabolic outcomes of peppermint oil supplementation. The leaves of the peppermint contain several flavonoids, with main components primarily eriocitrin, luteolin and hesperidin which consequently gives the supplement antioxidant properties. Eriocitrin specifically was found in a study by Ferreira, et al. that even at low doses of 25 mg/kg resulted in significant metabolic, inflammatory and oxidative stress improvements. With peppermint oil possessing levels of eriocitrin that consisted of a concentration range of 6%-15%, it promotes the desire for performing additional research to see if there are parallel benefits with a peppermint oil supplementation protocol [8-10].
Peppermint oil has been found to have the ability to act as an antagonist to calcium which results in a spasmolytic effect in the gastrointestinal tract. The use of peppermint oil as a treatment method for abdominal ailments dates back to ancient Egypt, Greece and Rome. Where natural and cost effective remedies were used then, there is still a market for them now so research needs to clarify if peppermint oil is a potential method for cardiometabolic disease management and prevention. The aroma of peppermint has been found to be effective on perceived physical workload, temporal workload, effort and anxiety [11].
Research on peppermint spirits inhalation has been conducted on women following a caesarean section (n=35). A total of 22 participants completed the peppermint spirits inhalation intervention whilst eight performed a placebo inhalation [12]. An additional five completed standard antiemetic therapy. The results found that there were a greater proportion of participants in the peppermint spirits group who had no nausea or only slight nausea at 2 minutes vs. placebo 14 (63.6% vs. 0 and vs. standard antiemetics (0). Whilst this study is focusing on peppermint spirit inhalation rather than an oral supplement, it provides confidence that there were positive effects of peppermint to explore in greater detail.
One of the few studies which directly looked at cardiometabolic indices with peppermint oil supplementation and therefore carries significant weight in the benefits of peppermint oil was conducted by Barbalho, et al. They found that with daily supplementation of 20 g of peppermint in 200 ml of water, of the 25 participants, 41.5% showed a decrease in glycemia. The conclusion of the study was that peppermint oil can be efficient at controlling glycemia which is supported by past research utilising vegetables for glycemic control [13]. In addition to this, the study found that 66.9% presented a decrease in total cholesterol levels following the study, with 58.5% having a decrease in triacylglycerol rates and 52.3% in LDL-c indices.
However, 52% presented an increase in HDL-c indices. A key finding from the study was that blood pressure was reduced in 52.5% of the participants which supports the hypothesis that peppermint oil can be positively used to lower blood pressure [14].
There is significant evidence to support that a higher VO2max has a positive correlation with decreased risk in the incidence of a number of lifestyle related diseases, primarily cardiovascular diseases. Although VO2max is not directly measured in this study, predictions can be made based on pulmonary oxygen uptake (V’O2) levels. This study analysed V’O2 values both at rest and during moderate intensity exercise. An increased V’O2 predicts the body’s increased efficiency at producing work. Meamarbashi and Rajabi performed a ten days peppermint oil supplementation protocol to investigate exercise performance changes. In twelve healthy male university students, the physiological parameters (spirometry and gas analysis showed that 0.05 ml of peppermint essential oil over ten days significantly improved V’O2 (L/min and V’CO2 (L/min. The V’O2 improved by 10.5% between pre and post-test whilst V’CO2 improved by 21.1% [15-17]. Their findings strongly support the effectiveness of peppermint oil supplementation on the exercise performance, respiratory function variables, systolic blood pressure, heart rate and respiratory gas exchange parameters. Given the similarity in protocol to the current investigation, it is expected that tantamount results would be acquired during our study. With a longer duration of supplementation, it is possible that the findings may be of more significance and a greater difference [18].
The measurement of CO2 has seen vast advancements since first developed in approximately 1918 to analyse gas concentrations in mines. This data of significant value can now be efficiently gained with the use of the MetaLyser 3B system [19]. Minute ventilation to carbon dioxide output (V’E/V’CO2 slope) is the strongest death predictor before larger lung resections. Disturbances in the human body occur when the physiological systems cannot return fluctuations in CO2 levels to normal levels. In a state of stable CO2 production and ventilation, a change in V’CO2 represents metabolic and alveolar ventilation change. Cardiac output changes directly cause V’CO2 changes. On the contrary, V’CO2 decreases in the event of low cardiac output, shock and pulmonary embolism. When pulmonary embolism occurs, the CO2 gradient increases. An increase in V’CO2 can also be used as a predictor of fluid responsiveness and fluid resuscitation is the central method of managing patients who bear acute circulatory failure [20]. If acute circulatory failure is left untreated then this results in an imbalance of systemic venous return and cardiac function. Consequently this causes a decrease in cardiac output, resulting in a clinical syndrome of systemic organ insufficiency.
A randomised crossover study in 13 healthy volunteers compared 182 mg of peppermint oil vs. placebo with 50 mL water when in a fasted state, followed by a nutrient drink given via a pump over 60 minutes. Peppermint oil was found to decrease intragastric pressure (P<0.0001) and gastric motility index (P<0.05) during fasting but did not affect parameters during the nutrient drink or gastric accommodation. The peppermint oil was also found to reduce appetite vs. placebo during fasting. A within subjects design study involving a protocol in which participants completed a peppermint inhalation condition (administered every 2 hours) and a noninhalation condition for 5 days each. Participants rated their hunger level every two hours and completed a food diary listing of everything they consumed throughout the study. Participants were found to have consumed significantly fewer total calories, calories from saturated fat, total fat and sugar during the peppermint inhalation condition. Participants also rated their hunger level significantly lower during peppermint inhalation. A drop in weight may be an outcome of the 20 days protocol. These findings promote interest in understanding the complexity of the impact which peppermint oil has on the human anatomy.
Elevated blood pressure levels are an increasing issue globally with the number of associated deaths doubling to 1.2 billion across the world over the past three decades. In England alone, high blood pressure affects over 1 in 4 adults which highlight the urgency of establishing methods for reducing hypertension. Currently, a prevalent discussion is the topic of replacing antihypertensive medications with appropriate nutrition and nutraceutical supplements which are widely available and affordable. There is significant scientific literature to back up such strategies. In oral supplementation of peppermint, data has shown a reduction in heart rate and systolic blood pressure likely to be due to the ability to relax smooth muscle with peppermint oil supplementation via calcium channel blockade or direct enteric nervous system effects. Consequently there is a decrease in the likelihood of peristalsis. This can be beneficial in the ability to perform colonoscopies.
Menthol and peppermint extracts have been found to increase alertness in both those with an upper respiratory tract illness as well as healthy individuals due to the stimulating effect they have on the trigeminal nerve. There may be cardiometabolic effects as a result of the effects on cranial nerves but this is yet to be established through scientific research. White tea is considered to be the oldest form of tea but for the first time peppermint was added and tested to see any additional benefits. The findings suggested that the addition of peppermint added potential antibacterial and anti-inflammatory qualities.
Peppermint oil supplementation remains a relatively new avenue of research, with the quantities of peppermint oil supplementation unestablished. However, in a study that was placebo controlled on the tolerance of L-menthol, even single doses as high as 320 mg were highly tolerated. This is because the absorption rate was quick and approximately 70% was emitted via urine. It is expected that the same would occur with peppermint oil supplementation. The majority of the research analysing the rate at which peppermint oil is absorbed is predominately in rats making it hard to conclude the likelihood of seeing the same results in humans. A non-randomised study that looked at the same group of participants, pre and postsupplementation, had participants intake 50 μl of peppermint oil. They found positive cardiometabolic health outcomes in humans but further investigation is needed for a more comprehensive understanding.
In a controlled study on the efficacy of peppermint oil in diarrhoea predominant IBS, sixty five patients were randomly allocated to receive either peppermint oil or placebo three times daily for six weeks. Over two to three intervals throughout the study, changes in symptoms were monitored and then analysed by paired and unpaired ‘t’ tests. The observations at the conclusion of the six weeks of abdominal pain therapy were that there was a highly significant (p>0.001) improvement (mean ± SD) 4.94 ± 1.30 in the peppermint oil group compared with 6.15 ± 1.24 in the placebo group. Just two weeks after the end of the trials, the pain score again increased (6.09 ± 1.93) concluding that the peppermint oil was effective in relieving only abdominal pain in diarrhoea predominant IBS momentarily. It is possible that the same could be found for improvements in blood pressure and other cardiometabolic health related indices, but that they wouldn’t be long term.
There is pharmaceutical products currently widely prescribed containing peppermint oil. An example is Mintec; the gastro resistant capsule containing 0.2 ml peppermint oil is prescribed for symptomatic relief of irritable bowel or spastic colon syndrome. Before being approved for the market, pharmacokinetic properties were determined with an open cross over study. Menthol is the main component of peppermint oil. Therefore, the study was conducted on eight healthy volunteers; to compare the excretion pattern of menthol from peppermint oil contained in the Mintec capsules, as well as, uncoated capsules. In each leg of the study, each participant received 0.4 ml of peppermint oil as two capsules of one of the preparations. Over the next 24 hours, the excretion of the oil in the urine was monitored. Mintec capsules significantly delayed the rate of excretion of menthol compared with the non-coated capsules. Further products such as buscomint peppermint oil are available to patients that in supporting vivo studies state that peppermint oil appears to enhance the production of bile due to the choleretic and antifoaming effects of the antispasmodic action. Subsequently, the peppermint oil supplement helps to decrease abdominal distension, as well as discomfort and abdominal pain. The research will address a gap in non-pharmaceutical methods of improving cardiometabolic health and blood pressure.
Rationale
Cardiometabolic disease is the cause of death for 17.9 million people globally each year so it is imperative that research is conducted on any possible protocols which provide natural treatment or preventative methods for cardiometabolic disease. As aforesaid in the literature review, the research found on peppermint oil has been positive. Although it is known that peppermint oil can provide health benefits, there has not been sizable research on the effects of peppermint oil supplementation on blood pressure and other cardiometabolic health related indices. Given the overwhelming number of deaths caused by cardiometabolic health and the cost of the health services, a greater understanding of the effects of peppermint oil from this study provides health authorities with valuable clinical information.
Aim
The aim of this specific study was to investigate the influence of 20 days of twice daily, oral, peppermint oil supplementation on cardiometabolic and other health related indices in healthy adults compared to placebo. The primary objective of this randomised trial is to examine the influence of the peppermint oil oral supplement on systolic blood pressure relative to a placebo. Its secondary objectives are to assess if peppermint oil supplementation impacted other risk factors associated with and as a function of cardiometabolic disease.
Hypotheses
The research tests the hypothesis that it is to be expected that the primary outcome of the peppermint oil supplement group will acquire a reduction in systolic blood pressure compared to the placebo group. In addition, the secondary hypothesis tested is that the peppermint oil group will have data to support advances in cardiometabolic health parameters in comparison to the placebo.
Materials and Methods
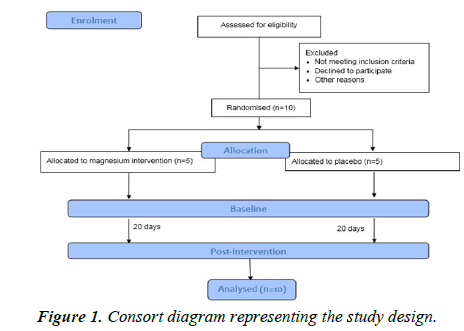
The research proposal was approved by the university of central Lancashire ethics, integrity and governance unit (ref: HEALTH 0016) through the school approval process on 1st February 2022. Informed consent was explicitly given throughout the research to all participants with written consent acquired at both baseline and follow-up testing, in accordance with the declaration of Helsinki and the Oviedo convention. All participants were over the age of 18 meaning it was not necessary for the consent of a parent or guardian to be obtained. This investigation exhibited a 20 days parallel, single blind (blinded to participant), randomised placebo controlled trial (Figure 1). The 20 days supplementation period has previously been published elsewhere and applied to this protocol. The protocol has been replicated from a recent study by Sinclair, et al.
The objective of the proposed research is to identify how a 20 days peppermint oil supplementation affects the risk factors associated with cardiometabolic indices. The research will be completed in a laboratory at the university of Central Lancashire collecting quantitative data in an observational study design. Potential participants were provided with the participant information sheet during recruitment to establish if they gave consent to take part in the study. If the participant met the eligibility criteria then they were invited to the exercise physiology laboratory in UCLan’s darwin building, for the initial testing.
On arrival at the laboratory, all participants were required to complete a PARQ form to eliminate any potential health risks in participating as well as a consent form. PARQ forms are common within this style of research to allow physicians to efficiently, effectively and safely establish if participants are safe to undergo the study with minimal risk. Participants were also required to complete questionnaires to give an extensive summary of their sleep quality and psychological well-being.
Anthropometric measures of mass (kg) using weighing scales and height using a stadiometer were collected in order to calculate the participant’s body mass index (kg/m2). Body fat percentage (%) was examined using a bioelectrical impedance analysis device. The final anthropometric measure collected was waist circumference and hip circumference allowing the waist to hip ratio to be calculated.
Throughout the laboratory data collection, a gas analysis system (MetaLyser 3B system, Cortex Biophysic, Leipzig, Germany) was used. Initially, the participant lay supine for 15 minutes and then resting heart rate, blood pressure, resting energy expenditure and substrate oxidation were gained. Following the collection of the resting values, participants walked on a treadmill (hp Cosmos Pulsar, Nussdorf, Germany) at a velocity of 4.5 km/h for 8 minutes. This walking velocity of 4.5 km/h was chosen as studies have shown this velocity is classified as a moderate exercise intensity. The data was then inputted into a password protected spread sheet for data analysis.
Following the exercise testing, capillary blood samples were collected by finger prick. Capillary triglyceride, total cholesterol and glucose levels (mmol/L) were obtained using handheld analysers and capillary haemoglobin levels (g/L using a single handheld analyser.
After the initial testing, the participants were given either a peppermint placebo to take one drop, twice a day, for 20 days or the peppermint sample. The supplement could be diluted with as much water as necessary. When the participant completed the retest, the participant was asked if they thought they had the sample or placebo and the researcher noted if they chose correctly or incorrectly. This allowed for confirmation of the fact that the sample used as the placebo was legitimate enough to be used for further research and provided validity to the data.
To ensure standardisation, where possible, the participants were booked in for their retest at the exact same time slot as the baseline measurements. This is in order to reduce the variability in baseline measurements from participants’ behaviour and environment ahead of testing and during data collection. This provides increased validity when detecting true effects with the relatively small sample size of ten participants. However, with limited lab availability this was unfortunately not always possible.
Duty of care was evident throughout with all risks explained on the risk assessment as well as any the participant needed to be aware of explained on the participant information sheet. The risks in this study were low risk and the value of the research offset any potential risks. All information collected from participants has been kept strictly confidential and only the investigators named in the ethics approval have access to the data. Electronic anonymised data has been stored on an encrypted folder via the UCLan network using Microsoft OneDrive and paper forms are kept in a locked drawer. The data will be securely stored for 5 years from the end of the study and then destroyed. Participants have been made aware of this and understood that they could withdraw at any point until the completion of data collection.
In order to be eligible for participation in the study, the participants had to be over 18 years of age and with no allergy to peppermint. In addition, they had to be a non-smoker, have a Body Mass Index (BMI) of less than 30, be injury free and not be diagnosed with any cardiometabolic or psychological diseases. Further exclusion criteria included pregnancy, exceeding 65 years of age, and any metabolic/uncontrolled hypertensive conditions. This mirrors the commonly used recruitment criteria.
The total sample size of this 20 days, parallel, single blind, placebo controlled trial was ten individuals in order to meet the desired confidence level, with an equal distribution of male and female participants selected to participate. Whilst this is not a strength or limitation, a heterogeneous sample have positive implications for how broadly findings may translate to the wider population. Upon exit of the post-test data collection, all participants were asked which liquid they thought they had been allocated in order to help calculate the blinding efficacy.
Results
Total trial completion numbers in each group were peppermint oil (n=5) and placebo (n=5), with 100% completion rate for both groups. Changes from baseline to 20 days in the experimental parameters were used to create binary variables, i.e. improve/did not improve for each participant. If p values have been reported, then it should be recognised that values which were close to but higher than 0.05 do not indicate a “trend” or statistical significance (Table 1).
| All | Placebo | Peppermint | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 31.70 | 15.51 | 23.40 | 1.14 | 40.00 | 19.18 |
| Mass (kg) | 72.00 | 11.85 | 78.92 | 9.41 | 65.08 | 10.39 |
| Height (m) | 1.73 | 9.34 | 1.77 | 9.99 | 1.69 | 7.39 |
| BMI (kg/m2) | 23.87 | 2.43 | 25.04 | 1.28 | 22.70 | 2.87 |
| Sex (m/f) | 5/5 | 2/3 | 3/2 | |||
Table 1. Baseline characteristics of 16 completed study participants.
Of the 10 participants that completed the trial, 60% (n=6 correctly identified their designated trial arm and the chisquared test showed that the test sample was significant X2 significant X2 (1)=4.00, p<0.05, indicating that an effective blinding strategy was adopted (Table 2).
| Placebo | Peppermint | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Mass (kg) | 78.90 | 9.41 | 78.64 | 8.75 | 65.08 | 10.39 | 65.06 | 10.56 |
| Body fat (%) | 26.04 | 6.96 | 24.88 | 7.25 | 26.22 | 4.45 | 25.9 | 4.75 |
| BMI (kg/m2) | 23.88 | 2.42 | 25.02 | 1.23 | 22.67 | 2.85 | 22.70 | 2.97 |
| Waist circumference (m) | 86.10 | 6.56 | 86.00 | 6.78 | 104.7 | 6.14 | 104.8 | 5.63 |
| Waist: Hip ratio | 0.83 | 0.07 | 0.82 | 0.07 | 0.86 | 0.05 | 0.82 | 0.74 |
Note: No statistically significant differences (p>0.05) in anthropometric parameters were found.
Table 2. Anthropometric measures as a function of each trial arm.
No statistical differences (p>0.05) in V’O2 at rest were found. V’O2 at moderate intensity exercise (95% CI=0.49-0.13), t=4.02, p=0.004, ηp²=0.67) significantly decreased in the peppermint oil arm compared to placebo.
No statistically significant differences (p=0.051) in V’CO2 at rest were found (Table 3). V’CO2 at moderate intensity exercise ( 95% CI=0.07-0.47), t=3.07, p =0.015, η p²=0.47) significantly decreased in the peppermint oil arm compared to placebo.
| Placebo | Peppermint | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Rest | ||||||||
| V’O2 (L/min) | 0.24 | 0.05 | 0.33 | 0.65 | 0.31 | 0.07 | 0.25 | 0.08 |
| V’CO2 (L/min) | 0.22 | 0.05 | 0.31 | 0.07 | 0.30 | 0.06 | 0.24 | 0.08 |
| Carbohydrate oxidation (g/min) | 0.25 | 0.05 | 0.33 | 0.11 | 0.34 | 0.06 | 0.28 | 0.10 |
| Fat oxidation (g/min) | 0.02 | 0.01 | 0.03 | 0.03 | 0.02 | 0.02 | 0.02 | 0.01 |
| % carbohydrate | 83.65 | 1.59 | 79.58 | 15.08 | 88.35 | 7.72 | 87.60 | 9.75 |
| % fat | 16.35 | 1.59 | 20.42 | 15.08 | 11.65 | 7.72 | 12.40 | 9.75 |
| Total kcal/min | 1.18 | 0.27 | 1.62 | 0.33 | 1.56 | 0.36 | 1.26 | 0.39 |
| Resting metabolic rate | 1695.67 | 384.30 | 2392.22 | 482.24 | 2239.44 | 512.16 | 1816.71 | 567.14 |
| Moderate intensity exercise | ||||||||
| V’O2 (L/min) | 0.75 | 0.08 | 0.91 | 0.05 | 0.89 | 0.13 | 0.73 | 0.09 |
| V’CO2 (L/min) | 0.78 | 0.07 | 0.78 | 0.07 | 0.66 | 0.11 | 0.66 | 0.11 |
| Carbohydrate oxidation (g/min) | 0.57 | 0.24 | 0.59 | 0.17 | 0.83 | 0.11 | 0.64 | 0.25 |
| Fat oxidation (g/min) | 0.15 | 0.08 | 0.22 | 0.05 | 0.11 | 0.06 | 0.11 | 0.07 |
| % carbohydrate | 61.51 | 25.54 | 53.97 | 11.99 | 77.29 | 10.76 | 70.88 | 19.80 |
| % fat | 38.49 | 25.54 | 46.03 | 11.99 | 22.71 | 10.76 | 29.12 | 19.80 |
| Total kcal/min | 3.64 | 0.44 | 4.36 | 0.28 | 4.35 | 0.58 | 3.57 | 0.50 |
| Energy expenditure (kcal/min) | 3.64 | 0.44 | 4.36 | 0.28 | 4.35 | 0.58 | 3.57 | 0.50 |
Table 3. Energy expenditure and substrate oxidation measurements as a function of each trial arm.
No statistical differences (p>0.05) in carbohydrate or fat oxidation at rest or moderate intensity exercise were found. No statistical differences (p>0.05) in percentage carbohydrate or fat at rest or moderate intensity exercise were found. No statistical differences (p>0.05) in RMR were found. No statistical differences (p>0.05) in haematological values were found (Table 4).
| Placebo | Peppermint | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Cholesterol (mmol/L) | 3.70 | 0.29 | 3.56 | 0.08 | 3.54 | 0.89 | 3.50 | 0.00 |
| LDL (mmol/L) | 2.11 | 0.36 | 1.99 | 0.11 | 1.97 | 0.12 | 2.00 | 0.09 |
| HDL (mmol/L) | 1.22 | 0.11 | 1.21 | 0.06 | 1.22 | 0.09 | 1.17 | 0.07 |
| Total: HDL ratio | 3.06 | 0.49 | 2.93 | 0.17 | 2.91 | 0.19 | 3.01 | 0.18 |
| LDL: HDL ratio | 1.76 | 0.46 | 1.65 | 0.16 | 1.62 | 0.19 | 1.72 | 0.18 |
| Glucose (mmol/L) | 4.84 | 0.50 | 4.74 | 0.65 | 4.32 | 0.29 | 4.70 | 0.60 |
| Triglycerides (mmol/L) | 1.20 | 0.32 | 1.18 | 0.16 | 1.20 | 0.25 | 1.04 | 0.21 |
| Haemoglobin (g/L) | 142.00 | 56.66 | 148.40 | 43.57 | 142.80 | 5.63 | 159.20 | 29.84 |
Table 4. Haematological values as a function of each trial arm.
No statistical differences (p>0.05) in systolic, diastolic blood pressure or resting heart rate were found (Table 5).
| Placebo | Peppermint | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Systolic blood pressure (mmHg) | 116.60 | 5.86 | 114.20 | 5.07 | 114.60 | 8.96 | 106.40 | 11.55 |
| Diastolic blood pressure (mmHg) | 73.40 | 13.41 | 74.60 | 8.08 | 74.80 | 10.23 | 72.60 | 10.62 |
| Resting heart rate (beats min⁻¹) | 63.00 | 8.72 | 60.40 | 7.13 | 63.40 | 13.39 | 62.40 | 10.64 |
Table 5. Blood pressure and resting heart rate as a function of each trial arm.
No statistical differences (p>0.05) in beck depression inventory, COOP WONCA, STAI state, STAI trait, PSQI, Insomnia and Epwroth were found (Table 6).
| Placebo | Peppermint | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Beck depression inventory | 3.40 | 3.05 | 3.40 | 3.05 | 3.00 | 3.74 | 2.20 | 3.90 |
| COOP WONCA | 2.00 | 0.47 | 2.00 | 0.47 | 1.77 | 0.30 | 1.77 | 0.30 |
| STAI state | 39.20 | 12.52 | 39.20 | 12.52 | 26.80 | 5.97 | 26.60 | 6.19 |
| STAI trait | 43.40 | 9.84 | 43.40 | 9.84 | 31.00 | 3.94 | 31.40 | 4.28 |
| PSQI | 5.00 | 1.22 | 5.00 | 1.22 | 3.00 | 1.41 | 2.60 | 0.89 |
| Insomnia severity index | 3.80 | 2.17 | 3.80 | 2.39 | 2.20 | 1.92 | 3.2 | 2.39 |
| Epworth sleepiness scale | 4.40 | 3.36 | 4.40 | 4.36 | 4.40 | 4.36 | 4.40 | 4.36 |
Table 6. Questionnaire measurements as a function of each trial arm.
Discussion
This is the first study to evaluate the effects of peppermint oil supplementation after a 20 days period. The study aimed to investigate any changes in cardiometabolic indices in the controlled group compared to a placebo group. The primary aim of this randomised trial is to examine the influence of the peppermint oil oral supplement on systolic blood pressure relative to a placebo. The secondary aim explored the effects of the supplementation of peppermint oil supplementation on other risk factors associated with and as a function of cardiometabolic disease.
Regarding the primary outcome, the current investigation does not support our hypothesis of significant reductions in systolic blood pressure in the peppermint oil group compared to placebo. This result is inverse to the data found by Meamarbashi and Rajabi but their study focused primarily on whilst exercising. Systolic blood pressure in their study decreased by 6.2% after ten days of peppermint oil and diastolic blood pressure decreased by 7.8%. Our findings of no significant change in blood pressure are in line with those of Park, et al. who showed that systolic and diastolic blood pressure were not changed significantly by inhalation of peppermint essential oil. There is contrasting evidence to show that a four percent menthol solution causes blood vessels to widen.
Vasodilation causes a decrease in systemic vascular resistance, subsequently increasing blood flow to downstream capillaries and a decrease in blood pressure. The findings from the current investigation were likely to be because the participants have no previous history of high blood pressure. If we were to conduct the same study on diagnosed hypertensive individuals, the results may be more significant so this is an avenue for future research. In addition to this, it is likely that healthy individuals would respond to a greater extent to a longer term protocol.
The current investigation notably presents a significant decrease in V’O2 at moderate intensity exercise after the intervention. Pulmonary oxygen uptake plateaus to a steady state within about 2-3 minutes at rest to moderate-intensity exercise. In the present study, V’O2 at moderate intensity exercise following 20 days of supplementation, resulted in an 18% decrease. The findings are in agreement that the plateau in both states was reached at a lower level and thus has been affected by external factors outside of the supplement such as diet and lifestyle choices. Work V’O2 is determined by the amount of additional oxygen consumption that is needed to perform work. This excludes the oxygen consumption needed for basal metabolism. At work, the average energy demand is approximately 3.3 kcal/min.
This is in line with the mean total energy demand for this study’s complete data sample at moderate intensity exercise was 3.98 kcal/min (SD=0.57) and for those in the peppermint group at the retest and 3.57 kcal/min (SD=0.50) for the placebo group.
This is comparable to data found during studies performed during the 1950’s and 1960’s but there is no up to date research to support this. Previous research has found that a weight bearing activity produces a 15% greater peak V’O2 value compared to a non-weight bearing activity. Further studies could investigate if peppermint oil creates a statistically significant improvement of V’O2 in weight bearing activity in addition to the non-weight bearing activity which was found in this study.
The study produced statistically significant deteriorations in the pulmonary CO2 output (V′CO2) at moderate intensity exercise in the peppermint group in comparison to the placebo. The mechanisms responsible for the decrease in V’CO2 are not known at this stage. These findings of V’O2 and V’CO2 differences may have considerable exercise physiology relevance rather than clinical. The periodic increases during the measurements at rest can be accounted for by the participant moving slightly to maintain comfort causing oxygenation to arterial blood as it traverses the pulmonary capillaries. The factors that dictate arterial blood gas values are considered multifactorial and complex. Monitoring exhaled CO2 can provide valuable information on the breathing efficiencies of an individual and critical physiologic data in regard to the ventilation and perfusion matching in the lungs, cardiac output, and metabolic rate. CO2 observations in individuals are often underutilised. The reason for this data not being used widespread is likely due to the high costs of the technology required for collecting the data. The volume of exhaled CO2 per minute (VCO2) can also be used to estimate the metabolic rate which can be seen in Table 3.
Although the role of resting heart rate on cardiovascular disease is still unclear, increased resting heart rate has been associated with increased risk of mortality. A study directly focusing on the association of resting heart rate and its change with incident cardiovascular events found that both continuous increase in high baseline heart rate and decrease in low baseline heart rate are associated with higher risk of CVD. A contrasting study found that a resting heart rate of greater than 65 beats/min has a strong independent effect on premature mortality and stroke, but a lesser effect on coronary heart disease. This is not a concern for the participants in this present study as the mean resting heart rate was 63 beats/min. The current investigation showed no significant variations in the peppermint group from pre to post-test compared to the placebo group. Resting heart rate can be considerably affected by stress in a participant's life. A greater overview of resting heart rate variability throughout the 20 days from the peppermint oil could have been acquired through collecting resting heart rate data as well as blood pressure at additional intervals in the protocol. Methods of reducing resting heart rate that focus on lifestyle adjustments or inexpensive and accessible supplements may be beneficial for people with moderate to high levels of resting heart rate. It could be found that with a longer duration protocol, peppermint oil may have an effect on an individual’s resting heart rate but increased research on this area is required.
Peppermint has previously been shown to yield positive effects on human cognitive function. Statistical significance was not found in the psychological well-being in the current investigation compared to placebo. Accounting for underlying behavioural pathways external to the study protocol, it is difficult to find an association at present. Psychological changes are commonly transient and seasonal with a lot of external factors contributing to the individual’s state.
Life satisfaction and positive emotions have been previously associated with reduced risk for incident cardiometabolic conditions. In a study on transgenic mice, sniffing peppermint essential oil showed improvement in learning and memory ability. Lv, et al. concluded that peppermint essential oil may improve cognitive function but there is limited supporting data for humans. With the rising levels of depression and other mental health conditions there is positive support for further investigation into the link of psychological wellbeing to cardiovascular health as well as if peppermint supplementation for a longer duration could contribute positively.
Although previous research has shown that peppermint oil can result in fat loss due to reduced appetite from the supplement, no significant differences were found in the participants of this investigation on body weight or body fat percentage. At the pre-test, the mean BMI value for the peppermint group was 22.67 ± 2.85 and 23.88 ± 2.42 for the placebo group. The healthy BMI range is between 18.5 and 24.9 so weight loss was not a necessary concern for the current participants (NHS, n.d.) A significant correlation between peppermint oil and weight loss may have been established in those already advised to reduce body fat. Obesity is commonly recognised as a direct contributing factor to incident cardiovascular risk factors. Overweight and obesity alone is estimated to contribute to 14% of deaths in Europe, so any accessible and affordable supplement that can produce positive results should be investigated further. Additional research on the utilisation of peppermint oil as a method for reducing mass in those that are categorised as obese is of value.
Assessment of Resting Metabolic Rate (RMR), to provide a nutritional evaluation of individuals is a helpful tool when dealing with clients that are classed as overweight or obese. A prolonged healthy body weight for the duration of one’s lifespan is one of the most effective preventive strategies for heart failure with preserved ejection fraction. RMR did not have any statistically significant differences in this study. Whilst RMR is an indirect cause of issues in cardiometabolic health, it can be a useful indicator of necessary measures to be taken to improve cardiometabolic indices.
Although no statistically significant differences in the primary outcome of improved systolic blood pressure relative to placebo were evident, the long term effects of blood pressure reduction following peppermint oil supplementation have not yet been explored. These findings are contrary to the findings by Barbalho, et al. that found a decrease in blood pressure by 52.5%. It is important to note that blood pressure can increase with dietary changes such as increased sodium intake, increased alcohol consumption and decreased potassium intake. Dietary diaries or standardised nutritional guidelines in the future throughout the 20 days protocol, would provide a more comprehensive understanding. Internationally the primary guideline to maintain optimal blood pressure levels is adopting stress preventative strategies through dietary and lifestyle interventions (ESH/ESC task force for the management of arterial hypertension 2013). Therefore, if these strategies are habitual, then hypertension is unlikely to be a risk thus a peppermint supplement provides no significant change.
Whilst cholesterol didn’t have a statistically significant difference, the higher mean age in the peppermint group compared to the placebo group could be a contributing factor in the variability of the data as research suggests that total cholesterol levels increase with age during young adulthood and middle age. In addition to this, all participants were below the UK’s healthy cholesterol level of 5.0 mmol/L meaning the likelihood of a decrease is small. A participant sample of those with high cholesterol would display with confidence whether peppermint oil is a contributing factor to decreased cholesterol or not. As mentioned with blood pressure, hypercholesterolemia can be prevented with the intervention of an adequate lifestyle, reducing the major risk factor for cardiovascular disorders. It has been found that elevated Low Density Lipoprotein (LDL) for long durations does irreversible and cumulative damage to one’s arteries. The longer a young person has high cholesterol, the greater the risk of developing cardiovascular disease. The NHLBI funded Coronary Artery Risk Development in young Adults study (CARDIA) also stated that two people with the same cholesterol level at age 40 may have very different risks of having a heart attack or stroke with the risk being higher for the person who had higher cholesterol as a teenager. Although this study didn’t find any significant changes in cholesterol or any participants below the healthy levels, it is an important reminder of the severity of high cholesterol and the need for continuous efforts in both identifying high levels early as well as establishing preventative methods.
The mean glucose values of 4.32 mmol/L for the peppermint group and 4.80 mmol/L for the placebo at the start of the study are within the recommended normal fasting blood glucose concentration levels of between 3.9 mmol/L and 5.6 mmol/L. Therefore it is not necessary for lifestyle changes or to monitor glycemia currently regardless of the supplement. Anand, et al. found that a 1 mmol/l increase in fasting plasma glucose presented a 17% increase in the risk of future cardiovascular events or death. Whilst peppermint oil at this stage presents no clear indication that it reduces high glucose levels, the same protocol could be applied to future supplements for scientific research. An additional study by Asia pacific cohort studies collaboration assessed the link between glucose and the risk of cardiovascular disease by analysing 237,468 participants fasting blood glucose data. The conclusion from their statistical analysis was that fasting blood glucose is an important factor of cardiovascular disease, with the considerable potential benefit of usual blood glucose in a reduction of levels to at least 4.9 mmol/l.
The triglyceride glucose index has been established as a reliable alternative biomarker of insulin resistance. Lipid guidelines for CVD prevention have evolved over recent years with current research, but it is now consistently defined, including in the national health and nutrition examination survey, that elevated triglyceride levels are considered anything above >8.3. The mean triglyceride values of 1.20 mmol/L for both the peppermint group and for placebo at the start of the study are considered in the healthy range. Elevated triglyceride levels are associated with increased cardiovascular risk, even in the “normal” range but the association between triglyceride levels and cardiovascular events differs by sex.
Anaemia or low haemoglobin levels have been found to be a contributing factor in negatively affecting the cardiovascular system. Left ventricular hypertrophy has been a symptom of long term anaemia. The adult normal haemoglobin range of 130 g/L-180 g/L and 115 g/L-165 g/L for females supports the findings that all participants in the current investigation were in the normal range with a mean value of 142 g/L thus no reason for significant change. Research is inconclusive on whether a haemoglobin level or haemoglobin physiologic range has any effect on CVD incidences. Anaemia independent pathways include direct effects of cardiac iron deficiency on metabolism, oxygen sensing, and calcium handling in the heart and of vascular iron deficiency on oxygen sensing and vasoconstriction in the pulmonary arteries.
Participant feedback supports other relevant investigations that the peppermint was well tolerated with few adverse events, with no unexpected gastrointestinal issues associated with the nutritional supplement. Adjusting the method of supplementation may also provide more significant results for the variables measured during this investigation. Whilst this study ingested the peppermint sample as an oil, as mentioned earlier, topical or inhalation protocols with peppermint have seen positive results and inspire future research.
Conclusion
Overall, the current investigation presented an effective level of blinding efficacy, no known adverse incidents, a high retention rate, very good compliance levels, as well as improvements in V’O2 and V’CO2 in the peppermint arm. Further research studies with larger sample sizes and longer durations with the use of different methods of peppermint supplementation are required in hypertensive patients with predefined hypertension stages to confirm or deny whether supplementation of peppermint oil may be a safe nutritional intervention for treating hypertension. The same should be performed for those at risk of cardiovascular disease. Nevertheless, this field of research studying the effects of peppermint oil supplementation is novel and understudied. Therefore, further studies are necessary to be able to give a definitive answer that increased peppermint oil supplementation has positive alterations on cardiometabolic indices and other health related outcomes.
Limitations
A challenge during data collection was having to follow COVID-19 protocol. In the event of a positive COVID-19 result, the participant was unable to return for the post-protocol test on the assigned day, so data collection was in some cases delayed a few days which may have altered the retest results. An additional challenge was ensuring all the participants took their provided supplement, twice daily, for the duration of the study. All participants were encouraged to have the supplement before breakfast and after their evening meal but the timings of consumption varied between participants. The time in which the peppermint oil was taken the night before the retest may have affected the data. Whilst participants were asked to not exercise the day of the retest before coming to the lab, as well as no high intensity exercise in the 24 hours before, we had no control over if the participants did this. Participants’ lifestyles outside of the lab may also impact the significance over the 20 days protocol. Although all participants completed the questionnaires to assess sleep quality and psychological wellbeing, all of the answers were subjective rather than backed up with quantitative data. To gain a more comprehensive understanding of their sleep quality and state of rest, resting heart rate in the morning could be acquired as well as the potential of sleep tracking devices being used. There is also variability in whether the participants did the test in a fasted state or unfasted. In the future, standardising nutrition prior to testing would be beneficial.
Given the time constraints on the study, the total number of participants was 10 which given the double blind nature meant we had five participants in each group (control vs. placebo). Therefore, the results of this investigation need to be considered with caution and to gain confidence in the findings, more samples need to be analysed.
Disclosures
The author has no relationship with the supplement providers thus there are no known conflicts of interest or factors that should be disclosed for any other reason. All nutritional supplements were self-bought by the university of Central Lancashire so there is no financial support from external parties which would promote any bias.
References
- Aberra T, Peterson ED, Pagidipati NJ, et al. The association between triglycerides and incident cardiovascular disease: What is “optimal”?. J Clin Lipidol. 2020;14(4):438-47.
[Crossref] [Google Scholar] [PubMed]
- Ahmed CS, Jiang H, Chen JY, et al. Traffic related particulate matter and cardiometabolic syndrome: A review. Atmosphere. 2018;9(9):336.
- Alam MS, Roy PK, Miah AR, et al. Efficacy of Peppermint oil in diarrhea predominant IBS-a double blind randomized placebo controlled study. Mymensingh Med J. 2013;22(1):27-30.
[Google Scholar] [PubMed]
- Asia Pacific Cohort Studies Collaboration. Blood glucose and risk of cardiovascular disease in the Asia Pacific region. Diabetes Care. 2004;27(12):2836-42.
[Crossref] [Google Scholar] [PubMed]
- Barbalho SM, Machado FM, Oshiiwa M, et al. Investigation of the effects of peppermint (Mentha piperita) on the biochemical and anthropometric profile of university students. Food Sci Technol. 2011;31(3):584-8.
- Bazzano LA, Green T, Harrison TN, et al. Dietary approaches to prevent hypertension. Curr Hypertens Rep. 2013;15(6):694-702.
[ -->