Research Article - Journal of Pain Management and Therapy (2021) Special Issue on Pain and Physical Therapy
The effect of low-level laser therapy on persistent Idiopathic facial pain.
Adel Bouguezzi1*, Maroua Garma2
1 Department of Oral Health and Oro-Facial Rehabilitation, University of Monastir, Monastir, Tunisia
2 Department of Oral Pathology and Oral Surgery, University of Monastir, Monastir, Tunisia
Corresponding Author:
- Dr. Adel Bouguezzi
Department of Oral Health and Oro-Facial Rehabilitation University of Monastir Monastir Tunisia
E-mail: dr-adel@live.fr
Accepted date: 22 May, 2021
Citation: Bouguezzi A, Garma M. The effect of low-level laser therapy on persistent Idiopathic facial pain. J Pain Manage Ther. 2021;5(4):1-3.
Abstract
Trigeminal neuralgia is a pain passes through nerve's branches and its trigger is located in skin or mucosa that could lead to pain with a trigger stimulus. The pain involved branches of trigeminal nerve that sometimes has patients to seek the treatment for several years. Low-Level Laser Therapy (LLLT) is a treatment strategy which uses a single wavelength light source. In this article, we report on four patients who were diagnosed with Persistent Idiopathic Facial Pain (PIFP). All patients were treated with LLLT system that produces low-energy infrared light (808 nm diodes). The laser was applied to the symptomatic locations. Patients were treated once per day for five consecutive days, followed by a two-day interval. This regimen continued until the total number of applications reached 20. The results of our study show that LLLT could have beneficial effect on patients with orofacial pain as partial or total resolution of symptoms.
Keywords
Trigeminal nerve, Idiopathic orofacial pain, Laser low level.
Introduction
Low Level Laser Therapy (LLLT) is becoming more used due to its beneficial effects in various medical conditions but also due to the fact that treatment with LLLT is pain free and has few contraindications.
The use of LLLT for peripheral nervous system regeneration is currently being investigated in order to achieve early functional nerve recovery. There are only few studies regarding the use of LLLT for nerve recovery in humans and rats [1].
Materials and Methods
Four patients with Persistent Idiopathic Facial Pain (PIFP) were involved in this study. Diagnosis of PIFP was carried out according to criteria established the Headache Classification Subcommittee of the International Headache Society [2].
(1) Facial pain present daily for at least 1 month and persisting for all or most of the day.
(2) The pain is deep and poorly localized of moderate or severe intensity, but not unbearable.
(3) The pain is confined at onset to a limited area on one side of the head.
(4) The pain is without paroxysms, precipitation from trigger areas, autonomic symptoms, sensory loss, and other physical signs; but dysaesthesia may occur [3].
The exclusion criteria were other orofacial pain conditions due to odontogenic causes, vascular conditions (migraine, etc.) and inability of patient to understand the text of the informed consent.
None of the patients had systemic diseases nor took meds that might affect their pain.
The study was approved by the local ethics commission and informed written consent was obtained from all patients.
Patients had unrelenting facial pain. Patients had tried various medications including analgesics, NSAIDs, and steroids, all of which offered no relief [4].
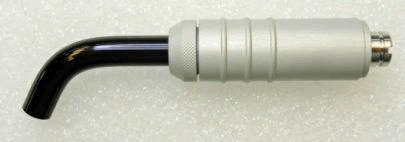
In the study, The GaAlAs diode laser device was used (Figure 1), the irradiation parameters were the wavelength of 808 ± 10 nm, power of 100 mW, and pulse frequency of continuous waveform-20,000 Hz.
The spot size was 6 mm (Figure 2) and the beam surface area was 0.28 cm².
On the other hand, the radiant exposure or fluency was 32.86 J/cm² and the power density was 0.71 W/cm².
Furthermore, the applicator was placed at proximity of the skin or mucosa at the most painful surface for 30s.
Application was performed once per day for five consecutive days, followed by a two-day interval [5].
The total number of applications was 20. Although there are, yet, no established treatment protocol for various conditions treated with LLLT, we chose 20 treatments based on standard protocol used in wound care.
Outcome primary endpoint was patients’ report on the relief of symptoms (0=no improvement, 1=partial improvement, 2=complete improvement) after 20 sessions of treatments (Figures 1 and 2).
Results
Our report indicates that LLLT appears to be effective in the treatment of TN for our four patients, a total resolution of symptoms was achieved in 50% of patients. Results Clinical characteristics of the patients are presented in (Table 1) [6].
| Gender | Age | Diagnosi s | Site | Sympto ms (months ) |
Outcom e | |
|---|---|---|---|---|---|---|
| Patient 1 | F | 54 | PIFP | Lower Lip, left side | 15 | Partial improve ment |
| Patient 2 | F | 72 | PIFP | Maxillary ridge, right molar region | 82 | Partial improve ment |
| Patient 3 | M | 59 | PIFP | Lower lip, left side | 3 | Complet e improve ment |
| Patient 4 | F | 49 | PIFP | Left mental region | 25 | Complet e improve ment |
Discussion
The mechanism of pain production remains controversial. One theory suggests that peripheral injury or disease of the trigeminal nerve increases afferent firing in the nerve. Failure of the central inhibitory mechanisms may be involved [7]. Authors have hypothesized that trigeminal pain related has a peripheral etiology as well as a central pathogenesis factor.
They evaluate that chronic irritation of the trigeminal nerve leads to both a failure of segmental inhibition in the trigeminal nucleus, and ectopic action potentials in the trigeminal nerve. In 95% of cases, no lesion is diagnosed, and the cause is labeled idiopathic by default. Some authors have speculated that, like Bell’s palsy, a neurotropic virus may be the causative agent and the proximity of the two nerves may give cause to further support this theory [8].
Ch’ien and Halsey reported two cases of concomitant trigeminal sensory neuropathy and Bell’s palsy. Although the exact pathogenesis is unknown, it is, however, generally accepted that focal demyelination in the root of the trigeminal nerve is involved.
Persistent idiopathic facial pain is the current terminology for Atypical Facial Pain and is characterized by daily or near daily pain that is initially confined but may subsequently spread. Pain cannot be attributed to any pathological process, although traumatic neuropathic mechanisms are suspected. When present intraorally, PIFP has been termed 'Atypical Odontalgia', and this entity is discussed in a separate article in this special issue. PIFP is often a difficult but important differential diagnosis among chronic facial pain syndromes [9].
When the cause of the TN is identifiable, treatment involves elimination of the cause. In idiopathic cases, however, a variety of medicinal and surgical treatment modalities should be considered. Medicinal management includes carbamazepine, phenytoin, baclofen, gabapentin, oxcarbazepine, lamotrigine, pimozide, and tizanidine hydrochloride.
Although medication is the first line of treatment, tolerance may develop as the treatment period and the need for extra dosage increase, which leads to more side effects. Nearly 50% of TN sufferers are not satisfied with medical therapy, because of incomplete control of pain or drug-related side effects. Drowsiness, fatigue, dizziness, nausea, nystagmus, memory loss, and a sense of exhaustion are common side effects of carbamazepine which necessitates finding alternative treatment.
Pregabalin was chosen by most clinicians because it has a better pharmacological profile when compared to Gabapentin. In addition, Pregabalin has been associated with lower pain levels compared to Gabapentin, despite its higher cost. The association of anticonvulsants with tricyclic antidepressants or selective serotonin and noradrenaline reuptake inhibitors, although also used in the treatment of PIFD, had no clinical evidence [10].
The treatment is difficult and often requires a multidisciplinary approach. The most important part of the treatment is psychological counseling and pharmacological therapy. Pharmacological treatment with tricyclic antidepressants and anti-epileptic drugs can be tried [11]. The conservative, pharmacological treatment with amitriptyline is the primary choice. Venlafaxine and fluoxetine treatment can also be considered.
There have been numerous claims in the literature for the therapeutic effects of LLLT treatment such as acceleration of wound healing pain attenuation restoration of normal neural function following injury enhanced remodeling and repair of bone, normalization of abnormal hormonal function, stimulation of endorphin release and modulation of the immune system [12].
LLLT has beneficial effect on paraesthesia’s with lasers 4–6 J per point along the projection of the nerve. Also reported that GaAlAs laser therapy (820 nm, 4 × 6 J per treatment, in a total number of 20 treatments) results in both subjective and objective improvement in mechanical sensory perception in long standing neurosensory deficit of the inferior alveolar nerve. Used 632.8 nm, 670 nm and 830 nm diode lasers in patients with temporomandibular joint pain and trigeminal neuralgia. Most of the patients had 12 applications (twice a week) with an average dose of 1.8 J/cm2. Most treatment consisted of a series of 12 applications (twice a week) and in 15 cases a second series was applied. Patients were treated with an average dose of 1.8 J/cm2.
More recent studies such as one studied LLLT in 16 patients with Persistent Idiopathic Facial Pain (PIFP) and average pain reduction of 43.47% (ranging from 9.3% to 91.8%) was achieved which is lower percentage in comparison to our sample (70%). However, their patients received LLLT between one to ten times, whereas all our patients received the same LLLT regimen (ten times altogether). The same authors concluded that LLLT may be an effective treatment for PIFP.
Last but not least we have to mention the limitations of present study: small number of patients, self-evaluation of symptoms (visual analogue scale should be used in the future), lack of placebo group and different duration of symptoms (the duration of the symptoms should be divided into acute and chronic in the future studies) [13]. The results of our study show that LLLT could have beneficial effect on patients with or facial pain as partial or total resolution of symptoms.
Conclusion
LLLT with its biostimulatory, antiinflammatory and analgesic effects has proven to be an effective intervention in reducing pain in trigeminal neuralgia patients. Nevertheless, this treatment modality still has not been included in every day dental practice in the treatment of chronic idiopathic orofacial pain. One of the reasons might be a lack of standardization of treatment protocol for LLLT. Therefore, one of the aims of this paper was to contribute in developing specific guidelines for the use of LLLT in patients with TN as we have less need for surgical treatment or medicine use. LLLT may also have a positive psychological effect, especially on patients suffering from chronic pain conditions, such as TN.
Competing Interests
The authors declare that they have no competing interests.
References
- Broggi G, Ferroli P, Franzini A, et al. Microvascular
- decompression for trigeminal neuralgia: comments on a
- series of 250 cases, including 10 patients with multiple
- Baker KA, Taylor JW, Lilly GE, et al. Treatment of trigeminal neuralgia: use of baclofen in combination with carbamazepine. Clin Pharm. 1985;4:93–6.
- Cheshire WP. Trigeminal neuralgia: diagnosis and treatment. Curr Neurol Neurosci Rep. 2005;5:79–85.
- sclerosis. J Neurol Neurosurg Psychiatry. 2000;68:59-64.
- Walker J. Relief from chronic pain by low power laser irradiation. Neurosci Lett. 1983;43:339-44.
- Burchiel KJ, Slavin KV. On the natural history of
- Poole TE, Holland I, Peterson LJ, et al. Clinical efficacy of low level laser treatment of oro-facial neurosensory deficits. J Oral Maxillofac Surg. 1993;182.
- Walsh LJ. The current status of low level laser therapy in dentistry. Part 1. Soft tissue applications. Aust Dent J. 1997;42:247-54.
- Khullar SM, Emami B, Westermark A, et al. Effect of low- level laser treatment on neurosensory deficits subsequent to sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:132-38.
- Pinheiro AL, Cavalcanti ET, Pinheiro TI, et al. Low-level laser therapy is an important tool to treat disorders of the maxillofacial region. J Clin Laser Med Surg. 1998;16:223- 26.
- trigeminal neuralgia. Neurosurgery. 2000;46:152-55.