Case Report - Biomedical Research (2017) Volume 28, Issue 8
Surgical treatment of renal cell carcinoma metastatic to the pancreas: report of one case and review of the literature
Wei-Feng Yao1*, Jun-Wei Liu1, Xiang-Lei He2 and Cheng-Wu Zhang1*1Department of Hepato-Biliary-Pancreatic Surgery and Hernia Center, Zhejiang Provincial People’s Hospital, Hangzhou, PR China
2Department of Pathology, Zhejiang Provincial People’s Hospital, Hangzhou, PR China
- *Corresponding Author:
- Wei-Feng Yao
Department of Hepato-Biliary-Pancreatic Surgery and Hernia Center
Zhejiang Provincial People’s Hospital, PR China
Cheng-Wu Zhang
Department of Hepato-Biliary-Pancreatic Surgery and Hernia Center
Zhejiang Provincial People’s Hospital, PR China
Accepted date: December 29, 2016
Abstract
Metastasis of Clear Cell Renal Cell Carcinoma (CCRCC) to the pancreas is uncommon. Herein, we describe a case of a 53-year-old man with a history of CCRCC treated by radical left nephrectomy 11 years previously, who presented with a pancreatic tumor detected during health examination. Computed Tomography (CT) scan, Magnetic Resonance Imaging (MRI) and Positron Emission Tomography CT (PET-CT) confirmed a solitary mass at the head of pancreas. Cytological diagnosis by FNA prior to surgery was metastatic carcinoma. Standard pancreaticoduodenectomy was performed and postoperative pathology confirmed as metastatic CCRCC. The patient had an uneventful post-operative recovery. Now he was followed up for 18 months and no clinical signs of recurrence occurred.
Keywords
Renal cell cancer, Pancreatic metastases, Pancreaticoduodenectomy, FNA
Introduction
Metastatic pancreatic cancer from another primary site is rare, and the estimated frequency ranging from 2% to 5%, and may occur long after manifestation of the primary cancer, regardless of its site [1]. Clear Cell Renal Cell Carcinoma (CCRCC) is one of the primary locations known to metastasis to the pancreas, with less than 2% reported [2]. Mostly, about half of cases in which the pancreas is the only metastatic site and is isolated metastasis [3,4]. Therefore, it is important to find out a better way to treat the pancreatic metastasis from RCC. So far, there have been several case reports and case series of pancreatic metastasis from a renal primary lesion treated with surgical resection. In some studies, there is no significant difference in overall survival between the surgical group and drug treatment group. So far, there have been few reports on the relationship between FNA and pancreatic metastasis in the preoperative diagnosis of renal cell carcinoma, which is mainly based on the patient's previous history of renal cell carcinoma, and the imaging finding. Recent reports have shown that pancreatic metastasis in CT can be manifested as high density lesions or low density lesions, for this reason the pancreatic metastasis of renal cell carcinoma in the image is not typical of the performance.
Herein, we report a case of a 53-year-old man, who present with a pancreatic tumor detected during health examination. Had a history of RCC treated by radical left nephrectomy 11 years previously, and reviewed several studies and case reports in recent years, expect to find out a best way to treat this disease.
Case Report
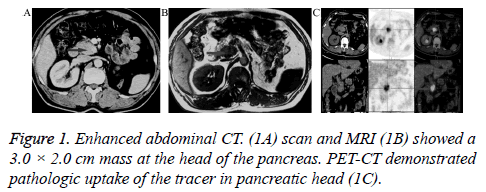
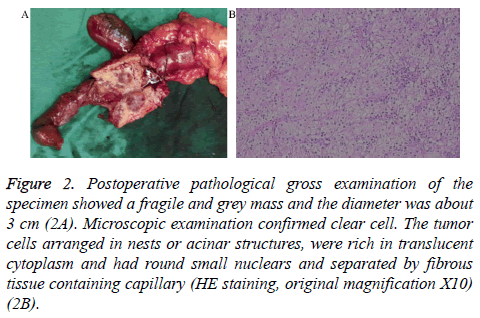
A 53-year-old man had received left nephrectomy due to left renal tumor 11 years previously, and the pathologic results were CCRCC with negative ureteral margin. After 11 consecutive years of follow-up, he underwent a medical examination and BUS showed a mass in the head of the pancreas. In spite of no obvious symptoms, he was admitted and several imaging examinations were introduced in order to make a diagnosis. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) scan and MRI showed a unique 3.0 cm × 2.0 cm mass at the head of pancreas (Figure 1A and 1B). Positron Emission Tomography CT (PET-CT) demonstrated abnormal metabolic activity in pancreatic head (Figure 1C). Cytological diagnosis by FNA prior to surgery was metastatic carcinoma. Pancreatic metastasis from CCRCC was confirmed according to the history of CCRCC and these results. Then he was scheduled for surgical resection. Intraoperative rapid pathologic results revealed pancreatic metastatic clear cell carcinoma, so standard pancreaticoduodenectomy was performed. Postoperative pathological gross examination of the specimen showed a fragile and grey mass and the diameter was about 3 cm (Figure 2A). Microscopic examination confirmed clear cell. The tumor cells arranged in nests or acinar structures, were rich in translucent cytoplasm and had round small nuclear and separated by fibrous tissue containing capillary (Figure 2B). The patient had an uneventful post-operative recovery. Now he was followed up for 18 months and no recurrence occurred. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Zhejiang Provincial People’s Hospital. Written informed consent was obtained from participant.
Figure 2: Postoperative pathological gross examination of the specimen showed a fragile and grey mass and the diameter was about 3 cm (2A). Microscopic examination confirmed clear cell. The tumor cells arranged in nests or acinar structures, were rich in translucent cytoplasm and had round small nuclears and separated by fibrous tissue containing capillary (HE staining, original magnification X10) (2B).
Discussion
Currently CCRCC is increasing all over the world. Among these patients, approximately 20%-30% have a metastatic status at the time of presentation. Moreover, the tendency of secondary diseases is common in spite of early treatment by nephrectomy for primary CCRCC [5]. In our case, the patient was found pancreatic metastasis after resection of renal cell carcinoma 11 years, which is consistent with most of the cases currently, reported disease-free survival. For this reason a long follow up above 10 years is necessary in patients with CCRCC [1]. Pancreas is one of the secondary locations of CCRCC and it is often involved in diffuse metastatic disease [6]. Isolated metastasis to the pancreas is rare, ranging in incidence from 2%-5% [7].
In our case, the patient had no symptoms, and pancreatic mass was found by routine examination after nephrectomy, CT and MRI showed a mass in pancreas head, about 3 cm in size. As reported in earlier similar case, pancreatic metastases are rarely symptomatic. Most patients are detected during follow-up investigations after previous operation or annual physical examination [1]. Just like this case. While some patients may present with abdominal pain (20%), gastrointestinal tract bleeding (20%), obstructive jaundice (9%), weight loss (9%), pancreatitis (3%) or diabetes mellitus (3%), which is similar with other malignant tumors, especially primary pancreatic tumor [8]. Several studies showed that the diameter of the metastatic lesion have some association with patient symptoms. Bassi reported that in asymptomatic patients the median tumor diameter was less than 25 mm, while 45 mm in symptomatic patients [9].
The preoperative diagnosis of pancreatic metastasis from CCRCC is a suspicion based on the fact that the patients had a surgical resection previously. Imaging examinations such as US, CT, MRI, EUS and PET-CT can help to make diagnosis. Sometimes fine-needle biopsy by the conduct of EUS or CT was helpful to confirm the clinical suspicion. As this case, an obvious nodular enhancement at arterial and portal phases was described on CT scan. MRI found the same lesion. PET-CT was introduced to identify the distant metastasis. The diagnosis was confirmed with cytological result by fine-needle biopsy. In Our opinion, preoperative EUS and FNA are very important, can get pathological diagnosis preoperatively. The diagnosis rate of clear cell carcinoma by FNA cytology was about 77%, mainly because of its cytological features, which was obvious in the features of haemorrhage and necrosis. Compared to other metastatic pancreatic cancer, the present study showed that renal cell carcinoma with pancreatic metastasis is relatively good in the prognosis, and if other parts of the tumor metastasis to the pancreas, that means the cancer had no surgical indications. So, we can formulate the treatment plan before surgery for pancreatic mass by FNA cytology.
In our case, a standard pancreaticoduodenectomy was performed; the patient had an uneventful post-operative recovery. Now he was followed up for 18 months and no clinical signs of recurrence occurred. At present surgical resection of pancreatic metastasis from CCRCC remains the most effective treatment. Surgical resection might be associated with long-term disease-free intervals in highly selected patients. Hoshino et al. reviewed studies from 1998 to 2013 that focused on surgical resection. The results showed the median 5-year overall survival rate after metastasectomy was reported to be 75% to 88%, compared to 0% to 50% without metastasectomy [10]. Raphael Benhaim et al. reported a retrospective monocentric study including 20 surgically treated patients, median follow-up after pancreatectomy was 69 months (1-150 months). Disease-free survival at 2 years was 60%. Overall survival rates at 2 and 4 years were 79% and 72% respectively [11]. At the meantime, targeted therapies, such as sunitinib and pazopanib, have shown efficiency on metastatic CCRCC with improvement of overall survival [12]. In addition, radiofrequency ablation for pancreatic malignancies may be a facultative option, but recently a systematic review reported median survival after RFA of 3-33 months, morbidity related to RFA of 4%-37%, mortality of 0-19% and overall morbidity of 10%-43% [13]. It means that compared with control group, the RFA has no obvious advantage while significantly increased the risk; it is not recommended that the RFA for pancreas metastasis, chemotherapy, radiotherapy and immunotherapy have proved to be ineffective for metastatic CCRCC.
Patients with pancreatic metastases from CCRCC should be evaluated with a multidisciplinary method, but the literature on this subject is limited due to rarity of such pancreatic metastasis. Most of the data in the literature are from case reports and randomized trials were difficult to conduct. Further researches are necessary to establish the approach to combine surgery with other treatments in the different stage of pancreatic metastasis.
Conflict of Interest
All authors have no conflict of interest regarding this paper.
References
- Zerbi A, Ortolano E, Balzano G, Borri A, Beneduce AA, Di Carlo V. Pancreatic metastasis from renal cell carcinoma: which patients benefit from surgical resections? Ann Surg Oncol 2008; 15: 1161-1168.
- Crippa S, Angelini C, Mussi C, Bonardi C, Romano F, Sartori P, Uggeri F, Bovo G. Surgical treatment of metastatic tumour to the pancreas: a single center experience and review of the literature. World J Surg 2006; 30: 1536-1542.
- Masetti M, Zanini N, Martuzzi F, Fabbri C, Mastrangelo L, Landolfo G, Fornelli A, Burzi M, Vezzelli E, Jovine E. Analysis of prognostic factors in metastatic tumors of the pancreas: a single-center experience and review of the literature. Pancreas 2010; 39: 135-143.
- Akashi Y, Saiura A, Kishi Y, Koga R, Morimura R, Yoshioka R, Yamamoto J, Yamaguchi T. Outcome after surgical resection of isolated metastases to the pancreas. Hepatogastroenterol 2010; 57: 1549-1552.
- Leibovich BC, Blute ML, Cheville JC, Lohse CM, Frank I, Kwon ED, Weaver AL, Parker AS, Zincke H. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer 2003; 97: 1663-1671.
- Konstantinidis IT, Dursun A, Zheng H, Wargo JA, Thayer SP. Metastatic tumors in the pancreas in the modern era. J Am Coll Surg 2010; 211: 749-753.
- Ballarin R, Spaggiari M, Cautero N, De Ruvo N, Montalti R. Pancreatic metastases from renal cell carcinoma: the state of the art. World J Gastroenterol 2011; 17: 4747-4756.
- Sellner F, Tykalsky N, De Santis M, Pont J, Klimpfinger M. Solitary and multiple isolated metastases of clear cell renal carcinoma to the pancreas: an indication for pancreatic surgery. Ann Surg Oncol 2006; 13: 75-85.
- Bassi C, Butturini G, Falconi M, Sargenti M, Mantovani W. High recurrence rate after atypical resection for pancreatic metastases from renal cell carcinoma. Br J Surg 2003; 90: 555-559.
- Hoshino Y, Shinozaki H, Kimura Y, Masugi Y, Ito H, Terauchi T, Kimata M, Furukawa J, Kobayashi K, Ogata Y. Pancreatic metastases from renal cell carcinoma: a case report and literature review of the clinical and radiological characteristics. World J Surg Oncol 2013; 11: 289.
- Benhaim R, Oussoultzoglou E, Saeedi Y, Mouracade P, Bachellier P. Pancreatic metastasis from clear cell renal cell carcinoma: outcome of an aggressive approach. Urology 2015; 85: 135-140.
- Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, Nathan P, Staehler M, de Souza P, Merchan JR, Boleti E, Fife K, Jin J, Jones R, Uemura H, De Giorgi U, Harmenberg U, Wang J, Sternberg CN, Deen K, McCann L, Hackshaw MD, Crescenzo R, Pandite LN, Choueiri TK. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. New Engl J Med 2013; 369: 722-731.
- Fegrachi S, Besselink MG, van Santvoort HC, van Hillegersberg R, Molenaar IQ. Radiofrequency ablation for unresectable locally advanced pancreatic cancer: a systematic review. HPB (Oxford) 2014; 16: 119-123.