Research Article - Current Pediatric Research (2023) Volume 27, Issue 2
Study on resistance pattern of neonatal bacterial sepsis to establish antibiotic stewardship for tertiary care NICU in central India.
Deepak Kumar Patel*, Mamta Dhaneria, Ashish J Pathak
Department of Paediatrics, RD Gardi Medical College and CRG Hospital, Ujjain, Madhya Pradesh, India
- Corresponding Author:
- Deepak Kumar Patel
Department of Paediatrics,
RD Gardi Medical College and CRG Hospital,
Ujjain, Madhya Pradesh,
India
E-mail: helenfelicia24@gmail.com
Received: 26 January, 2022, Manuscript No. AAJCP-23-88467; Editor assigned: 30 January, 2022, Pre QC No. AAJCP-23-88467(PQ); Reviewed: 13 February, 2023, QC No. AAJCP-23-88467; Revised: 20 February, 2023, Manuscript No. AAJCP-23-88467(R); Published: 28 February, 2023, DOI:10.35841/0971-9032.27.02.1795-1801.
Abstract
Background: Neonatal sepsis is significant cause of morbidity and mortality among neonates worldwide. World Health Organization (WHO) has estimated that 1.6 million deaths occur globally every year due to neonatal infections and 40% of all neonatal deaths occur in developing countries. In India, the incidence of blood culture proven sepsis was reported as 8.5 per 1,000 live births, as per the national neonatal perinatal database. It was found that sepsis is one of the commonest causes of neonatal mortality contributing to 19% of all neonatal deaths so we planned a study to know about resistant pattern of neonatal bacterial sepsis and promote rational use of antibiotics for establish antibiotic stewardship at tertiary care hospital NICU.
Materials and methods: The retrospective observational study was conducted at RD Gardi medical college and CR Gardi hospital, Ujjain on neonates admitted in NICU with clinical suspicion of sepsis. The time duration of the study was from January 2019 to January 2020. Data was collected using a mobile phone based application; this application was specifically designed to collection of data for the study. And data were entered on Microsoft excel sheet and analyzed by a software STATA 10.
Results: Sepsis was common more common in boys, preterm babies, and very low birth weight babies. Among the clinical features of admitted neonates only respiratory distress had significant correlation with culture positive sepsis. Increase risk was associated with mechanical ventilation in neonates. Gram negative organism constitutes 87% of all isolates and gram positive 13%. The most frequently isolated organism in blood was Burkholderia cepacia (33%). Among gram positive organism’s Staph aureus was most frequently isolated. Gram negative organisms were most resistant to Ampicillin and Cephalosporin group of antibiotics and were most sensitive to colistin, tigecycline and meropenem. Gram positive organisms were least resistant to vancomycin, teicoplanin and linezolid.
Burkholderia cepacia was the most common causes of neonatal sepsis in our study. A significant proportion of the isolates were multidrug resistant strains which pose a great threat to neonatal survival. Implementation of effective preventive strategy to combat the emergence of antibiotic resistance needed. We recommended a combination of piperacillin-tazobactum and amikacin as a first line therapy and the combination of meropenem and vancomycin as the second line imperical therapy in our NICU.
Keywords
Neonatal sepsis, NICU, Antimicrobial resistance.
Introduction
Neonatal sepsis is a systemic condition of bacterial, viral, or fungal (yeast) origin that is associated with hemodynamic changes and other clinical manifestations in neonates. Neonatal sepsis is a significant cause of morbidity and mortality among neonates worldwide [1,2]. World Health Organization has estimated that 1.6 million deaths occur globally every year due to neonatal infections and 40% of all neonatal deaths occur in developing countries [3]. In India, the incidence of blood culture proven sepsis was reported as 8.5 per 1,000 live births for the year 2002–2003 by the national neonatal perinatal database [4]. In recent years, the subject of the emergence and subsequent increase in the incidence of resistance to antimicrobial agents has become a serious threat. Reports from all around the world suggest that antibiotics are rapidly losing their effectiveness, with some early reports going so far as to suggest that we are approaching a post-antibiotic era [5].
The rate of antimicrobial resistance among neonatal sepsis pathogens is steadily increasing; A 2000s surveillance revealed increasing rates of MRSA, VRE, and other patterns of resistance patterns. Various fetal, maternal and NICUs environmental factors contribute toward causing infections in newborns. Apart from the immature immune system, some of the fetal factors that predispose neonates to infections are: Low birth weight, gestational age and APGAR score, prolonged hospital stay, invasive procedures, endotracheal tubes, umbilical cauterization, parenteral nutrition, lack of adequate hand washing by hospital personnel and indiscriminate use of antibiotics [6]. Neonatal sepsis has been illustrated to be a leading cause of neonatal morbidity and mortality within both, clinical care and community settings of India [7].
Thus, this shows the importance of identifying the etiologic agents and the contributing risk factors for causing neonatal infections in NICUs and to work out the preventive measures to reduce the morbidity and in turn mortality in NICUs. The present retrospective study was therefore undertaken with the aim to study resistance pattern of neonatal bacterial sepsis to established antibiotics stewardship for tertiary care NICU at CR Gardi hospital and RD Gardi medical college Ujjain MP.
Materials and Methods
The retrospective observational study was conducted at RD Gardi medical college and CR Gardi hospital, Ujjain on neonates admitted in NICU after obtaining ethics committee clearance with clinical suspicion of sepsis. The time duration of the study was from January 2019 to January 2020.
Inclusion criteria
All neonates from 0 to 28 days of life which were admitted with suspected neonatal sepsis in NICU department of paediatrics during January 2019 to January 2020..
Exclusion criteria
• Neonates who already have taken antibiotics prior to admission will be excluded from the study.
• Neonates with sepsis caused by fungal organism and anaerobes were also not included.
• Presence of major congenital malformation.
Case selection procedure: We enrolled 167 neonates who were admitted in NICU at RDGMC during January 2019 to January 2020 and fulfilled at least one of the following clinical signs and symptoms were considered suspected sepsis: Fever, hypothermia, respiratory distress including cyanosis and AZpnoea, etc. After admission of the neonate blood sample was taken and send it for sepsis screening and blood culture analysis. After that positive blood culture sample was sent for antibiotic susceptibility testing.
Sepsis screen (7): The cut off values of the positive rapid screening tests in this study are as follows:
• Total leukocyte count <5000/mm.
• Absolute neutrophil count <1800/mm3.
• Immature (band cells) to total neutrophil ratio>0.2.
• C-Reactive Protein (CRP): >1 mg/dl.
• Micro ESR >15 mm in 1st hour.
If any two of the following parameters are positive or significant, the sepsis screen said to be positive.
Antibiotic susceptibility testing: Antibiotic susceptibility tests were carried out by the Kirby-Bauer disc diffusion method, as stated by the standards of Clinical and Laboratory Standards Institute (CLSI) [8], three to four colonies of the isolated organism were mixed with sterile saline until the turbidity of the mixture was equivalent to 0.5 MacFarland, and then the suspension was swabbed over Muller-Hinton Agar (MHA) plates. Antibiotic discs were then added within 15 min and incubated overnight at 37°C (18 hrs). The different groups of antibiotics were represented.
Data were collected from an android based software and then entered into Microsoft excel sheet and analyzed by statistical software STATA 10. Chi square test with 95% Confidence Interval (95% CI) used to calculate Odds Ratios (OR) for potential risk factors.
Results
In present study out of 167 neonates with clinical suspicion of sepsis, 32% neonates had positive blood culture sepsis. Male sex (39%) very low birth weight (46%) and preterm (53%) were important neonatal risk factor for sepsis (Table 1).
| Characteristics | Categories | Number n (%) | Culture positive sepsis n(%) | OR | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Sex | Male | 96 (57) | 37 (39) | 1.98 | 1.007-3.998 | 0.04 |
| female | 71 (43) | 17 (24) | ||||
| Birth weight | Normal | 43 (26) | 10 (23) | 2.86 | 1.02-7.97 | 0.045 |
| LBW | 96 (57) | 31 (32) | ||||
| VLBW | 28 (17) | 13 (46) | ||||
| Gestation | Term | 118 (71) | 28 (24) | 3.63 | 1.79-7.34 | 0.001 |
| Preterm | 49 (29) | 26 (53) | ||||
| Respiratory distress | No | 109 (65) | 29 (27) | 2.08 | 1.05-4.09 | 0.03 |
| Yes | 58 (35) | 25 (43) | ||||
| Mechanical ventilation | No | 156 (93) | 46 (29) | 6.37 | 1.61-25.11 | 0.03 |
| Yes | 11 (7) | 8 (73) | ||||
| CPAP ventilation | No | 147 (88) | 48 (33) | 0.88 | 0.31-2.44 | 0.812 |
| Yes | 20 (12) | 6 (30) | ||||
| Birth asphyxia | No | 150 (90) | 48 (32) | 1.15 | 0.40-3.31 | 0.783 |
| Yes | 17 (10) | 6 (35) |
Table 1. Multivariate analysis of neonatal characteristics associated with culture positive sepsis (n=167).
In the present study n=53, 32% neonates had positive sepsis screen (2 or more than 2 parameter of sepsis screen positive). And among them n=28, 53% neonates had positive blood culture (p-value=0.01). Positive sepsis screen had sensitivity of 52%, specificity of 78%, PPV of 53% and NPV of 77%. And in our study AUC for positive sepsis screen is 64.9%, which signifies that positive sepsis screening is reliable indicator of neonatal sepsis.
| Antimicrobial class/agent tested | Activity by microorganism | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Burkholderia cepacia (n=18) | Pseudomonas aeruginosa (n=10) | Non fermenter GNB(n=9) | Klebsiella pneumoniae (n=4) | E.coli (n=3) | ||||||
| R (%) | S (%) | R (%) | S (%) | R (%) | S (%) | R (%) | S (%) | R (%) | S (%) | |
| Penicillin | ||||||||||
| Ampicillin | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| Amoxycillin-clavulinic acid | 89 | 11 | 100 | 0 | 91 | 9 | 100 | 0 | 100 | 0 |
| Piperacillin | 78 | 22 | 40 | 60 | 82 | 18 | 50 | 50 | 67 | 33 |
| Pipercillin -tazobactum | 60 | 40 | 30 | 70 | 70 | 30 | 60 | 40 | 33 | 67 |
| Cephalosporins | ||||||||||
| Cefuroxime | 100 | 0 | IR | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| Cefotaxime | 83 | 17 | 100 | 0 | 100 | 0 | 75 | 25 | 33 | 67 |
| Ceftazidime | 39 | 61 | 30 | 70 | 33 | 67 | 60 | 40 | 100 | 0 |
| Ceftriaxone | 89 | 11 | IR | 0 | 78 | 22 | 100 | 0 | 100 | 0 |
| Cefaperzone-sulbactum | 62 | 38 | 23 | 77 | 100 | 0 | 75 | 25 | 100 | 0 |
| Other beta lactum | ||||||||||
| Imepenum | 67 | 33 | 30 | 70 | 71 | 29 | 0 | 100 | 33 | 67 |
| Meropenum | 40 | 60 | 50 | 50 | 9 | 91 | 0 | 100 | 33 | 67 |
| Aminoglycocides | ||||||||||
| Gentamicin | 88 | 22 | 70 | 30 | 89 | 11 | 75 | 25 | 67 | 33 |
| Amikacin | 61 | 39 | 50 | 50 | 55 | 45 | 50 | 50 | 33 | 67 |
| Quinolones | ||||||||||
| Ciprofloxacin | 89 | 11 | 100 | 10 | 100 | 0 | 100 | 0 | 100 | 0 |
| Levofloxacin | 79 | 21 | 100 | 0 | 78 | 22 | 75 | 25 | 67 | 33 |
| Others | ||||||||||
| Colistin | 23 | 77 | 20 | 80 | 44 | 56 | 0 | 100 | 0 | 100 |
| Tigecycline | 38 | 62 | 30 | 67 | 22 | 78 | 0 | 100 | 0 | 100 |
| Cotrimoxazole | 27 | 73 | 90 | 10 | 87 | 23 | 25 | 75 | 33 | 67 |
| Polymyxin -B | 89 | 11 | 20 | 80 | 77 | 23 | 25 | 75 | 33 | 67 |
| Aztreonam | 62 | 38 | 70 | 30 | 66 | 44 | 25 | 75 | 33 | 67 |
Table 2. Antimicrobials activity pattern of gram negative culture isolates in study group.
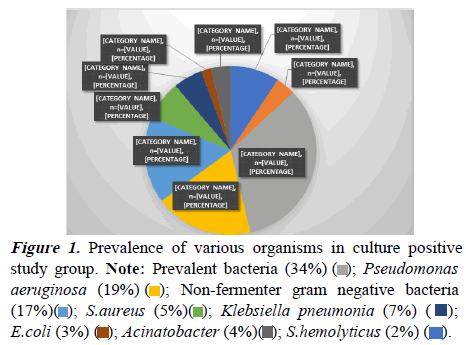
Above figure shows that in the present study among the culture positive isolates Burkholderia cepacia was most prevalent bacteria n=18 (34%), followed by pseudomonas aeruginosa (n=10, 19%), non-fermenter gram negative bacteria (n=9, 17%), S.aureus (5%) (n=5), Klebsiella pneumonia (n=4, 7%), E.coli 6% (n=3), Acinatobacter (n=2, 4%) and S. hemolyticus CONS (n=1, 2%).
In the present study among the culture positive isolates (n=28, 52%) were Multi Drug Resistant organism (MDR). Non fermentar gram negative bacteria shows maximum 78% MDR followed by Burkholderia cepacia (67%), E. coli (67%), Klebsiella pneumoniae (50%), Acinatobacter (50%) and Pseudomonas aeruginosa (40%) (Table 3).
| Antibiotics class/agent tested | Activity by organisms | |||
|---|---|---|---|---|
| Staph aureus (n=5) | Staph.heamolyticus(n=2) | |||
| R (%) | S (%) | R (%) | S (%) | |
| Penicillin | ||||
| Benzylpenicillin | 100 | 0 | 100 | 0 |
| Oxacillin | 100 | 0 | 100 | 0 |
| Cephalosporins | ||||
| Cefoxitin | 60 | 40 | 50 | 50 |
| Quinolones | ||||
| Ciprofloxacin | 80 | 20 | 100 | 0 |
| Levofloxacin | 60 | 40 | 50 | 50 |
| Aminoglycosides | ||||
| Gentamicin | 80 | 20 | 100 | 0 |
| Amikacin | 60 | 40 | 50 | 50 |
| Macrolides-lincosamide | ||||
| Erythromycin | 80 | 20 | 100 | 100 |
| Clindamycin | 60 | 40 | 100 | 0 |
| Glycopeptides | ||||
| Vancomycin | 20 | 80 | 0 | 100 |
| Teicoplanin | 0 | 100 | 0 | 100 |
| Others | ||||
| Cotrimoxazole | 20 | 80 | 50 | 50 |
| Chloramphenicol | 100 | 0 | 100 | 0 |
| Tetracycline | 60 | 40 | 100 | 0 |
| Linezolid | 20 | 80 | 0 | 100 |
Table 3. Antimicrobials activity pattern of prevalent gram-positive culture isolates in study group.
Discussion
Neonatal sepsis is significant cause of morbidity and mortality among neonates worldwide. World Health Organization has estimated that 1.6 million deaths occur globally every year due to neonatal infections and 40% of all neonatal deaths occur in developing countries [3]. In India, the incidence of blood culture proven sepsis was reported as 8.5 per 1,000 live births, as per the national neonatal perinatal database. It was found that sepsis is one of the commonest causes of neonatal mortality contributing to 19% of all neonatal deaths. Antibiotic resistance is an emerging problem in Neonatal Intensive Care Units (NICU) particularly in developing countries. The spectrum of organisms that cause neonatal sepsis changes from time to time and varies from region to region.
Hence continuous surveillance for antibiotic susceptibility, rational use of antibiotics and the strategy of antibiotic cycling can provide some answers to it [9]. In this study 26% neonates had birth weight >2500 g (normal), 57% neonates had weight 1500-2499 g Low Birth Weight (LBW) and 17% neonates had birth weight <1500 g Very Low Birth Weight (VLBW). There is preponderance of LBW neonates in the present study. Mean birth weight was 1910 g. A study conducted by Rashmi et al. [10] in Karnataka there were 49% neonates were of birth weight >2500 g (normal), 30% (n=33) neonates were of birth weight 1500-2499 g (LBW) and 11% neonates were of birth weight <1500 g (VLBW). Present study had more LBW neonates than this study. In the present study out of 167 neonates enrolled with neonatal sepsis, 32% (n=54) had positive blood culture and 68% had negative blood culture.
A study conducted by Dipak et al. [11] in Maharashtra found that among 292 cases of neonatal septicemia, 37% had positive blood culture whereas in 63% had blood negative culture. Above study is in accordance with present study. In our study out of 167 neonates enrolled, 17% had Very Low Birth Weight (VLBW) and Among VLBW neonates 46% had culture positive sepsis which is statistically highly significant (pvalue= 0.045). So VLBW is an important risk factor for developing culture positive sepsis. The rate of infection is inversely proportional to the birth weight and low IgG levels due to impaired cellular immunity in low birth weight neonates contributes to the to the increased susceptibility to infection in these neonates [12]. Roy et al. [13] their study in New Delhi found that out of 50 cases of blood culture positive neonatal sepsis 36% were low birth weight and this was statistically significant (p-value=0.008).
In present study out of 167 enrolled neonates, 35% had respiratory distress, 11% had apnea, 11% had altered consciousness due to birth asphyxia, 1.79% had GI bleeding and 1.79% had sclerema in decreasing order. Out of 34% neonates who had respiratory distress 43% had positive blood culture. This finding is statistically highly significant (pvalue= 0.03). Respiratory distress has been the predominant clinical finding for neonatal sepsis in the present study. Pokhrel et al. [14] in their study in Nepal found that out of 336 neonates enrolled with neonatal sepsis, common clinical finding observed at admission were respiratory distress (79.7%), tachycardia (60.9%), cyanosis (59.4%) and hypothermia (53.6%). In the present study 167 neonates were enrolled, among them 32% had culture proven sepsis. In the culture isolates gram negative organisms (87%) were commonest. Burkholderia cepacia was the most prevalent bacteria 34% followed by Pseudomonas 19%, non-fermenter GNB 17% Klebsiella 7%, E.coli 6%, Acinatobacter species 4%.
Burkholderia cepacia showed maximum resistance against Ampicillin (100%) and cefuroxime (100%) followed by amoxycillin clavulanic acid (89%), ceftriaxone (89%), ciprofloxacin (89%), gentamicin (88%), cefotaxime (83%), piperacillin (78%), cefaperazone-sulbectum (62%) and amikacin (61%). Burkholderia cepacia showed sensitivity to colistin (77%), cotrimoxazole (73%) followed by tigecycline (62%), meropenem (60%), ceftazidime (60%), piperacillin-tazobactam (40%). In the present study Staph.aureus showed maximum resistance to benzyl penicillin (100%), oxacillin (100%) chloramphenicol (100%) followed by, ciprofloxacin (80%), gentamicin (80%), erythromycin (80%), cefoxitin (60%). Staph.aureus showed sensitivity to teicoplanin (100%), linezolid (80%), vancomycin (80%), ceftazidime (67%), piperacillin-tazobactam (70%).
A similar study done by Pathak et al. [15] in Ujjain found that S.aureus was resistant to ciprofloxacin (58%), clarithromycin (16%), clindamycin (11%), gentamycin (19%), amikacin (13%), tetracyclines (23%), doxycycline (20%) and co-trimoxazole (51%). in the present study among the culture positive isolates, 52% (n=28) were Multi Drug Resistant organism (MDR). Non fermenter GNB shows maximum 78% MDR followed by Burkholderia 67% E.coil 67%), Klebsiella (50%), Acinatobacter spp. (50%) and Pseudomonas (40%). Similar study conducted by Rath et al. [16] in Odisha found that out of 73 culture positive neonatal sepsis case 66% (n=33) were multi drug resistant. 81% of Klebsiella spp, 60% of Acinetobacter spp. And 100% of Burkholderia were multidrug resistant.
Conclusion
Neonatal sepsis is systemic infection of neonates that is associated with haemodynamic changes and other clinical manifestations in first month of life. It encompasses various systemic infections of newborn such as septicemia, meningitis, pneumonia, arthritis, osteomyelitis and urinary tract infection. Total 167 neonates were enrolled in study with clinical features of neonatal sepsis. The incidence of culture proven sepsis in present study is 32%. Neonates with respiratory distress syndrome had significant association with development of culture proven sepsis. Preterm neonates were more prone (56%) for culture positive Burkholderia sepsis as compared to term neonates (44%). Almost all the gram-negative bacteria showed 100% resistant to ampicillin, amoxycillin/clavulanate, third generation cephalosporins (cefuroxime and ceftriaxone).
Burkholderia which was most common gram-negative organism in present study showed sensitivity to colistin, cotrimoxazole, tigecycline, and meropenem. Staphylococcus aureus was the most common gram positive organism, showed maximum resistance against benzyl penicillin, oxacillin, ciprofloxacin, gentamicin and erythromycin but showed sensitivity to teicoplanin, vancomycin and linezolid. This study determined the incidence, onset, risk factors, and causative agents for neonatal sepsis in resource constrained settings in India. Careful measures have to be taken to overcome the change in trend of organisms causing sepsis, and selection of antibiotics should be prudent. Every NICU should develop their antibiogram in order to have appropriate antibiotic stewardship and decrease incidence of MDR.
Limitations
More studies are needed to study the effect of interventions on the modifiable risk factors for neonatal sepsis. Due to the small sample size results cannot generalized.
Recommendation
The results of the present study will be used to design and implement an antibiotic stewardship policy and introduce interventions to reduce neonatal sepsis in our settings. Proper aseptic precaution while using endotracheal intubation and mechanical ventilation.
Acknowledgement
Authors would like to thank all study participants for their valuable time. Authors would like to extend their gratitude to the staffs of the Department of Pediatrics, RD Gardi Medical College, Ujjain, MP for their contributions and technical supports.
Funding
No funding sources.
Conflict of Interest
None declared.
Ethical Approval
The study was approved by the Institutional Ethics Committee RD Gardi Medical College, Ujjain, MP.
References
- Schaffner J, Chochua S, Kourbatova EV, et al. High mortality among patients with positive blood cultures at a children’s hospital in Tbilisi, Georgia. J Infect Dev Ctries 2009; 3: 267–72.
- Kaistha N, Mehta M, Singla N, et al. Neonatal septicemia isolates and resistance patterns in a tertiary care hospital of North India. J Infect Dev Ctries 2009; 4: 55–7.
- Sundaram V, Kumar P, Dutta S, et al. Blood culture confirmed bacterial sepsis in neonates in a North Indian tertiary care center: Changes over the last decade. Jpn J Infect Dis. 2009; 62(1): 46-50.
- Network NN. National Neonatal-Perinatal Database Report. 2002-2003.
- Cohen ML. Epidemiology of drug resistance: Implications for a post-Antimicrobial era. Science. 1992; 257(5073): 1050-5.
- Dhaneria M, Jain S, Singh P, et al. Incidence and determinants of health care-associated blood stream infection at a neonatal intensive care unit in Ujjain, India: A prospective cohort study. Diseases 2018; 6(1): 14.
- Ramesh A, Ashok D, Vinod P, et al. AIIMS protocols in neonatology second edition. (2nd edn) 2019.
- Clinical and Laboratory Standards Institute (CLSI). Performance standard for antimicrobial disk susceptibility testing. Twenty First Informational Supplement; ClSI: Wayne, PA, USA, 2011; M100-s21.
- Shrestha S, Adhikari N, Rai BK, et al. Antibiotic resistance pattern of bacterial isolates in neonatal care unit. JNMA J Nepal Med Assoc. 2010; 50(180): 277-81.
- Rashmi P, Praveen BK. Clinico-bacteriological profile of neonatal sepsis. Int J Contemp Pediatr 2019; 6(2): 796-802.
- Deepak M, Aziz F, Agrawal G. Clinico-bacteriological profile and antibiotic sensitivity pattern of neonatal septicaemia-A prospective observational study. Int J Cur Res Rev 2015; 7(5): 13.
- Arpita jigar Shah Summaiya A. Mulla, Sangita B. Revdiwala. Neonatal sepsis: High antibiotics resistance of the bacterial pathogens in a neonatal intensive care unit of a tertiary care hospital. J Clin Neonatol 2012; 2(1): 72.
- Roy RD, NCDC D. Risk factors and outcome analysis of gram-positive and gram-negative neonatal sepsis: A case-control study. Canadian Journal of Infection Control. 2017; 32(2): 98-103.
- Pokhrel B, Koirala T, Shah G, et al. Bacteriological profile and antibiotic susceptibility of neonatal sepsis in neonatal intensive care unit of a tertiary hospital in Nepal. BMC Pediatr 2018; 18(1): 208.
- Pathak A, Marothi Y, Kekre V, et al. High prevalence of extended-spectrum β-lactamase-producing pathogens: Results of a surveillance study in two hospitals in Ujjain, India. Infect Drug Resist 2012; 5: 65.
- Rath S, Panda S, Nayak M, et al. Blood culture positive sepsis and sensitivity pattern in a tertiary care neonatal centre in eastern India. International Journal of Contemporary Pediatrics. 2019; 6(2): 487.
 ); Pseudomonas
aeruginosa (19%) (
); Pseudomonas
aeruginosa (19%) ( ); Non-fermenter gram negative bacteria
(17%)(
); Non-fermenter gram negative bacteria
(17%)( ); S.aureus (5%)(
); S.aureus (5%)( ); Klebsiella pneumonia (7%) (
); Klebsiella pneumonia (7%) ( );
E.coli (3%) (
);
E.coli (3%) ( ); Acinatobacter (4%)(
); Acinatobacter (4%)( ); S.hemolyticus (2%) (
); S.hemolyticus (2%) ( ).
).