Research Article - Journal of Anesthetics and Anesthesiology (2017) Journal of Anesthetics and Anesthesiology
Strategic and operational aspects of the Jeovah?s witness patient?s candidates for deceased-donor kidney transplant
- *Corresponding Author:
- Luca Guzzetti
Anesthesia and Palliative Care Unit University Hospital of Varese Italy
Tel: 00393664867525
E-mail: luca.guzzetti@hotmail.it
Accepted date: February 23, 2017
Citation: Bacuzzi A, Guzzetti L, Alicino V, et al. Strategic and operational aspects of the Jeovah?s witness patient?s candidates for deceaseddonor kidney transplant. J Anest Anesthes. 2017;1(1):1-5.
Abstract
Introduction: The correct perioperative management of Jehovah's Witness candidate for kidney transplant is a complex clinical and organizational effort for the whole team involved, to ensure patient safety, transplanted organ survival and respect for the religious motivation.
Aim: This protocol aims to provide a shared and agreed pathway for the evaluation and management of the Jehovah’s witness patients with end-stage chronic kidney disease, candidates for kidney transplant from cadaveric donor.
Material and Methods: An extensive medical literature search was performed using search engines through keywords like 'Jehovah's witness', 'blood transfusion, 'kidney transplant' and 'blood refusal' to create a pathway for the evaluation and management of the Jehovah's witness patients with end-stage chronic kidney disease, candidate to kidney transplant from cadaveric donor.
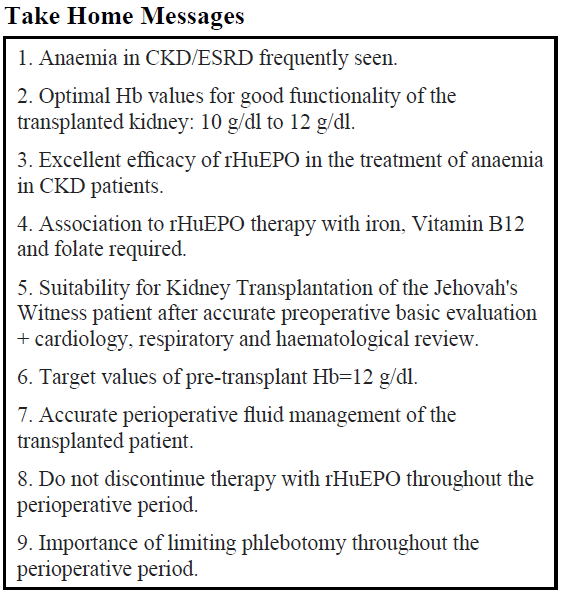
Results: We developed a treatment protocol for Jehovah’s Witness patients undergoing kidney transplant in our University Hospital. Surgical suitability is obtained after an accurate preoperative basic evaluation, in addition to cardiology, respiratory and haematological review. Excellent efficacy of rHuEPO associated with iron, vitamin B12 and folate in the treatment of anemia in CKD patients.
Conclusion: The implementation of this specific protocol ensures patient safety with low rate of perioperative complications.
Keywords
Jehovah's Witnesses, Blood transfusion, Ethical/moral conflict, Blood refusal, rHuEPO
Introduction
The perioperative management of the Jehovah's Witness patient presents complex ethical, legal and medical issues. The refusal of whole blood, packed red blood cells, platelets, plasma, and autotransfusion of pre-deposited blood, creates a frustrating dilemma for the physician, since a routine procedure and potentially lifesaving is considered unacceptable to the patient [1]. The correct management of Jehovah's Witness is a complex clinical and organizational effort for the whole team involved, to ensure patient safety, transplanted organ survival and respect for the religious motivation.
Materials and Methods
We have performed a systematic revision of literature to create an approach to kidney transplant procedures for Jehovah’s witness patients in our hospital. We have underlined the following concepts: religious foundations underlying the refusal of blood transfusions, the current strategies haemo-conservative for bloodless surgery, definition of anaemia and pathogenesis of anaemia associated with chronic renal failure. It is crucial to identify some unique aspects as transfusion requirements in kidney transplantation, definition of minimum threshold of Hb for the efficient operation of the kidney and to prevent myocardial ischemic events.
On this basis, we have developed a clinical protocolcorporate organizational which is divided into the following points: 1) the preoperative evaluation of Jehovah's Witness patient’s candidates to Renal Transplantation. 2) the concept of maximizing erythrocytes production and identification of target value of preoperative Hb for Jehovah's Witness patient’s candidates to renal transplant in order to prevent adverse events.
Discussion
Bloodless surgery: Overview
Some patients in our Trasplant Surgical Department present several preoperative, intraoperative and postoperative challenges. Jehovah's Witnesses are a religious organization whose members believe that the Bible is the true Word of God [2]. The Witnesses began as a small Bible study group led by Charles T. Russell in the late 1870's near Pittsburgh, Pennsylvania. Originally called "International Students of the Bible" or "Russellites", they took its current name, adopted in 1931. Jehovah's Witnesses have always based their beliefs on a literal interpretation of the Bible. They believe that all hope of eternal life or salvation is forfeited if they do not adhere strictly to the dictates of the Bible. In this regard, Jehovah's Witnesses are deeply committed to the tenets of their beliefs, which include the rejection of blood transfusions. The Witnesses' that the blood transfusion violates the law of God was established in 1945 and is based on the following passages from the Bible [3].
“Everything that lives and moves about will be food for you. Just as I gave you the green plants, I now give you everything.4 But you must not eat meat that has its lifeblood still in it.” Genesis 9:3-4
“Any Israelite or any foreigner residing among you who hunts any animal or bird that may be eaten must drain out the blood and cover it with earth, 14 because the life of every creature is its blood. That is why I have said to the Israelites, “You must not eat the blood of any creature, because the life of every creature is its blood; anyone who eats it must be cut off.” Leviticus 17:10-16.
“It seemed good to the Holy Spirit and to us not to burden you with anything beyond the following requirements: 29 You are to abstain from food sacrificed to idols, from blood, from the meat of strangled animals and from sexual immorality. You will do well to avoid these things.” Acts 15:28-29.
Regardless of the circumstances, the Jehovah's Witness believes the biblical injunctions concerning blood [4,5]. Even the use of his own blood, collected and deposited in a blood bank in preparation for a planned surgery, is prohibited [6,7]. During surgery they strongly deny the administration of whole blood, and the use of pre-deposited autologous blood. On the other hand they accept the administration of crystalloid, colloid and recombinant products as rHuEPO and coagulation factors. Many of them accept the administration of albumin, hemodilution and intra and post-operative cell salvage.
Actually in the surgical field there is a growing awareness of the dangers associated with blood transfusions. There are, no doubt that, despite progress, we are not yet able to eliminate the post-transfusion complications yet [8]. There still are some apprehensions regarding the transfusion-related risk of infection caused by known virus-(Hepatitis and HIV) [9] and has by unfamiliar infectious agents (prions causing Creutzfeld- Jacob disease) [10]. In many clinical trials, transfusions were associated with increased relapse and reduced survival in patients undergoing surgery for malignancy [11] and have also been implicated in the genesis of postoperative infectious complications, both in patients undergoing abdominal [12] and orthopedic [13] surgery. More recently it has been proved that peri-operative transfusions are an independent risk factor in the post-traumatic "Multiple Organ Failure" [14]. International experience on Jehovah's Witnesses showed how it is possible to avoid blood transfusions even in difficult circumstances, applying appropriate therapeutic strategies [15]. The analysis of the data published on Jehovah's Witnesses undergoing major surgery without blood transfusion has proved that transfusion refusal adds a mortality risk from anaemia estimated approximately between 0.5% and 1.5%. However each transfusion is potential cause of adverse mild to severe reactions estimated in 20% of cases [16]. The morbidity and mortality resulting from transfusions probably outweigh the risks arising from the refusal of transfusion [17].
The integration and multidisciplinary approach to the problems of the patient in this assessment is the key to deciding the suitability for surgery. It is crucial to evaluate cardiological status in patients candidabile to kidney transplantation, considering their pathophysiological peculiarities (Chronic Kidney Disease and End Stage Renal Disease). Considering the frequent association of anaemia with CKD and the posttransplant anaemia (PTA), the Jehovah's Witness patient’s candidates for kidney transplantation should be evaluated and treated for the peri-operative correction of Hb values. The correction applies not only to the overall benefits associated with the correction of anaemia but also to tolerate perioperative blood loss without reaching Hb values compromising the transplanted kidney functionality. For the treatment of anaemia in CKD the Erythropoiesis-stimulating agents (ESA) have been used since 1980, represented by the different molecules of recombinant human erythropoietin (rHuEPO) that have replaced the use of RBC transfusions and steroids [18]. In the early studies performed on patients with CKD the use of rHuEPO was associated with an improved quality of life [19,20]. Following studies have pointed up the risk of hypertension, ischemic events, loss of vascular access and hyperkalaemia [21] in the case of inappropriate use of rHuEPO (tended to increase over the values of Hb). However, considering the connection between CKD and cardiovascular disease, other studies have shown that anaemia in patients with CKD causes left ventricular hypertrophy, diastolic dysfunction and congestive heart failure [22]. Correction of anaemia with rHuEPO is capable of stopping and reversing these cardiac complications not without possible cardiovascular complications [23]. Treatment of anaemia should therefore be addressed to achieve levels of preoperative Hb of 12 g/dl, not exposing to additional risks (from exaggerated correction with recombinant erythropoietin) and generally sufficient, in a perspective of careful perioperative management, to secure the post-operative value that does not compromise renal graft functionality. The use of ESAs (rHuEPO) is effective and safe for the treatment of anaemia associated with CKD. The efficacy of rHuEPO depends on the availability of iron. The integration of iron, folate and vitamin. B12 are almost always required during administration of rHuEPO. There is the possibility of an immediate perioperative administration of rHuEPO in the Jehovah's Witness patients.
You should make every effort to bring the patient to the operating table with the best possible set-hematology. In this regard, as the Jehovah's Witnesses reject the pre-deposit, several authors have found maximize preoperative hemoglobin levels, by preceding surgeries cycles of 3-4 weeks of therapy with erythropoietin and iron. It has been demonstrated in all areas of surgery, that the administration of recombinant erythropoietin in the perioperative period increases hemoglobin concentration and helps to prevent post-operative anaemia. The stimulation of erythropoiesis is made evident by the increase in reticulocyte count in the third day of treatment. The equivalent of a unit of blood is produced within a week, while the equivalent of five units is produced in 28 days. Therefore, the therapy of four weeks with EPO produces a rate of erythropoiesis equal to 2.5 times the normal value and allows you to plan interventions in which both a predictable loss of blood is equal to 5 unit [24]. The importance of adequate preparation was highlighted by the publication of the work on liver transplants performed without the use of blood and blood products [25].
A logical approach to kidney transplant in Jehovah’s witness
The minimum value of Hemoglobin under which the transfusion is indicated has been recently reviewed and it is now widely accepted to be evaluated on the individual patient. In the absence of cardiovascular and respiratory issues the target of 7 g/dl are acceptable. Moreover, the use of invasive and noninvasive cardiovascular monitoring techniques allows us to define accurately the need to transfuse red blood cells. The administration of recombinant human erythropoietin before surgery, cell salvage techniques and the meticulous surgical technique have a key role for saving the blood. Anaemia is defined on Hb value less than 11 g/dl for pregnant women and children between 6 months and 5 years of age, 12 g/dL for nonpregnant women, to 13 g/dl for men [26]. The classification of the National Kidney Foundation defines 5 stages of Chronic Kidney Disease; in the 5th stage chronic anaemia is seen in 33% of cases. The prevalence of post-transplant anaemia (posttransplant anaemia-PTA) varies in medical literature between 20% and 70%; this large variability can be partly explained by differences in the diagnostic criteria for anaemia and the interval to the moment of transplantation. [27,28]. In the observational study of Poesen et al. [29] conducted on 391 patients undergoing single kidney transplantation in the period between 2003 and 2009, were evaluated hemoglobin levels and iron metabolism in the immediate post-transplant period and three months after surgery. In this paper, the definition of anaemia, as in the study TRESAM, corresponded to that proposed by the clinical practice guidelines for outpatient surveillance of renal transplant recipients: hemoglobin ≤ 13 g/dl for males and ≤ 12 g/dL for females [30].
The main results of this study are: I) post-transplant anaemia (PTA) is a frequent response, severe anaemia in at least 30% of patients; II) the diagnostic phlebotomy is an important but underrated cause for immediate PTA; III) poor graft function impairment, advanced age of the donor and reduced iron stores are independently associated with low hemoglobin levels at 3 months after transplantation. Perioperative blood loss during kidney transplantation is estimated around 100 ml to 200 ml, also in our department’s experience. The incidence of anaemia pre-transplantation is approximately 68%; in 23% of cases patients were transfused in the operating room and transfusions were not justified in 10% of cases (data not published: our experience). In our department, we have collected data from 2009 to 2010, based of 38 patients (27 males/11 females). 68% of patients were anaemic before surgery, with mean values of Hg=12 g/dl. The minimum average Hg was achieved in VII ^ dd post-op, corresponding to 9.7 g/dl. 65% of patients received transfusions and all transfusions were made for values of Hb >7.0 g/dl. The data considered, just came from a limited observational retrospective analysis of two parameters: changes in Hb and use of RBC in the perioperative period. Other aspects such as comorbidities of patients, use of rhEPO in the preoperative, iron therapy, presence of DGF in the postoperative, intraoperative blood loss, volume of blood by diagnostic phlebotomy in post-op, presence of ischemic heart disease should be also considered in next study. However, it is clear that in 23% of patients transfused in the operating room, using PFC resulted in a substantial loss of blood in only one patient.
The management of hemoglobin, fluid challenge and cardiovascular homeostasis are the cornerstones of the perioperative management of patients undergoing kidney transplantation. As for the identification of a threshold value of hemoglobin below which the survival of the renal graft is in danger, the literature data are not numerous, often related to more general aspects of perioperative fluid therapy and hemodynamic management of transplant patients. In the perioperative management of kidney transplantation, the optimal range of Hb values not compromising the organ function, is between 10.0 and 11.9 g/dl; there is no evidence of advantages for Hb values >12 g/dl. In patients with ischemic heart disease, GRC transfused with Hb values >10 g/dl is an inappropriate procedure. The benefits of transfusion outweigh the risks when the values of Hb <7 g/dl. For Hb values between 8 and 10 g/dl there were several controversies and it is good practice to assess the real need in each case. A major objective of intraoperative management of the patient undergoing kidney transplantation is to maintain a good perfusion pressure and the correction and maintenance of blood volume, often reduced to the pre-transplant dialysis. This is essential to the rapid recovery of function of the renal graft. Immediate diuresis is visible in more than 90% of kidney transplants from living donors (LDKT) and between 40% and 70% of transplants from cadaver donor. Although due to several factors, the increased percentage of delayed graft function (DGF) in the case of transplants from cadaver donor is also motivated by a more difficult management of blood volume in the recipient. The management of intraoperative fluid administration during transplantation is crucial. The kidney transplant can be performed by administering only crystalloid due to the short duration of the intervention, the minimum blood loss and the maintenance of capillary permeability. We are currently missing evidence of better outcomes by administering colloids during kidney transplantation. Currently there is a debate concerning the choice of crystalloid able to ensure the best functional recovery of the transplanted kidney. Apart from the type of crystalloid to use it is important to define the volume of fluid to be infused. De Gasperi et al. [31] showed that infusion of aggressive fluids has to be avoided, ensuring a situation of euvolemia administering 15 ml/kg/h to 20 ml/ kg/h of crystalloids in the intraoperative phase in addition to the replacement of losses. The placement of a central venous catheter and measuring the central venous pressure (CVP) is considered essential for proper intra and post-operative fluid management of the patient [32]. A CVP range of 10 mmHg to 15 mmHg is a reasonable value if the patient underwent a kidney transplant in the absence of severe heart failure, to ensure throughout the surgery and post-operative until the stable recovery of functionality graft.
In this specific context, the hemodynamic monitoring is particularly important as it has to provide the parameters for a real Perioperative Hemodynamic Therapy. The objective of intraoperative anaesthetic management during kidney transplant is to ensure a good blood volume and a good perfusion pressure (Mean Arterial Pressure) providing the best availability of oxygen (DO2-oxygen delivery) for the peripheral tissues (and graft failure in particular). The basic parameters to be considered are ECG continuous monitoring of D2 and V5, Heart Rate, Invasive Blood Pressure and SpO2. These data must also add an indirect index of Oxygen Consumption of peripheral tissues (VO2), represented by the saturation of oxygen in the venous blood of the superior vena cava taken from the central venous catheter (ScvO2) and measurement of blood lactate and values Hb of arterial puncture (arterial blood gas). With this information available, you can follow a -Goal-Directed Therapy (GDT) geared to ensuring MAP>70 mmHg, a PVC between 10 and 15 mmHg, a value of blood lactate between 1 mmol/l and 2 mmol/l and a value Hb>10 g/dl. [33,34]. The preoperative evaluation of the Jehovah's Witness patient candidate for kidney transplantation must stand out from the usual evaluation. The difference lies in the particular attention that must be paid to evaluating cardiac and respiratory. The strict application of the American College of Cardiology/American Heart Association must verify the ability of the cardiovascular system of the patient to deal with transient states of anaemia satisfying the oxygen demands of the peripheral tissues.
Conclusion
The minimum value of Hb under which transfuse in the absence of cardiovascular and respiratory diseases values of Hb=7 g/dl are acceptable.
• Intraoperative is recommended the use of rHuEPO, blood salvage techniques and meticulous surgical technique.
• Anaemia is defined by Hb value of 11 g/dl in pregnant women and children between 6 months and 5 years old; 12 g/dL in non-pregnant women and 13 g/dl for men.
• Iron deficiency is an important factor in the aetiology of post-transplant anaemia (PTA).
• Perioperative estimated blood loss during kidney transplant is around 100 ml to 200 ml.
• In perioperative management, the optimal Hb values, not compromising kidney functionality, are between 10.0 g/ dl and 11.9 g/dl, with no evidence of benefits for values >12 g/dl.
• In patients with ischemic heart disease, RBC transfusion with Hb values >10 g/dl is an inappropriate procedure. The benefits of transfusion outweigh the risks when the values of Hb <7 g/dl. For Hb values between 8 g/dl and 10 g/dl, blood transfusion is controversial and individual assessment of the real need is required.
• Intraoperative fluid therapy should be based on crystalloid. Colloids are useful to expand blood volume. Several hemodynamic monitoring techniques are available to guide perioperative fluid management and to ensure organs oxygenation.
• The multidisciplinary integration in preoperative assessment is the key to confer the suitability of surgery.
• The treatment of anaemia should be addressed to achieve preoperative Hb levels=12 g/dl.
• In our experience, the achieving of preoperative Hb target of 12 g/dl with rHuEPO allows us to perform kidney transplantation in Jehovah's Witness patient (suitably selected) based on an adequate scientific rationale.
The use of rHuEPO is effective and safe for the treatment of anaemia associated with CKD. The integration of iron, Folate and vitamin B12 are always required during administration of rHuEPO.
References
- Dixon JL, Smalley MG. Jehovah's Witnesses: The surgical/ethical challenge. J Am Med Assoc. 1981;246:2471-2.
- Harrison BG. Visions of Glory: A history and memory of Jehovah's witnesses. New York: Simon and Schuster, 1978.
- Jehovah's witnesses and the question of blood. New York: Watchtower bible and tract society of New York. Inc,1977.
- How can blood save your life? Brooklyn: Watchtower bible and tract society, Inc., 1990.
- Jehovah's witnesses and the question of blood. 9 p.
- The truth that leads to eternal life. New York: Watchtower bible and tract society of New York, Inc., 1968.
- Blood transfusions: Why not for Jehovah's Witnesses? New York: Watchtower bible and tract society of New York, Inc., 1977.
- Klein HG. Allogeneic transfusion risks in the surgical patient. Am J Surg. 1995;170(6):21-6.
- Williams AE, Thomson RA, Schreiber GB, et al. Estimates of infectious disease risk factors in US blood donors. JAMA. 1997;277:67-972.
- Busch MP, Glynn SA, Schreiber GB. Potential increased risk of virus transmission due to exclusion of older donors because of concern over CreutzfeldJakob disease. Transfusion. 1997;37:996-1002.
- Blumberg N, Chuang-Stein C, Heal JM. The relationship of blood transfusion, tumor staging, and cancer recurrence. Transfusion. 1990;30:291-4.
- Johanson S, Andersson M. Adverse effects of perioperative blood transfusion in patients with colorectal cancer. Eur J Surg. 1992;158:419-25.
- Koval M, Rosemberg AD, Zuckerman JD, et al. Does blood transfusion increase the risk of infection after hip fracture? J Orthop Tratima. 1997;1:260-6.
- Moore FA, Moore EE, Sauaia A. Blood transfusion. An independent risk factor for postinjury multiple organ failure. Arch Surg. 1997;132:620-5.
- Howell PJ, Bamber PA. Severe acute anaemia in a Jehovah?s witness-survival without blood transfusion. Anaesthesia. 1987:42:44-8.
- Walker RH. Transfusion risk. Am J Clin Pathol. 1987;88:374-8.
- Kítchens CS. Are transfusion overrated? Surgical outcome of Jehovah?s Witnesses. Am J Med. 1993;94:117-9.
- Obrador GT, Roberts WL, Peter WL, et al. Collins, Trends in anaemia at initiation of dialysis in the United States. Kidney Int. 2001;60;5:1875-84
- Benz RL, Pressman MR, Hovick ET, et al. A preliminary study of the effects of correction of anaemia with recombinant human erythropoietin therapy on sleep, sleep disorders, and daytime sleepiness in hemodialysis patients (the SLEEPO study). Am J Kidney Dis. 1999;34(6):1089-95.
- da Revicki RE, Brown DH, Feeny A, et al.Healthrelated quality of life associated with recombinant human erythropoietin therapy for pre-dialysis chronic renal disease patients. AmJ Kidney Dis. 1995;25(4):548-54.
- Winearls CG. Historical review on the use of recombinant human erythropoietin in chronic renal failure. Nephrol Dial Transplant. 1995;10(2):3-9.
- McClellan WM, Flanders WD, Langston RD, et al. Anaemia and renal insufficiency are independent risk factors for death among patients with congestive heart failure admitted to community hospitals: A population-based study. J Am Soci Nephrol. 2001;13(7):1928-36.
- AK Singh, L Szczech, KL, Tang KL, et al. Correction of anaemia with epoetin alfa in chronic kidney disease. New Eng J Med. 2006;355(20):2085-98.
- Goodnough LT, Monk TG, Andriole GL. Erythropoietin therapy. N Eng J Med. 1997;336:933-8.
- Ramos HC, Todo S, Kang Y, et al. Liver transplantation without the use of blood products. Arch Surg 1994;129:528-33.
- Kasiske BL, Vazquez MA, Harmon WE, et al. Recommendations for the outpatient surveillance of renal transplant recipients. J Am Soc Nephrol. 2000;11:S1.
- Vanrenterghem Y, Ponticelli C, Morales JM, et al. Prevalence and management of anaemia in renal transplant recipients: A European survey. Am J Transplant. 2003;3:835.
- Winkelmayer WC, Chandraker A. Post-transplantation anaemia: Management and rationale. Clin J Am Soc Nephrol. 2008;3(2):S49.
- Poesen R, Bammens B, Claes K, et al. Prevalence and determinants of anaemia in the immediate post-kidney transplant period. Transplant Int. 2011;24(12):1208-15.
- Kasiske BL, Vazquez MA, Harmon WE, et al. Recommendations for the outpatient surveillance of renal transplant recipients. J Am Soc Nephrol. 2000;11.
- Gasperi A, Narcisi S, Mazza E, et al. Perioperative fluid management in kidney transplantation: Is volume overload still mandatory for graft function? Transplant Proc. 2006;38:807-9.
- Sarinkapoor H, Kaur R, Kaur H. Anaesthesia for renal transplant surgery. Acta Anaesthesiol Scand 2007;51:1354-67.
- Brienza N, Giglio MT, Marucci M, et al. Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study. Crit Care Med. 2009;37(6):2079-90.
- Mikhail Y, Kirov, Vsevolod V,et al. Perioperative haemodynamic therapy. Current Opinion in Critical Care.2010;16:384-92.