Research Article - Biomedical Research (2017) Volume 28, Issue 10
Radiofrequency ablation Habib-4X in the clinical application of spleen preservation surgery
Junzhong Shi, Huijun Sun, Yijun Wang, Jianbin Zhuang*, Licheng Zhang and Xiaojiang Liu
Tianjin Institute of Hepatobiliary Diseases, Tianjin Key Laboratory of Artificial Cells, Department of General Surgery, the Third Central Hospital of Tianjin, Tianjin, PR China
- *Corresponding Author:
- Jianbin Zhuang
Tianjin Institute of Hepatobiliary Diseases
Tianjin Key Laboratory of Artificial Cells
Department of General Surgery
Third Central Hospital of Tianjin, PR China
Accepted date: February 25, 2017
Abstract
Objective: To evaluate the effects of radiofrequency ablation Habib-4X for patients with splenic tumor or injury to repair their damage.
Methods: The clinical effect of splenectomy in 80 patients with splenic tumor or injury was analysed retrospectively from July 2010 to September 2016. Of these, 40 patients who received radiofrequencyassisted splenectomy (RP group) were compared to 40 patients who had splenectomy without ablation (RN group). Use factors operative timethe amount of bleeding lose and the rates of complication to compare efficacies while detect platelet level at 5, 10, 15, 20 and 30 days after surgery to determine the effect for immune system.
Results: The operative time, blood lose and the complication rate in the RP group is significantly lower than that in RN group (P<0.05), however the platelet level in the RN group is significantly higher than the RP group (P<0.05) from day 5 to day 20. All the patients were stable in the operation and did not need to stay in the ICU.
Conclusion: Splenectomy with radiofrequency ablation Habib-4X is safer and more reliable than conventional splenectomy, which not only reduces the difficulty of operation, but also improves the success rate of operation. So most of the patients’ spleen function can be preserved and avoid long-term severe infection occurs, which deserves promotion to promote the preservation of spleen surgery in clinical.
Keywords
Radiofrequency ablation, Habib-4X, Spleen preservation, Clinical application
Introduction
Radiofrequency (RF)-assisted technology, which consists of adequate irrigation with saline combined with RF irradiation, allows the surgeon to coagulate the parenchyma before transaction, resulting in a virtually bloodless procedure. And some papers reported that this technology was applied to parenchymal transection in hepatectomies to reduce blood loss [1]. Recently, a lot of research is focused on the liver resection in order to reduce bleeding [2-4]. Radiofrequency-assisted hepatectomy was first described by Weber et al. [3] who used a single needle probe to deploy RFA energy before liver resection, and the mean blood loss, which has been shown to be effective in reducing intraoperative blood loss; it has been recommended for cirrhotic patients [5,6]. However, Radiofrequency (RF)-assisted technology is rarely reported for spleen resection.
Management of splenic injury has changed dramatically over the past decades with a strong emphasis on spleen preservation rather than splenectomy [7,8]. With the study of the immune function of the spleen, especially its anti-infection, anti-tumor function to be sure, to retain some of the splenic partial resection of the concept and method came into being. At present, the indications for splenectomy are spleen injury and benign tumor of spleen. In spite of the many surgical techniques available for splenectomy in recent decades, extensive resection of the spleen has been limited by the huge risk of intraoperative or postoperative bleeding. To explore a safe and reliable method of spleen-conserving surgery has become a new clinical issue.
Total splenectomy or partial splenectomy is a curative surgery, especially for epithelial cysts because incomplete treatments result in disease recurrence. Considering that partial splenectomy has an immunologic advantage over total splenectomy [9], partial splenectomy should be performed whenever possible for these benign diseases. A key to performing partial splenectomy safely has been control of bleeding during transection of the spleen. Although various techniques including suture control, compression of the spleen, use of an argon beam coagulator, or a stapling technique have been used to prevent bleeding from the cut surface, we present here an alternative procedure using a new device [10].
In recent years, foreign radiofrequency ablation for partial splenectomy received good results [10,11]. However, the use of this technique remains controversial due to few reported perioperative outcomes and complications. Moreover, some studies have suggested that radiofrequency-assisted spleen resection leads to less blood loss, a lower transfusion rate, and less postoperative morbidity and mortality. Some studies have reported that radiofrequency-assisted spleen resection causes severe dysfunction, and the incidence of postoperative complications is higher than that of simple hepatectomy. The safety of radiofrequency-assisted spleen resection is still questioned. Here, from July 2010 to September 2016, the clinical effect of splenectomy in 80 patients with splenic tumor or injury was analysed retrospectively to assess the efficiency and safety of radiofrequency-assisted splenectomy.
Patients and Methods
Patients’ information
From June 2010 to September 2016, a total of 80 patients with benign and malignant spleen tumors were recruited from the Department of General Surgery, the Third Central Hospital of Tianjin. Of these cases, 40 patients received radiofrequencyassisted spleen resection (RP group), and 40 patients had splenectomy without ablation (RN group) [12]. Exclusion criteria: (1) non-benign lesions of the spleen, such as malignant tumors or borderline lesions; (2) splenic pre-resected tissue is too much, is expected to retain the whole spleen 1/3 spleen.
The patients and their families were also asked to give their written consent to the surgery. Patients were fully informed of their conditions and options. They voluntarily chose the surgical approach. This study was consistent with the Declaration of Helsinki. The study was approved by the Research Ethics Committee of the Third Central Hospital of Tianjin.
Operative technique
Three expert surgeons with more than 10 years of splenectomy experience performed the operations. They used the same splenectomy procedure that they had all agreed upon before the operation to minimize the influence of procedure on outcome.
This group of patients were treated with general anesthesia, take the left rib margin large enough oblique incision, in order to facilitate the full integrity of the free spleen. Simple splenic injury patients, the use of blood back to the machine line of autologous blood transfusion, and control of active bleeding (which can temporarily block the spleen). After the complete dissociation of the spleen, the splenic marker line was designed with the argon knife according to the patient's specific circumstances. The Habib 4X electrode needle was inserted into the deepest part of the spleen tissue along the marking line, and the foot switch was started to ablate and solidify the spleen tissue. After the device automatically stops the program-controlled ablation, and a tone. Repeated ablation along the cut-off line in order to repeat more solidification can be automatically finished.
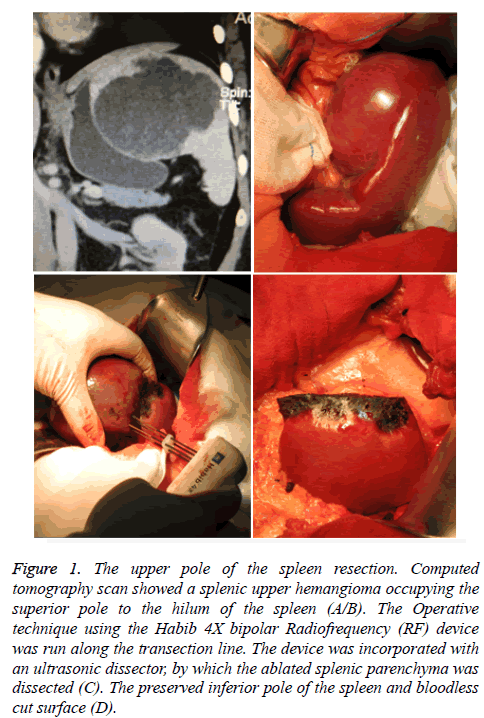
The spleen parenchyma of the spleen was cut into 1.2~1.5 cm wide and the specimens were cut off with a scalpel at 2/3 of the area near the coagulation necrosis. The remaining spleen section had a thickness of 0.8-1.0 cm solidified surface. Interrupted suture ligament spleen, fixed spleen in the spleen bed (Figures 1A and 1B).
Figure 1: The upper pole of the spleen resection. Computed tomography scan showed a splenic upper hemangioma occupying the superior pole to the hilum of the spleen (A/B). The Operative technique using the Habib 4X bipolar Radiofrequency (RF) device was run along the transection line. The device was incorporated with an ultrasonic dissector, by which the ablated splenic parenchyma was dissected (C). The preserved inferior pole of the spleen and bloodless cut surface (D).
A HabibTM 4X bipolar radiofrequency device (Generator 1500X, RITA Medical Systems, Inc. CA, United States) was used to deploy the radiofrequency therapy during operation in the RP group. In the treatment, the surgical electrode directly puncture to the wound site, the start of the RF output, the organization of the polar molecules and ions at the same frequency with the RF current high-speed motion shock generated friction heat, and conduction to the adjacent tissue, the organization internal Heating, evaporation of water inside and outside the cell, dry, shrinkage to achieve the purpose of hemostasis.
Observation indicators
Laboratory measurements were recorded for both groups of patient’s related indicators. Laboratory parameters include platelets in the patient's body (PLT) were recorded. 5 days, 10 days, 15 days and 20 days after operation were recorded 30 d of the PLT, patients with venous blood, through the automatic blood cells in mind recorder measurement. PLT to compare the two surgical methods of coagulation power the impact of energy. Surgery-related parameters, including surgery time, surgery bleeding volume, the day after the intraperitoneal drainage and postoperative complications rate, in order to compare the two groups of spleen-preserving surgery.
Statistical analysis
Continuous data are expressed as either mean with standard deviation or median with range depending on the data distribution. The groups were compared using the t test and Mann-Whitney test for continuous variables and the χ2 test and Fisher’s exact test for proportions. P<0.05 was considered significant. Statistical analyses were performed with SPSS (Version 18.0; SPSS, Chicago, IL, United States).
Results
Patients and splenectomy characteristics
In this study, the splenectomy without ablation (RN group) and radiofrequency-assisted spleen resection (RP group) have enrolled 40 patients, two groups in age (53.2 ± 9.4 vs. 46.2 ± 9.8), body weight (59.7 ± 9.8 vs. 61.2 ± 7.2), gender (27/13 vs. 16/14), type of resection (31/9 vs. 28/12) and other aspects of the difference was not statistically significant (Table 1). A total of 31 (77.5%) minor and 8 (22.5%) major splenectomies were performed in the RP group, and 28 (70.0%) minor and 12 (30.0%) major splenectomies were performed in the RN group. There were no statistically significant differences between the two groups. There was no bleeding during the course of parenchymal transection (Figure 1C). The cut surface of the spleen was hemostatic without the use of suture or other hemostatic techniques (Figure 1D).
| Groups | Age (yr) | Body weight (kg) | Gender (Male/Female) | Type of resection (Minor/Major) |
|---|---|---|---|---|
| RN | 53.2 ± 9.4 | 59.7 ± 9.8 | 27/13 | 31/9 |
| RP | 46.2 ± 9.8 | 61.2 ± 7.2 | 26/14 | 28/12 |
Table 1. Patients and splenectomy characteristics.
Intraoperative variables
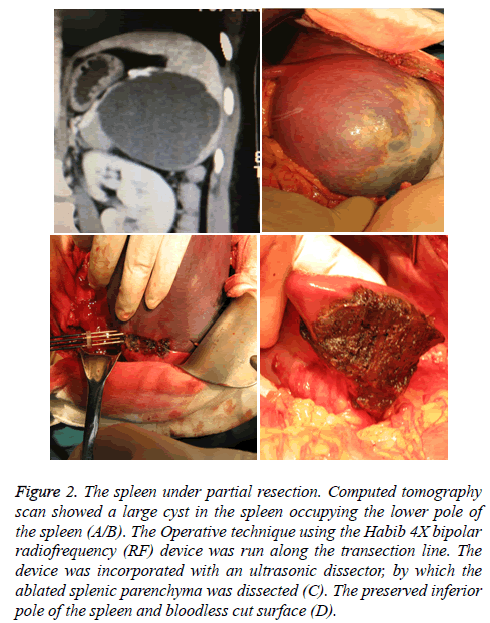
There was significantly less median intraoperative blood loss in the RP group (195.4 ± 20.7 ml vs. 471.5 ± 28.3 ml, P<0.05). In this group of cases, splenectomy was successfully performed without occlusion of the splenic pedicle blood flow with lower blood transfusion requirement than those in the RN group (Table 2). The total operation time was no significant difference between the two groups (171.8 ± 15.3 ml vs. 163.5 ± 17.5 ml, P>0.05). Ablation coagulation necrosis with the formation of the scalpel can be directly off the spleen, spleen section completely without bleeding (Figure 2). All the patients were stable in the operation and did not need to stay in the ICU. There was no significant difference in the overall incidence of postoperative complications between the two groups (7.5 % vs. 2.5 %, P=0.11). The 30 d mortality and hospital stays showed no statistically significant differences between the two groups.
Figure 2: The spleen under partial resection. Computed tomography scan showed a large cyst in the spleen occupying the lower pole of the spleen (A/B). The Operative technique using the Habib 4X bipolar radiofrequency (RF) device was run along the transection line. The device was incorporated with an ultrasonic dissector, by which the ablated splenic parenchyma was dissected (C). The preserved inferior pole of the spleen and bloodless cut surface (D).
| Groups (min) | Operative time (min) | Blood lose (ml) | Transfusion requirement, n (%) | Radiofrequency-assisted time | Complication rate, n (%) |
|---|---|---|---|---|---|
| RN | 171.8 ± 15.3 | 471.5 ± 28.3 | 29 (72.5) | 0 | 3(7.5) |
| RP | 163.5 ± 17.5 | 195.4 ± 20.7 | 11 (27.5) | <15 | 1(2.5) |
Table 2. Intraoperative variables characteristics.
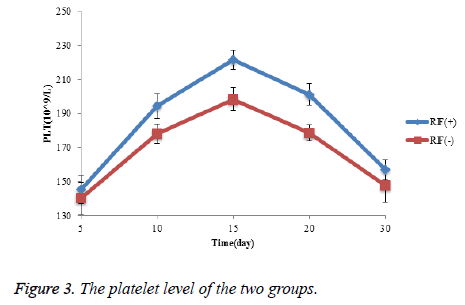
Platelets (PLT) level comparison
In the monitoring of thirty days Postoperative platelets (PLT) level, the platelet levels in the two treatment groups were increased firstly, reached the highest pint and then decreased. From our study, on the fifteenth day, both treatments the platelet content reached the highest level (220 vs. 190). However, the platelet content of the RP group were significantly lower than that of RN group from day 10 to day 20 postoperative, and there are no significant difference compared at day 5 and day 30 (Figure 3).
Discussion
Although various surgical techniques are available for spleen preservation, the result has been less satisfactory because of a significant risk of intraoperative hemorrhage encountered frequently during the procedure [13-15]. Over the last few years, radiofrequency ablation is currently one of the most commonly used technologies in the clinical treatment of spleen preservation. Radiofrequency ablation can not only resect the tumor itself but is also effective in sealing vessels and bile ducts, which can facilitate nearly bloodless spleen resection. The use of radiofrequency ablation devices to perform liver resection was described in 2002 by Weber et al. [3]. A series of studies by different groups confirmed the benefits of radiofrequency-assisted hepatectomy in reducing blood loss [16-18], but there are few studies about splenectomy, especially in clinical applications.
Spleen is the largest human peripheral lymphoid organs, with hematopoietic, immune, filtration, blood storage, regulation and other functions. Splenectomy can lead to severe OPSI (overwhelming post-splenectomy infection) [19], so spleen treatment is the importance of the general surgeon's consensus, where conditions permitting to retain the spleen or spleen tissue, is generally considered to retain at least the normal spleen tissue 1/3 in order to maintain the normal function of the spleen. Usually, partial splenectomy resection due to the real brittleness of the spleen and difficult to stop bleeding, resulting in diverted to complete splenectomy. With the advent of radiofrequency instruments, the use of radiofrequency has been applied to surgery due to hemostasis, which increases the likelihood of successful partial resection of the spleen.
Radiofrequency waves are transmitted to the tissue, causing changes in the direction of the ions, and produce ion kinetic energy and friction heat. Tissue fever causes the water inside and outside the cell detachment from the organization, leading to tissue damage, that tissue coagulation necrosis. The new generation of Habib 4X is a bipolar device that avoids the complications associated with electrical conduction because it eliminates the possibility of conduction damage and does not attenuate the current, thus significantly reducing the time to surgery. Habib 4X is named after its inventor, Professor Nagy Habib of the Imperial College London, and was first reported in 2002 [3]. In 2005, the technology was called Habib technology [20]. Initially as an adjunct hepatectomy technique, clinically achieved great success. In 2009, Hieronymus first reported partial splenectomy with splenic cysts using Habib 4X [21]. This group of patients was not blocked in the case of splenic partial resection successfully completed. Scalp off the spleen parenchyma, no cross-sectional vascular for any clamp, ligation and suture, to retain the spleen section is almost completely bleeding. The use of this technique for splenectomy is desirable because the Habib 4X radiofrequency device can rapidly form a clotted necrotic zone in the spleen plane to be severed, with all vessels being reliably clotted. Traditional partial splenectomy, section of the blood vessels are required to cut off after ligation, cross-section oozing need hot saline gauze pressure cover or argon knife, electric knife spray coagulation, fine line 8 word suture to stop bleeding. Crosssection full of bleeding, still need to close the suture or “U”- shaped interlocking suture. Operation difficult, timeconsuming, intraoperative bleeding is not easy to control, and postoperative secondary bleeding rate, so that a wide range of splenectomy surgery to be limited.
Habib 4X line partial splenectomy should pay attention to the problem RF operation should have enough patience, if the loss of patience at this time, knife cut off the bleeding on the inevitable, multi-point off the integrity of the cross section Ablation, making the cut off from the surface with a scalpel as far as possible without bleeding, so as to avoid postoperative secondary bleeding; met near the splenic segment of the thick blood vessels should be ligation or suture alone, repeated ablation, Easy to damage the spleen pedicle blood vessels, which led to postoperative splenic vein thrombosis, residual splenic insufficiency; retention and removal of coagulation closure zone should be maintained at 2: 1, so that hemostasis more reliable; residual spleen need to be fixed in the spleen bed , To prevent the subsequent occurrence of residual spleen to reverse and walk.
The current recognition of the spleen with an irreplaceable immune function, try to keep the spleen or part of the spleen has become the trend of modern splenic surgery. For the preservation of spleen benign tumor spleen, must have the following conditions: a normal spleen tissue structure; have a good blood supply, preferably with the trunk blood vessels; retained spleen volume of at least 1/3 of the normal. The principle is to ensure the safety of patients under the premise, then consider partial splenectomy.
We believe that, compared with the traditional partial splenectomy, partial splenectomy with Habib 4X line is more scientific, simple, safe and reliable. This technique not only reduces the difficulty of surgery, shorten the operation time, increase the safety of surgery, scientific and reliability, and can improve the success rate of surgery, so that spleen-preserving surgery can be widely carried out in clinical, making the majority of patients Spleen function can be retained, and to avoid long-term serious infection. So the technology has a certain clinical value, it is worthy of application and promotion. After the experience of this surgical technique, in the future can be considered to expand the indications for surgery, such as cirrhosis of the patients with partial splenectomy and renal partial excision of benign tumors.
References
- Sakamoto Y. Bloodless liver resection using the monopolar floating ball plus ligasure diathermy: preliminary results of 16 liver resections. World J Surg 2004; 28: 166-172.
- Feng K. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 2012; 57: 794-802.
- Weber JC, Navarra G, Jiao LR, Nicholls JP, Jensen SL. New technique for liver resection using heat coagulative necrosis. Ann Surg 2002; 236: 560-563.
- Pai M, Jiao LR, Khorsandi S, Canelo R, Spalding DR. Liver resection with bipolar radiofrequency device: Habib 4X. HPB (Oxford) 2008; 10: 256-260.
- Li M. Radiofrequency-assisted versus clamp-crushing parenchyma transection in cirrhotic patients with hepatocellular carcinoma: a randomized clinical trial. Digestive Diseases and Sciences 2013; 58: 835-840.
- Curro G. Radiofrequency-assisted liver resection in cirrhotic patients with hepatocellular carcinoma. J Surg Oncology 2008; 98: 407-410.
- Pachter HL, Grau J. The current status of splenic preservation. Adv Surg 2000; 34: 137-174.
- Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA. Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995; 38: 323-324.
- Jahn S, Bauer B, Schwab J, Kirchmair F, Neuhaus K. Immune restoration in children after partial splenectomy. Immunobiology 1993; 188: 370-378.
- Itamoto T, Fukuda S, Tashiro H, Ohdan H, Asahara T. Radiofrequency-assisted partial splenectomy with a new and simple device. Am J Surg 2006; 192: 252-254.
- Jiao LR, Tierris I, Ayav A, Milicevic M, Pellicci R. A new technique for spleen preservation with radiofrequency. Surgery 2006; 140: 464-466.
- Zhang F. Efficiency and safety of radiofrequency-assisted hepatectomy for hepatocellular carcinoma with cirrhosis: A single-center retrospective cohort study. World J Gastroenterol 2015; 21: 10159-10165.
- Ho CM. Splenic cysts: a new approach to partial splenectomy. Surg Endosc 2002; 16: 717.
- Pareek G. Haemostatic partial nephrectomy using bipolar radiofrequency ablation. BJU Int 2005; 96: 1101-1104.
- Pachter HL, Guth AA, Hofstetter SR, Spencer FC. Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg 1998; 227: 708-717.
- Pai M. Radiofrequency assisted liver resection: analysis of 604 consecutive cases. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 2012; 38: 274-280.
- Daylami R, Kargozaran H, Khatri VP. Liver resection using bipolar InLine multichannel radiofrequency device: Impact on intra- and peri-operative outcomes. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 2012; 38: 531-536.
- Ayav A, Jiao L, Dickinson R, Nicholls J, Milicevic M. Liver resection with a new multiprobe bipolar radiofrequency device. Arch Surg 2008; 143: 396-401.
- Morgan TL, Tomich E. Overwhelming Post-Splenectomy Infection (OPSI): A case report andreview of the literature. J Emerg Med 2012; 43: 758-763.
- Jiao LR, Navarra G, Weber JC, Havlik R, Nicholls JP. Radiofrequency assisted liver resection-a novel technique. Hepatogastroenterology 2005; 52: 1685-1687.
- Hieronymus P. Partial splenectomy for splenic cyst using a bipolar radiofrequency device. Gastroenterology Research 2009; 2: 242-244.