Review Article - Journal of Public Health and Nutrition (2019) Volume 2, Issue 2
Neural correlates in eating disorders: Definition, contexts and clinical strategies.
Giulio Perrotta*Department of Criminal and Investigative Psychology Studies, University of Federiciana, Cosenza, Italy
- Corresponding Author:
- Giulio Perrotta
Department of Criminal and Investigative Psychology Studies
University of Fedriciana
Italy
Tel: +393492108872
E-mail: giuliosr1984@hotmail.it
Accepted date: April 24, 2019
Citation: Perrotta G. Neural correlates in eating disorders: Definition, contexts and clinical strategies. J Pub Heath Catalog 2019;2(2):137-148.
Abstract
Starting from the concept of eating disorders, we proceeded to list the individual forms envisaged by the DSM-V, with a series of focus on clinical, psychodynamic, cognitive-behavioral and strategic profiles, focusing the analysis above all on the resolving context of the problems analyzed.
Keywords
Psychology, Neuroscience, anxiety, Panic, terror, Anxiety disorders, Panic attack, panic disorder, Mericism, avoidant-restrictive eating disorder, Anorexia, bulimia, Binge eating, Amygdala, Prefrontal cortex, Fear, Anxiety, Psychotherapy, Benzodiazepines, Antidepressants, Strategic approach.
Introduction
Eating disorders or psychogenic eating disorders, redefined by the DSM-5 as nutrition and nutrition disorders, are all psychopathological conditions that concern the relationship between individuals and food, with multidisciplinary contours, enter into relationship with psychiatric profiles, endocrinological, gastroenterological and cardiac. They are in fact closely interrelated by the presence of an abnormal relationship with food, by an excess of concern for the physical form, by an altered perception of the body image and by a close correlation between all these factors and the levels of selfesteem, but with different clinical and psychopathological characteristics. Weight, however, is not an essential clinical marker of eating disorders, because even people of normal body weight can be affected by the disease.
These disorders, if not treated in time and with adequate methods, can become a permanent condition and seriously compromise the health of all the organs and systems of the body and, in severe cases, lead to death. Currently, these disorders represent an important public health problem; given that for anorexia and bulimia, in recent decades, there has been a progressive lowering of the age of onset, so much so that diagnoses are increasingly frequent before menarche, up to cases of girls aged 8-9.
The pathology is no longer just for adolescents but it also affects prepubescent children, with much more serious consequences for the body and mind. An early onset can in fact lead to a greater risk of permanent damage secondary to malnutrition, especially for tissues that have not yet reached full maturity, such as bones and the central nervous system. Given their complexity, early intervention is of particular importance; a great collaboration between professional figures with different specializations is essential, for the purposes of an early diagnosis, a timely taking charge within a multidisciplinary path and an improvement of long-term evolution.
It is rather difficult to tell if a friend or family member has developed an eating disorder. The possible signals to take into consideration can be:
• A significant drop in body weight;
• Identification of times when the person lies about how much and when he ate;
• Episodes of excessive ingestion of food in a hurry;
• Continuous episodes in which the person always goes to the bathroom immediately after eating and when he returns he looks reddish in the face;
• The subject trains excessively, almost obsessively;
• Try to avoid eating with others;
• Cut the food into very small pieces or eat extremely slowly;
• Wear loose clothing to hide weight loss.
It can be difficult to ask for help if you have a concern that a loved one may have an eating disorder. People with an eating disorder are often defensive about their way of eating and their weight, and can deny that they are sick. It is very rare that they can figure out for themselves that they have a disorder and that they seek the advice of a therapist. So your role will be crucial to helping them.
The prevalence of nutrition and feeding disorders in young people increases between infancy and early adolescence and between 10 and 13 years of age the symptoms of eating disorders are present in non-clinical populations at levels very similar to those of populations teenagers, moreover, to a greater symptomatology at 9 years corresponds the highest risk of developing a greater symptomatology at 12 years. This suggests how important it is to identify the conditions that favor the development of these disorders well before adolescence.
Eating disorders mainly affect the female population with a ratio of 9: 1 [1], but this relationship weakens in the adolescent phase where the range can narrow to 3: 1 [2]. Adolescence appears to be the period of life with the highest risk of developing an eating disorder, up to 40% of new cases per year [3]. Furthermore, the literature also shows how having eating disorders in adolescence increases the risk that they continue for at least 10 years [4]. 70% of Merican children who attend middle and high schools adopt control methods to maintain weight that are not always suitable such as fasting, vomiting or the use of drugs even without any medical prescription [5]. In a recent work, the Norwegian researcher Klungland-Torstveit studied 2451 adolescents between the ages of 15 and 17 who attended three types of high school: high schools, professional institutes and sports schools [6]. The results of his research show that 55% of the students met the criteria for eating disorders: the significant samples concerned girls and students from vocational schools. In particular, the researcher found that:
• Teenage athletes seem to be the least affected by eating disorders;
• The prevalence of eating disorders is more significant in the female population (64%) than in the male population (45%). Despite this fact, however, the study shows how the gap between the two genders is being reduced (1.4: 1);
• Increases in males the attention towards their own body image;
• Regardless of the presence or absence of eating disorders, there is an increase in the tendency, in both genders, to the repeated use of even particularly restrictive diets.
Beyond this Norwegian study, other studies on populations of Arab adolescents, Mexicans and Iranians agree that overweight or obesity increase the possibility of incurring an eating disorder compared to those who are normal/underweight [7-9].
Even children are not excluded from the plot: already at the age of 6 it is possible to show behaviors that concern attention to one's physical form and appearance. Furthermore the use of diets is frequent in children aged 8 to 13 years.
The female sex is the most affected by eating disorders, it is estimated that the frequency in males is 10 to 20 times lower. In the last thirty years, there has been an increase in interest in the female body and in the "ideal" image that should be aspired according to the canons dictated by fashion, the mass media, magazines, the internet: LEANEST=BEAUTY=PROMISE OF HAPPINESS
The woman of today must be ambitious, successful, beautiful and look as much as possible at the models on the catwalk. In addition to the social and cultural aspects that can partly explain the increased prevalence of eating disorders in women, the biological aspects should not be overlooked. One of these appears to be related to the role of sex hormones in the regulation of serotonin (a neurotransmitter implicated in the regulation of anxiety, mood, impulsiveness and feelings of hunger and satiety). Some studies have found that the reduction of the production of serotonin following a caloric restriction is much more frequent in the female sex, thus confirming the presence of a possible role of female sex hormones or of a difference linked to gender.
However, it has been noted that in recent years, eating disorders are also spreading among the male population. It is
• High comorbidity with psychiatric illnesses (in order of frequency: depression, anxiety, obsessive-compulsive disorder and substance abuse);
• High comorbidity with other medical conditions including gastrointestinal diseases, electrolyte imbalances (sodium, potassium), pulmonary or cardiovascular disorders, Endocrinological alterations, lack of minerals in the skeletal system, neurological or dermatological changes (dry skin or hair loss). In particular, we have seen how subjects suffering from anorexia nervosa are more prone to osteoporosis, fractures and lower back pain;
• Clinical features: restrictive diets, fasting, rituals related to food, excessive concern for one's physical form or weight, excessive control in calorie intake, binge eating with consequent compensatory behavior such as excessive exercise, or vomiting self-induced.
An Australian study then pointed out that in the last few years, purging and binge eating have increased among men [11]. What are the consequences of an eating disorder? It has been found that many people suffering from eating disorders have a low or depressed mood. In addition, many suffer from anxiety that is often associated with food, nutrition, and concerns about weight and body image. Often the thoughts on these issues polarize the attention of the subjects and leave no room for others such as, for example, problems in relationships or low self-esteem. Some studies indicate that one in five anorexic individuals will die due to the aforementioned problems, due to starvation or suicide. Fasting, binge eating, self-induced vomiting, the use and abuse of laxatives can lead to:
• Blood diseases;
• Diseases of the gastrointestinal tract;
• Problems in electrolyte balance;
• Kidney disease;
• Diseases of the cardiovascular system.
A recent study by Jenkins and coworkers pointed out that the severity of symptoms related to eating disorders (poor physical health, limitation in the performance of daily activities, psychosocial stressors) can also significantly affect the quality of life of those suffering from food disorders. In particular, English researchers have stressed the importance of the role played by coping methods and social support. In particular, it emerged that family support and problem-centered coping are very important mediators in improving the quality of life of patients suffering from eating disorders.
Eating disorders are defined in the latest edition of the Diagnostic and Statistical Manual of DSM 5 Mental Disorders «Nutrition and Nutrition Disorders» and are presented in six main diagnostic categories:
• Pica;
• Mericism;
• Avoidant/restrictive eating disorder;
• Nervous anorexia;
• Bulimia nervosa;
• Uncontrolled feeding disorder.
In addition to the above, two residual categories are identified:
• Nutrition disorder or specified diet: these are sub threshold cases of anorexia, bulimia, binge eating disorder as well as disturbance with elimination behaviors and night eating syndrome;
• Nutrition disorder or unspecified diet, i.e. a feeding disorder in which information is missing to specify its characteristics.
The etiopathogenesis of nutrition and nutrition disorders is multifactorial. They are the result of the interaction of predisposing factors (genetic, psychological, environmental and socio-cultural), precipitating factors (restrictive diets and personal psychological difficulties) and maintenance factors (fasting syndrome and positive reinforcement from the environment). The diagnostic classification of nutrition and nutrition disorders takes place on an outpatient basis and requires the patient to be evaluated clinically, nutritionally and psychologically. These are clinical conditions that present high clinical and psychiatric comorbidity that must be investigated. The internal evaluation therefore includes the clinical - anamnestic, nutritional, dietary and energy expenditure assessment. During the clinical-anamnestic evaluation of nutrition and nutrition disorders, a careful anamnestic collection is performed together with the physical examination and the prescription of a series of tests including the urine test, the complete blood count, blood glucose, liver function test, lipid trim, creatininemia, azotemia, BMI. Often clinical observation is preceded by a history of very long illness and this greatly complicates the healing process. If performed correctly, the diagnosis of nutrition and feeding disorders allows the exclusion of other pathologies that can have secondary effects on the relationship with food, such as dysphagia, esophageal and pyloric spasms, dyspepsias, tumoral pathologies, infectious diseases, from substance use and other psychiatric disorders characterized by hyperphagia or hypophagy.
Grogan defined the body image as that set of perceptions, thoughts and emotions that a person experiences about his body [12]. But these perceptions on the body do not always have a positive meaning, nor do they coincide with the ideal bodily form on a subjective level: one speaks in this sense of dissatisfaction with the body image. This dissatisfaction represents one of the major risk and maintenance factors of disorders related to body image and nutrition [13]. Thinness is an instrument through which anorexic and bulimic patients are able, at the same time, to avoid and play, in a more restricted and controllable field, the game of life; the game of research and self-realization in the various areas in which our ambitions and circumstances challenge us, starting with love and work. Faced with the complexity of the challenge, patients with eating disorders retreat in fear and concentrate all their energies on controlling the body's appearance and nutrition. Thus the bodily aspect, from the means we use to live, communicate, present ourselves to the world, becomes a purpose, an end in itself.
According to Fairburn's trans diagnostic perspective, Eating Disorders (DA) or Eating Disorders would share the same psychopathological nucleus: an excessive importance attributed to weight, body shape and nutrition control. Longitudinal studies highlight the diagnostic instability of eating disorders and their migration from one category to another, suggesting that the diagnostic categories of Food Disorders in DSM-5 do not adequately describe the clinical reality. In this perspective, Eating Disorders are considered as a single category, maintained by common mechanisms such as low self-esteem and perfectionism [14]. Other studies have shown that even brooding and control are important maintenance factors for eating disorders [15,16]. In particular, subjects with eating disorders would show a greater tendency to worry about errors (pathological perfectionism), a lower sense of self-esteem, higher measures of brooding and a poor perception of control over external events and internal emotional states, compared to non-pathological subjects. Clinical and experimental evidence supports the hypothesis that perceived criticism is a risk factor for the development of clinical perfectionism in eating disorders. Parental criticism consists in being constantly subject to criticism from others considered significant, important for the person [17,18]. Recent data confirm the hypothesis according to which perceived criticism precedes maladaptive perfectionism in the psychological process, leading to the formation of obsessive control of weight and physical form in the minds of people suffering from eating disorders. In this case, it is possible to imagine the maladaptive perfectionism as a sort of reaction to the extreme pain caused by the criticisms received, which in turn stimulated, in individuals poor in cognitive resources and an adequate family substrate, the development of a control of a control over food, physical form and the fatuity of one's being. It is possible to infer that perceived criticism may be the rational factor that facilitates the trans generational transmission of perfectionism in subjects with eating disorders.
Unlike pathological perfectionism or low self-esteem, control is presented not as a problem, but as a solution. In the case of eating disorders, control is expressed in the control of weight, food and body appearance through diet, and is positively reinforced by the feeling of success that is experienced when it is respected, and negatively by the fear of gaining weight. The result is that, with the intensification of the diet, the weight decreases more and more and the process is self-perpetuating. It is for this reason that the need for control in eating disorders becomes a compulsive necessity, a real obligation. In eating disorders, patients suffer from a general need for control which, before their onset, will probably try to express themselves on more complex and potentially rewarding aspects of life, such as study, work, leisure, relationships or 'affectivity. But these areas soon prove to be too complex and uncontrollable. People with eating disorders feel they are not able to control personal relationships, internal reactions and events in general. To get the perception of control and reach a certain degree of predictability, they are willing to confine their lives within a reduced experience, confined to feeding and body size. However, although the management of food and body size initially offers the attraction of some possibility of control, in the end it condemns them to an isolated and insane existence. For Dalle Grave the tendency to control focuses on nutrition because it provides clear and immediate proof of selfcontrol capacity, because it has a powerful manipulative effect on others and in particular on family members [19].
The main causes of eating disorders are:
• Inheritance;
• Previous slimming diets;
• Problematic family relationships;
• Childhood traumas;
• Sexual violence;
• Transformation of pre-existing anorexia nervosa;
• Tendency to perfectionism combined with a sense of ineffectiveness;
• Low self-esteem;
• Depression;
• Passive style of behavior;
• Weight and line concerns.
• Fashion influences through the media;
• Emphasizing thinness as an attribute of beauty,
• Success and happiness; derision for one's physical appearance in childhood and adolescence.
Individual Eating Disorders According to DSM-5
In May 2013, the American Psychiatric Association (APA) published the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the result of a 14-year review process [20]. The DSM-5 has introduced numerous new features to try to improve the description of the symptoms and behaviors of people who suffer from nutrition and nutrition disorders during their life. The work group on eating disorders that developed the new DSM-5 criteria has set itself the primary objective of minimizing the use of the vague diagnosis "eating disorder not otherwise specified" to ensure that patients receive a diagnosis that accurately describes their symptoms and behaviors - the first step in defining a treatment plan. The main changes relate to having grouped into a single diagnostic category, called nutrition and feeding disorders, nutrition disorders characteristic of childhood and eating disorders, having provided a new definition of nutrition disorders and of nutrition, including new diagnostic categories and modified some diagnostic criteria. A minor change was the abandonment of the Roman numerals to define the DSM editions in favor of the Arabic numerals (from DSM-IV to DSM-5).
The DSM-5 provides the following definition of nutrition and feeding disorders: "Nutrition and nutrition disorders are characterized by a persistent eating disorder or by behaviors connected with diet that determine an altered consumption or absorption of food and that significantly damage physical health or psychosocial functioning ". It should be remembered that the DSM-IV did not provide a definition of eating disorder and this had caused numerous problems in establishing the diagnostic boundary of eating disorders not otherwise specified that did not have positive diagnostic criteria such as anorexia and bulimia.
The DSM-5 includes the following diagnostic categories (the first three mainly concern childhood nutrition disorders):
• Pica;
• Rumination disorder;
• Avoidance/restriction of food intake disorder;
• Bulimia;
• Uncontrolled feeding disorder;
• Nutrition or feeding disorder with specification;
• Nutrition or feeding disorder without specification.
The essential characteristic of pica is to ingest one or more non-nutritive and non-food substances for a period of at least a month. Typically ingested substances vary according to age and availability and may include paper, hair soap. The term "non-nutritive" has been included because the diagnosis of pica should not be applied when food products that have a minimal nutritional content are ingested. Typically there is no aversion to food in general. Furthermore, the ingestion of non-nutritive and non-food substances must also be inappropriate with respect to the level of development of the individual and must not be part of a culturally sanctioned practice. If eating behavior occurs in the context of another mental disorder or medical condition, a diagnosis of pica is made only if the ingestion of non-nutritive and non-food substances sufficiently severe to warrant additional clinical attention. The DSM-5 diagnostic criteria of the pica are as follows:
• Persistent ingestion of substances without food content, inedible for a period of at least 1 month;
• The ingestion of non-edible substances without food content is inappropriate with respect to the individual's stage of development;
• Ingestion behavior is not part of a culturally sanctioned or socially regulated practice;
• If the ingestion behavior occurs in the context of another mental disorder (e.g., intellectual disability - intellectual development disorder - autism spectrum disorder, schizophrenia) or another medical condition is sufficiently severe to warrant further attention clinic.
In remission: Following the previous full satisfaction of the criteria for pica, the criteria were not met for a substantial period of time.
Diagnostic codes: ICD-9: 307.52; ICD-10: F98.3 for children; F50.8 for adults.
Compared to DSM-IV, changes in the diagnostic criteria of rumination disorder have been minimal, except that in DSM-5, this disorder is no longer classified in childhood nutrition disorders, but in the broad diagnostic category "Nutrition and feeding disorders. The rumination disorder requires the regurgitation of food, which can be re-chewed, swallowed again or spit out, for at least 1 month, that the regurgitation is not attributable to an associated gastrointestinal condition or other medical condition, which does not occur during the course of other nutrition and feeding disorders and that if symptoms occur in the context of another mental disorder they must be severe enough to warrant additional clinical attention. The DSM-5 diagnostic criteria of rumination disorder are as follows:
• Repeated regurgitation of food for a period of at least 1 month. Regurgitated food can be re-chewed, growled or spit out;
• Repeated regurgitation is not attributable to an associated gastrointestinal condition or another medical condition (e.g., gastroesophageal reflux, pyloric stenosis);
• The eating disorder does not manifest itself exclusively during the course of anorexia nervosa, bulimia nervosa, binge-eating disorder or avoiding/restricting food intake disorder;
• If symptoms manifest themselves in the context of another mental disorder (e.g., intellectual disability - intellectual development disorder - or other neurodevelopmental disorder) they are sufficiently severe to warrant further clinical attention.
In remission: Following the previous full satisfaction of the criteria for rumination disorder, the criteria were not met for a substantial period of time.
Diagnostic codes: ICD-9: 307.53; ICD-10: F98.21.
Food avoidance/restriction disorder replaces and extends the DSM-IV diagnosis of childhood nutrition disorder. The major diagnostic category of this disorder, which can also be found in adults, is the avoidance or restriction of food intake for three main reasons: 1) apparent lack of interest in eating or food; 2) avoidance based on the sensory characteristics of food; 3) concerns about the adverse consequences of eating. Avoidance or restriction produce a persistent failure to meet the appropriate nutritional and/or energy needs by determining one or more of the following 4 consequences: 1) significant weight loss (or failure to achieve expected weight gain or inadequate growth in children); 2) significant nutritional deficiency; 3) functioning dependent on enteral nutrition or oral supplements; 4) marked interference with psychosocial functioning. There is no concern about body weight and shape, nor should it occur during the course of anorexia nervosa and bulimia nervosa. Finally, the disorder is not due to a lack of food availability or another medical or mental illness. The DSM-5 diagnostic criteria of food intake avoidance/restriction are the following:
• An eating or nutrition disorder (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concerns about the negative consequences of eating) manifested through the persistent inability to satisfy the appropriate nutritional and/or energy needs, associated with one (or more) of the following aspects: significant weight loss (or failure to achieve expected weight gain or discontinuous growth in children); significant nutritional deficit;
• Dependence on parenteral nutrition or oral nutritional supplements;
• Marked interference with psychosocial functioning.
The disorder is not better explained by a lack of food availability or by a culturally sanctioned associated practice. The eating disorder does not manifest itself exclusively during the course of anorexia nervosa or bulimia nervosa and there is no evidence of a disturbance in the way the weight or shape of one's body is experienced.
The eating disorder is not attributable to a concurrent medical condition and cannot be explained by another mental disorder. When the eating disorder occurs in the context of another condition or disorder the severity of the eating disorder exceeds that usually associated with the condition or disorder and justifies further clinical attention.
In remission: Following the previous full satisfaction of the criteria for the avoidant/restrictive intake disorder, the criteria were not met for a substantial period of time.
Diagnostic codes: ICD-9: 307.59; ICD-10: F50.8.
The DSM-5 introduced two important changes in the diagnostic criteria of anorexia. The first is the abolition of the amenorrhea criterion envisaged by DSM-IV because it cannot be applied to males, menopausal women, premenarals and those taking estroprogestinici and due to the fact that some people exhibit all the other signs of anorexia but they continue to menstruate. The second concerns the change of criterion A, which in the DSM-IV required less than 85% compared to what was expected (in practice a BMI <17.5) or the inability to reach the expected weight during growth, while in the DSM -5 a significantly lower weight is required lower than the normal minimum (i.e., BMI <18.5) or, for children and adolescents, lower than the expected minimum (i.e., <5th percentile). Furthermore, the phrase "refusal to maintain body weight above or at the minimum normal weight for age and height" was eliminated because it required the intention of the patient and could be difficult to evaluate objectively. In criterion C the phrase "persistent behavior that interferes with weight gain, even with a significantly low weight" was added. Finally, criteria have been introduced to assess the current severity level based on the BMI. The DSM-5 diagnostic criteria of anorexia are as follows:
• Restriction of calorie intake in relation to needs, which leads to a significantly lower body weight in the context of age, sex, developmental trajectory and physical health. The significantly low body weight is defined as a weight lower than the normal minimum or, for children and adolescents, less than the expected minimum;
• Intense fear of gaining weight or becoming fat, or persistent behavior that interferes with weight gain, even if significantly low;
• alteration of the way in which the individual experiences the weight or shape of his body, excessive influence of body weight or shape on self-esteem levels, or persistent lack of recognition of the gravity of the current underweight condition;
• Restricted type: During the last 3 months, the individual has not presented recurrent episodes of bingeing or elimination behaviors (e.g., self-induced vomiting or inappropriate use of laxatives, diuretics or enteroclisms). In this subtype weight loss is achieved mainly through diet,
• Type with binges/elimination pipelines: during the last 3 months, the individual has presented recurrent episodes of bingeing or elimination behaviors (i.e., self-induced vomiting or inappropriate use of laxatives, diuretics or enteroclisms).
In partial remission: following the previous full satisfaction of the criteria for anorexia, Criterion A (low body weight) was not satisfied for a substantial period of time, but Criterion B (intense fear of gaining weight or becoming fats or behaviors that interfere with weight gain) and Criterion C (alterations of self-perception related to body weight and shape) are still satisfied.
In complete remission: Following the previous full satisfaction of the criteria for anorexia, none of the criteria was met for a substantial period of time.
Current severity level:
• Mild: Body mass index ≥ 17 kg/m2
• Moderate: Body mass index 16-16.99 kg/m2
• Severe: Body mass index 15-15.99 kg/m2
• Extreme: Body mass index <15 kg/m2
• Diagnostic codes: ICD-9: 307.1; ICD-10: F50.01 restrictive
type; F50.02 Type with bulimic seizures/elimination ducts.
DSM-5 maintained the same diagnostic criteria as DSM-IV with the exception of criterion C (frequency and duration of binge eating). It is now required that inappropriate binge eating and compensatory behaviors both occur on average at least once a week for 3 months bulimia, while in DSM-IV they had to check at least twice a week for three months. Furthermore, as with anorexia nervosa, criteria have been introduced to assess the current severity level based on the number of compensatory behaviors per week. Finally, the two subtypes (with and without elimination pipelines) provided for by the DSM-IV have been eliminated. The DSM-5 diagnostic criteria of bulimia are as follows:
• Recurrent binge episodes. An episode of binge is characterized by both the following aspects: eat, over a period of time (e.g., a two-hour period), a significantly larger amount of food than most people would eat at the same time and in similar circumstances.
• Feeling of losing control during the episode (e.g., feeling that you cannot stop eating or controlling what or how much you are eating).
• Recurrent and inappropriate compensatory behavior to prevent weight gain, such as self-induced vomiting, abuse of laxatives, diuretics or other drugs, fasting or excessive physical activity.
• Inappropriate binge eating and compensatory behavior both occur on average at least once a week for 3 months.
• Self-esteem levels are unduly influenced by the shape and weight of the body.
• The alteration does not occur exclusively during episodes of anorexia.
In partial remission: following the previous full satisfaction of the criteria for bulimia, some, but not all, criteria were met for a substantial period of time.
In complete remission: following the previous full satisfaction of the criteria for bulimia nervosa, none of the criteria was met for a substantial period of time; satisfied, none of the criteria was met for an extended period of time.
Current severity level:
• Mild: An average of 1-3 episodes of inappropriate compensatory behavior per week.
• Moderate: An average of 4-7 episodes of inappropriate compensatory behavior per week.
• Severe: An average of 8-13 episodes of inappropriate compensatory behavior per week.
• Extreme: An average of 14 or more episodes of inappropriate compensatory behavior per week.
• Diagnostic codes: ICD-9: 307.51; ICD-10: F50.2.
The binge-eating disorder was included in DSM-5 as a distinct category of eating disorder, while in DSM-IV it was described in Appendix B in the categories that needed further study and could only be diagnosed using the wide diagnostic category " power supply disturbance not otherwise specified”. In DSM-5 binge-eating disorder maintained diagnostic criteria similar to those of DSM-IV with the exception of criterion D (binge frequency and duration). In DSM-5, in fact, binge eating must occur, on average, at least once a week for 3 months, while in the DSM-IV they had to check at least two days a week for 6 months. Furthermore, as with anorexia nervosa and bulimia nervosa, criteria have been introduced to assess the current severity level based on the number of binge episodes per week.
The DSM-5 diagnostic criteria of binge-eating disorder are the following:
• Recurrent bingeing episodes. An episode of binge is characterized by both the following aspects: to eat, in a defined period of time (for example, a period of two hours) a quantity of food significantly greater than that which most individuals would eat at the same time and in similar circumstances;
• Feeling of losing control during the episode (e.g., feeling that you cannot stop eating or controlling what or how much you are eating);
• binge episodes are associated with three (or more) of the following aspects: eat much faster than normal; eat until you feel unpleasantly full; eat large amounts of food even if you don't feel physically hungry; eat alone because of embarrassment about how much you are eating; feeling disgusted with yourself, depressed or very guilty after the episode.
There is a marked discomfort with regard to binge eating. The binge occurs, on average, at least once a week for 3 months. The binge is not associated with the systematic implementation of inappropriate compensatory behaviors such as bulimia nervosa, and does not occur exclusively during bulimia or anorexia.
In partial remission: following the previous full satisfaction of the criteria for binge-eating disorder, binge eating episodes occur with an average frequency of less than one episode per week for a substantial period of time.
In complete remission: following the previous full satisfaction of the criteria for binge-eating disorder, none of the criteria was met for a substantial period of time.
Current severity level:
• Mild: 1 to 3 episodes of binge a week;
• Moderate: 4 to 7 binge episodes per week;
• Severe: 8 to 13 episodes of binge a week;
• Extreme: 14 or more episodes of binge a week.
• Diagnostic codes: ICD-9: 307.51; ICD-10: F50.2.
The category of nutrition or nutrition disorder with other specification applies to presentations in which the characteristic symptoms of a nutrition and nutrition disorder that cause significant distress or impairment in social, occupational or other important areas predominate but they do not meet the full criteria for any of the disorders of the diagnostic class of nutrition and feeding disorders. The nutrition or nutrition disorder category with other specification is used in situations where the clinician chooses to communicate the specific reasons why the presentation does not meet the criteria for any specific nutrition and feeding disorder. This is done by recording "nutrition and feeding disorder with other specification" followed by the specific reason (e.g., "low frequency bulimia nervosa"):
• Atypical nerve anorexia. All criteria for anorexia nervosa are met, except in spite of significant weight loss, the individual's weight is within or above the normal range;
• Bulimia (low frequency and/or limited duration). All criteria are met for bulimia nervosa, except that inappropriate binge eating and compensatory behavior occur, on average, less than once a week and/or for less than 3 months;
• Binge-eating disorder (low frequency and/or limited duration). All criteria are met for binge-eating disorder, except that binge eating occurs, on average, less than once a week and/or for less than 3 months;
• Conduct of elimination disorder. Recurrent elimination conduct to influence body weight or shape (e.g., selfinduced vomiting, improper use of laxatives, diuretics or other drugs) in the absence of binges;
• Night feeding syndrome. Recurrent episodes of night-time eating, which occur when eating after waking from sleep or excessive consumption of food after the evening meal. There is only awareness and I remember eating. Night feeding is not better explained by external influences such as the modification of the sleep-wake cycle of the individual or by local social norms. Night-time feeding causes significant discomfort and/or impairment of operation. Disordered feeding patterns are not better explained by binge-eating disorder or another mental disorder, including substance use, and are not attributable to another medical disorder or drug effect.
• Diagnostic codes: ICD-9: 307.59; ICD-10: F50.8.
The category of nutrition or nutrition disorder with no other specification applies to presentations in which the characteristic symptoms of a nutrition and nutrition disorder that cause significant clinical distress or damage in social, occupational or other important areas predominate, but the full criteria for any of the disorders in the diagnostic class of nutrition and feeding disorders are not met.
The nutrition or nutrition disorder category with other specification is used in situations where the clinician chooses not to specify why the criteria are not met for a specific nutrition and nutrition disorder, and includes presentations where there is insufficient information to make a more specific diagnosis (e.g., in an emergency room setting).
Diagnostic codes: ICD-9: 307.50; ICD-10: F50.9.
Neural Correlates in Eating Disorders
The neuronal circuits involved in dysfunctional food behaviors involve reward regulation systems (satiety and reward), driving (exploration) and craving (impelling desire), evolutionarily highly conserved biological processes that support important human phenomena, from hunger regulation to more sophisticated finalized planning, and therefore cover different transverse mental functions in the expression of behavior, including emotionality as a whole, impulsiveness, compulsiveness and their adequate control. It is not surprising that these pathological conditions almost always combine a double diagnosis, including anxiety and mood disorders, implying a broad psychopathological spectrum.
Even the most authoritative reviews suggest trans-categorical biotechnological investments: the formulation of "personological spectra" would increase the statistical power of relevant multi-variable associations in the complexity of the pathogenesis of nutrition and nutrition disorders. And it is not a methodological tautology, but a scientific strategy to increase the sensitivity of the discovery of haplotypes susceptible to the risk of disease, while sacrificing their specificity (relatively important in terms of technical efficiency, on balance, in the peculiar polysynthromatic symptomatology of nutrition disorders).
The brain presents a systematic organization of the circuits of hunger, the same ones that coordinate sensation seeking in a broad sense (research), including toxicophilias and junipers of addictions (affective, gambling, compulsive shopping, etc.): the prefrontal cortex and the amygdala, among other things, regulates the value of nourishment gratification, the limbic system (insula) processes taste, flavor and hedonic properties, the nuclei of the base mediate the reinforcement of the action and the incentive-motivational levers (because I want or do not want to reiterate an action), the thalamus organizes the responses to the stimuli conditioning self-determination against a food (or any desired goal).
Dysfunctional food behaviors manifest themselves as the phenomenological expression of the constant and progressive interaction of numerous genetic variations, or polymorphisms, and cumulative environmental influences, variables that define them as complex multifactorial pathologies.
If it is true that the epidemiological sources produced by the scientific community agree in recognizing an important familiarity in the susceptibility to the development of nutrition disorders, the meta-analyzes still report contradictory and/or inconclusive data on the role of the single genes involved in risk predisposition [21]. This, in fact, makes the evaluation of the relative weight of the different hereditary components and of the stratified stresses of the experiential environment in the etiopathogenesis very insidious.
The biotechnological and molecular resources invested in the genetics of eating disorders since the 1970s have used different research areas and assorted methods: studies on qualitative and quantitative chromosomal alterations [22], studies on twins [23], studies on family pedigrees, linkage studies [24] case association studies "GWAS" control, specific studies of SNPs and rare variants [25], epigenetic studies [26].
The latter, of rare avant-garde, have the advantage of finally addressing the stubborn dilemma of the genome-environment interaction, in that they shift the research focus from the human genomic code as an automatic entity programmed a priori to an interface in continuous interaction between the baggage of inherited genes and what happens outside - an environment able to modify, influence and determine the expression of the complex genetic machine through different biochemical processes, including chromosomal chromatin methylation. Events external to the DNA have the power to physically change the structure favoring or preventing the transcription of proteins encoded by the genes. However, these are embryonic researches with not a few methodological flaws. For example, at present we are not able to study the methylation patterns of nucleobases of nucleic acids in human neurons for obvious ethical reasons, what has been collected so far from observation on blood or buccal cells.
The inconsistency and contradictory nature of the literature data obtained so far depend on heterogeneous sampling methodologies (different criteria for including the analyzed subjects, including BMI cut-off or body mass index, comorbidity, age, etc.), poor repeatability of studies, dimensions of statistically non-significant recruited populations (major bias), shifts in the systems of emotional control of life-time impulses and another infinity of multiplicity of individual human variables that are difficult to reproduce. The pleiotropism of these behavioral behaviors with a highly negative impact on the quality of life is, therefore, a manifestation of a genetic penetrance that is today unpredictable.
Research that uses modern neuroimaging techniques to study nutrition and nutrition disorders comes up against the same issues. Even in this literature, therefore, the non-homogeneity, sometimes the contradictory, of results between one study and another is a paradoxical rule. Then, as in front of an impressionist painting, whose subject is more distinctly appreciated moving away a little from the work, so in brain imaging we can get a clearer idea without focusing on individual papers, but considering the bibliographic sources on magnetic resonance structural, functional, on the Diffusion Tensor (the DTI), the PET (Positron Emission Tomograhy) and the SPECT (Single Photon Emission Computed Tomography), taken together.
The evidences that emerge clearly are: an alteration of the striated-prefrontal neuronal circuits, anatomical substrate of the reward, driving, craving, and anomalous functioning of the insula, used to process inside the limbic circuit the gustatory and visceral information [27], a hypo-activation of bottom-up areas and systems (attention driven by external environmental stimulus, primarily through optical sensory pathways) and a hyper-activation of top-down ones (attention guided by cognitive processes internal, such as imaginative representations and memory) [28]. The latter are the neurobiological correlates of pathological control that patients with Anorexia Nervosa have on instincts, including hunger, and their lives in general.
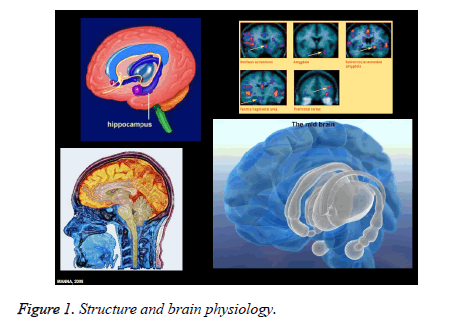
Thus, despite the lack of replicability of many results, the literature on the neuroimaging of nutrition disorders, however, manages to give us new insight into their pathogenesis - but, above all, new insight into what the disorders are: diseases that alter the structure and brain physiology. The hope is that these new scientific awareness and sensibilities will translate into innovative therapies, not only pharmacological, which are controversial today.
A study by Frank et al. - Department of Psychiatry of the University of Colorado and Eating Disorders Care, Colorado investigated the possible association between brain dopaminergic reward system, restriction of caloric intake and avoidance of food in a group of adolescents and young adults with anorexia nervosa. It was observed that the restriction of caloric intake and weight loss were associated with a sensitization of the dopaminergic reward system, reflected in an increase in the prediction error. In the opinion of the authors of the study, this increase found in dopominergic circuits could affect the mechanisms that fuel stress and anxiety by going to "overwhelm" the normal homeostatic hunger signals coming from the hypothalamus. In explaining this evidence, the authors report that weight loss, achieved through caloric restriction, would be associated with an abnormal activation of the reward system that would fuel anxiety, manifested through fear of weight gain and bodily dissatisfaction, which in turn would conflict with the homeostatic hunger signals, so the person eventually refrains from eating. In their model, there would be a vicious circle that would allow eating disorders to persist, maintain themselves over time through food restriction and malnutrition: in fact this direction of results was observed in the experimental group but not in the control group.
Finally, to the series of neuronal circuits and to the already known neuropeptides is added a new group of neurons located in a part so far little studied by the hypothalamus, the lateral nucleus of the tuber cinereum. It was discovered by a group from the Agency for Science Technology and Research (A* STAR) in Singapore. Previous research has shown that various areas of the brain are involved in eating behavior, for example the mid-basal hypothalamus, which assesses the relationship between food intake and energy expenditure, and the reward system, based on neurons that use dopamine as neurotransmitter, and several hormones are also involved, such as ghrelin, which stimulates the appetite and leptin, which tends to dampen it. Starting from the observation that brain damage in some regions of the hypothalamus due to various neurodegenerative diseases cause a drastic change in the eating habits of patients, who begin to eat very little spontaneously, Sarah Xinwei Luo and colleagues carried out experiments on mice to establish what specific characteristics the involved neurons had. The authors thus discovered that both after a period of fasting and after the administration of the hunger hormone ghrelin, a small group of neurons were activated in the hypothalamus which used GABA as the main mediator, but which also produce somatostatin. At this point the researchers activated and deactivated this particular group of neurons by exploiting both the administration of drugs and the use of optogenetics, a technique that involves the creation of genetically modified animals that a specific population of neurons expresses on its surface a photosensitive molecule. In this way it is possible to activate or deactivate those neurons with a pulse of light sent on a very thin optical fiber implanted in their brain. As a result the scientists obtained that the deactivation of these neurons reduced food intake and weight gain, while their stimulation had an opposite effect. Stimulation of somatostatin-producing neurons in other brain areas, such as the paraventricular nucleus, stria terminalis and amygdala, had no effect on the feeding behavior of animals.
Treatment and Therapies
The diagnostic-therapeutic-rehabilitative pathway of patients with eating disorders must always include both psychological and psychopathological aspects, both clinical-nutritional, metabolic and physical, and socio-environmental aspects, although to varying degrees depending on the specific eating disorder from which the patient is affected, of the different course, of the gravity and complexity of the clinical picture and of the various phases of the course. It must be based on the best available evidence, which at present is that detailed in the consensus document. The route must also guarantee:
• The active involvement of users and/or family members;
• Age-specific and disorderly management, both from a psychotherapeutic, psychiatric or neuropsychiatric point of view, both internally, pediatric and nutritional;
• The presence of personnel with specific training and experience in eating disorders;
• The treatment of any comorbidities and the general consequences of the disorder, in connection with staff trained on eating disorders.
The professional figures involved must be, depending on the age of the subject, the family doctor or the family pediatrician; psychiatrists or children's neuropsychiatrists; psychologists, psychotherapists, clinical nutritionists, internists or pediatricians, dieticians; other specialists (endocrinologist, gastroenterologist, gynecologist etc.), rehabilitators, nurses, educators, social workers, etc. can be variously represented at specific stages of the journey
The diagnostic evaluation of people with eating disorders should include:
• Examination of physical and nutritional health conditions;
• Examination of psychological, behavioral, family and social needs.
The diagnostic path also requires an accurate physical examination aimed at highlighting or excluding associated pathological conditions and/or complications, and a thorough evaluation of nutritional status. People with eating disorders should be evaluated and given treatment as soon as possible, before reaching worrisome physical conditions; close monitoring and treatment of severely underweight patients or those experiencing rapid weight loss should be a priority.
The psychotherapeutic intervention must be accompanied by a regular evaluation of the physical conditions that includes the measurement of body weight and specific parameters capable of signaling a possible increase in the risk to physical health. Nutritional rehabilitation is indicated at all treatment levels for weight recovery, food pattern restructuring, the achievement of a normal perception of hunger and satiety sensations and the correction of all the biological and psychological consequences of malnutrition. It is important that the re-feeding programs are applied in non-judgmental contexts and that they guarantee adequate emotional support for the patient.
Psychopharmacological treatment can certainly be useful in the appropriate treatment of psychiatric comorbid conditions, although some drugs must be used with caution, in consideration of the physical vulnerability of many patients. The clinical impression suggests that they may be useful in patients who have resistance to weight recovery, obsessive thinking or denial of the disease. Drugs should not be used as an exclusive treatment for eating disorders.
Cognitive behavioral therapy has been shown to be very suitable for eating disorders. It involves the use of diaries that allow you to monitor food intake, compensatory behaviors, work on emotions and thoughts related to food, physical appearance, weight. Patients learn to eat properly and to discuss dysfunctional thoughts that produce unpleasant emotions and that perpetuate uncontrolled food intake behaviors, fasting, vomiting, exaggeration in exercise, etc. The treatment of some cases of bulimia nervosa may require a therapy of 4-6 months, while for cases of anorexia nervosa it may take 1-2 years. For those who have a mild ailment, resorting to a dietician may be sufficient.
For some years the scientific literature has highlighted what are the neuroanatomical substrates related to eating disorders:
• Reduction in the volume of gray matter in regions involved in reward, impulse control and emotion regulation [29];
• Anomalies in the networks involving the anterior cingulate cortex (ACC) and the insula [30];
• Abnormal activation in response to aversive or reward stimuli [31].
The study by Dunlop and his collaborators focused in particular on an area of the brain that is called dorsomedial prefrontal cortex (dmPFC) [32]. This area plays a very important role in the aspects of self-control, inhibition of movements, suppression of emotional response, control of impulses, "loss-chasing" also present in pathological gambling. Researchers demonstrated how a non-invasive intervention using transcranial magnetic stimulation (rTMS) on this area improved the top-down control action on striatal regions associated with food control dysregulation behaviors (binge eating/purgation). The final result was a significant improvement in the connections within the neural network taken into consideration and a decrease in the dysfunctional behaviors examined.
Other studies are currently underway to demonstrate the effectiveness of such interventions. Prevention interventions are divided into primary (before the onset of the disease), secondary (at the first signs of symptoms) and tertiary (a confirmed disorder and therefore coincide with the actual treatment).
Anorexia and bulimia, disorders characterized by extreme eating habits and distorted body image, are among the most lethal psychiatric disorders, with few available treatments considered effective. An important study suggests that impaired functioning of some neural circuits could contribute to food restriction in anorexia and overeating in bulimia. The research, published June 4 in the online edition of the (American Journal of Psychiatry, and conducted by Tyson Oberndorfer and Walter H. Kaye), could pave the way to new and more effective treatments of these pathological conditions [33].
"We still don't know if anorexic or bulimic individuals suffer from a brain system disorder that regulates appetite, or if their eating behaviors are motivated by other phenomena, such as an obsessive concern about body image," says Kaye. "However, this study confirms other previous ones carried out by ours and other teams, establishing a clear relationship between these disorders and the way in which the insula, the area of the brain linked to the sense of taste, processes the reward signals to give to the individual the sense of hunger or satiety.”
The study used functional magnetic resonance imaging to test these brain areas, measuring the sweet taste response in 28 women who managed to overcome anorexia or bulimia. Compared to a group of 14 women who had never suffered from these disorders, women recovered from anorexia had a brain response significantly attenuated to the taste of sucrose (common sugar), while those cured of bulimia had significantly elevated it.
"One possibility is that the restricted intake of food occurs in anorexia because the brain cannot accurately recognize the sense of hunger," says Oberndorfer. "In contrast, overeating would occur in bulimia because of an exaggerated sense of hunger." A recent complementary study has investigated the brain structure in anorexia and bulimia nervosa and also found that the insula could be the basis for these eating disorders [34].
The researchers add that such studies could prove important for the treatment of these conditions. Identifying an abnormal neural substrate could help in reformulating the disease and offer new target areas for new treatments. "It may be possible to remodel the subjective experience, for example, by increasing the activity of the insula in anorexic individuals and attenuating it in bulimics," says Kaye.
Other studies indicate that healthy subjects can use feedback from magnetic resonance or biofeedback and mindfulness (a form of meditative psychotherapy, N.d.T.) to alter the brain's response to food stimuli. In anorexic patients with signs of satiety that are too strong in response to appetizing foods, the researchers suggest that light or even slightly repugnant foods could prevent cerebral over-stimulation. Medications capable of increasing or decreasing the reward response to food could also be developed.
The most suitable treatment for the person should be chosen together with a trusted therapist after a thorough diagnostic evaluation. The factors to be taken into consideration are many: the type of disorder, the physical situation, the presence of complications, the duration of the illness, the age, the expectations of the person and the previous therapeutic experiences, the availability of therapists and appropriate facilities nearby to the residence, personality characteristics and others. Treatment techniques are:
• Nutritional rehabilitation;
• Individual and group cognitive-behavioral therapy;
• Interpersonal therapy;
• Psychoanalytic psychotherapies;
• Food psychoeducation;
• Drug therapies;
• Family therapies;
• Cognitive rehabilitation therapy;
• Self-help.
For Bruch, traditional psychoanalysis, with its emphasis on the interpretation of unconscious processes, is rather ineffective. Employing a less orthodox psychoanalytic approach, which included an active participation by the patient in the reconstruction of her past, much better results were obtained. Because patients felt they were being listened to for the first time in their lives, instead of having to undergo an interpretation of their feelings and intentions. A peculiarity of the parents of anorexics seems, in fact, to be the imposition of decisions and convictions, with little attention to the expressions of need and desire of the child: it would be this lack of confirmation in the first mother-daughter interactions to lead to typical deficiencies in the of the Self, of identity and autonomy, as well as a lack of awareness of one's body. In the therapy of mental anorexia it was recognized, therefore, that the interpretation of the content is less important than the reconstruction of the interactional models of development and the correction of the wrong ideas of childhood.
Conclusion
It is now known that, in the context of the pathogenesis and maintenance of eating disorders, multifactoriality plays a central role. The problems related to this type of disorder, which arise between the psyche and the soma, are manifold, so much so that the data up to now present in the lit