Research Article - Journal of Clinical Dentistry and Oral Health (2017) Oral Medicine and Surgery
Musculoskeletal disorders among lebanese dentists-trend evolution.
Abi Aad Lamia*
Department of Dental Public Health, Lebanese University, Hadath, Lebanon
Accepted on December 05, 2016
Citation: Abi Aad L. Musculoskeletal Disorders among Lebanese Dentists-Trend Evolution. J Oral Med Toxicol. 2016; 1(1); 1-5
Abstract
Background: Musculoskeletal Disorders (MSDs) are significant workplace problems affecting dental professionals. This disease is on the rise among dental workers. Despite improvements in knowledge and ergonomic strategies in dental workplace, many dentists still don’t believe that their work environments affect their physical health. Moreover, many dentists don’t follow ergonomic guidelines in their practices.
Aim: To assess the prevalence and the relationships between demographic variables and some dental practices with musculoskeletal disorders among Lebanese dentists.
Materials and methods: Self-administrated questionnaires were answered by a sample of 218 dentists. I collected information about demographic variables such as gender, age, and years of experience, practices, and specialization. I also collected information about other variables such as: location of pain in different parts of the body. The recorded data was analysed with SPSS 20. P-value <0.05 was considered to be statistically significant.
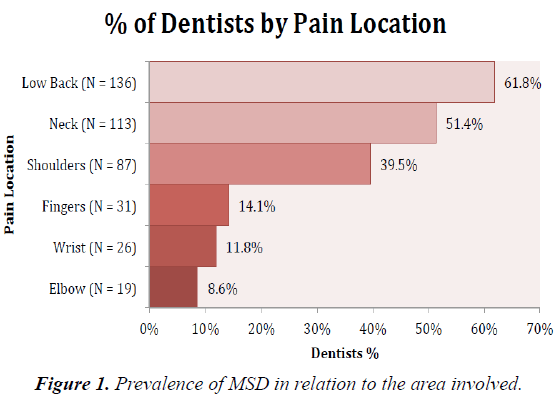
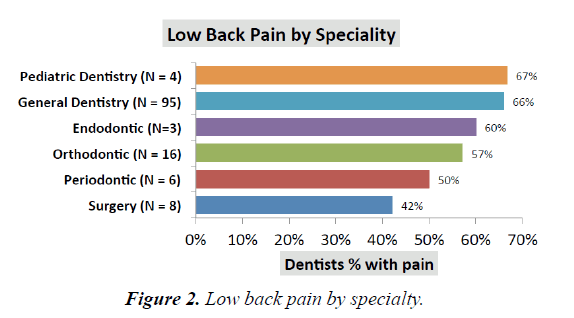
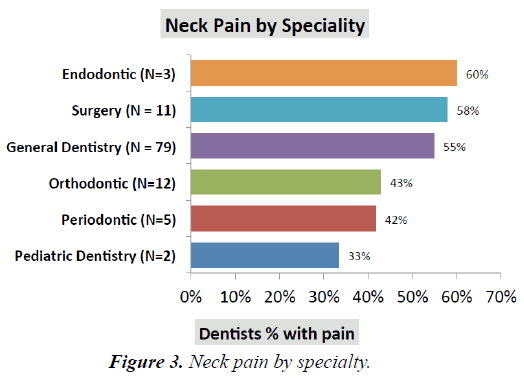
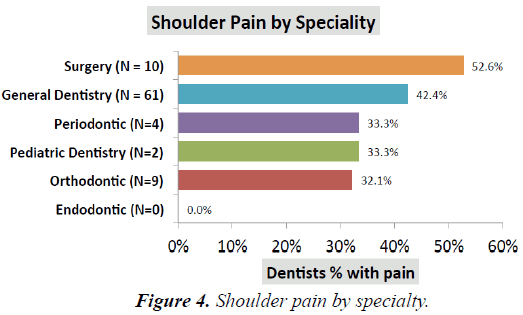
Results: 92.7% of the participants suffered from musculoskeletal disorders; out of which 40% had at least one MSD symptom over the past twelve months. Most common areas affected by MSD in order of magnitude were low back pain (61.8%), neck pain (51.5%), shoulders pain (39.5%), fingers pain (14.1%), wrists pain (11.8%), and elbows pain (8.6%). Pain differences were statistically significant among specialists. Back pain was the highest among paediatric dentists. Neck pain was the highest among endodontic dentists. While shoulders pain was the highest among dental surgeons. Neck pain was related to the working hours per day. Pain location was statistically significant between genders. In particular, females suffered more than males especially at the neck and the wrist levels. Permanent pain by location is inversely proportional to physical activity.
Conclusion: These findings may confirm that Lebanese dentists do not respect the ergonomic recommendations, and that Lebanese dentists have low awareness about their health issues. Further studies are needed to identify the specific risk factors for MSD for Lebanese dentists in order to introduce effective remedial measures.
Keywords
Dentistry, Health, Musculoskeletal disease, Ergonomics.
Introduction
Dentists are often exposed to a variety of occupational hazards that include but are not limited to chemical, biological, legal, as well as ergonomic hazards. These hazards can lead to diseases, disorders, and stresses [1]. In United Kingdom, a study had shown that the most frequent causes of premature retirement among dentists were: Musculoskeletal disorders 29.5%, cardiovascular diseases 21.1%, and neurotic symptoms 16.5% [2]. Musculoskeletal disorders and stress related illnesses were the two most important factors that influenced premature retirement [2].
Literature reviews across the world confirm that there is a high prevalence of Musculoskeletal Disorders (MSDs) among dentists [3-5]. The estimation is that 63-93% of dentists experienced musculoskeletal disorders worldwide [5]. World Health Organization (WHO) and United Nations [3] recognized that MSDs are the causes of long-term pains and disabilities that affect hundreds of millions of people [6]. World Health Organization defines an MSD as “A disorder of the muscles, tendons, peripheral nerves or vascular system not directly resulting from an acute or instantaneous event (e.g., slips or falls)” [7].
Problems causing MSDs symptoms are numerous. Risk factors are habits, genetic predisposition, physical conditioning, and age [1,6,8]. Dentists spend their workdays in static and awkward positions with repetitive movements, frequent vibrations affecting their hands and wrists, and suboptimal lightings [1-6]. They perform precise procedures in a small workspace: “The Patient Mouth”. Common postures of dentists are static these static postures require contractions of muscles to hold the body motionless while resisting gravity [9-10]. The awkward positions are due to improper seating, improper patient positioning, poor technics, and poorly designed equipment. Repetitive motions are extremely prevalent in clinical practices that involve performing scaling, root planning, and polishing [9]. Excessive Force is also prevalent in dentistry while extracting teeth. Grasping small instruments for prolonged periods requires a much greater force application than a power grip (object in the palm of the hand) [3].
However, there is reason to believe that MSD represent a significant barrier for the dental profession. A systemic review of high prevalence of MSDs in the dental profession identified a clear trend towards increasing awareness about MSDs in developed countries when compared to less developed countries [3,4,11]. What about Lebanon? In light of the above, the aim of this study is to assess the prevalence of MSDs among Lebanese’s dentists.
Materials and Methods
This survey was conducted in 2013 during two main dental conventions: The biannual meeting of the International Convention of the Lebanese University in September, and Beirut International Dental Meeting of the Lebanese Dental Association in October.
Based on a review of literature, a self-administered questionnaire was developed and adopted after being tested on 10 dentists. The self-administered questionnaire used to collect data was composed of 11 questions:
• Demographic variables: age, gender, years of experience, and specialty.
• Working technics: posture (standing or sitting or alternate between standing and sitting), duration of work (working hours per day, working day per week), and vision (if direct or indirect vision).
• Practice of dentistry: General dentistry or specialty.
• Pain location over the twelve past months: neck, shoulder, lower back, fingers, wrists, and elbows.
• Frequency of pain (rare, permanent, occasional, or none).
• Physical or none physical activity.
More than 300 questionnaires were hand-distributed to the participants during the day. The approached dentists were given a choice to fill either an English or French survey. Moreover, the dentists were asked to return it after answering individually in order to avoid collective answers and peer influence. The questionnaires were anonymous to maintain confidentiality.
230 questionnaires were filled and returned in the same day. Twelve questionnaires were not completely filled, and therefore were excluded from the study. Only 218 questionnaires were included in the study.
Statistical analysis: Data entry was performed using the software Access (Microsoft Office). Statistical package for social sciences (SPSS) version 20 was used to determine frequency distributions, means and proportions. Comparison of proportions was done using Fischer’s exact test. P-value <0.05 was considered as statistically significant.
Results
Demographic characteristics of the study sample
The sample included 218 dentists of which 67.4% are males and 32.6% are females. The mean age of the participants was 43. General dentists accounted to 67% of the studied subjects, and the remaining were specialists: Paediatric dentistry, oral surgeon, endodontic, periodontologist, and orthodontic. The average duration of practice was 18.6 years. Most of the practitioners were working 7 h per day and 5 days per week. 64% of dentists were working in the sitting position, and 52% of the dentists were using both direct and indirect vision (Table 1).
| N | % | |
|---|---|---|
| Gender | ||
| Male | 147 | 67.40% |
| Female | 71 | 32.60% |
| Total | 218 | 100.00% |
| Specialty | ||
| General Dentistry | 144 | 67.30% |
| Oral Surgery | 19 | 8.90% |
| Endodontic | 5 | 2.30% |
| Orthodontic | 28 | 13.10% |
| Paediatric Dentistry | 6 | 2.80% |
| Periodontology | 12 | 5.60% |
| Total | 214 | 100.00% |
| Vision | ||
| Direct | 86 | 39.40% |
| Indirect | 18 | 8.30% |
| Both | 114 | 52.30% |
| Total | 218 | 100.00% |
| Posture | ||
| Sitting | 138 | 64.50% |
| Standing | 11 | 5.10% |
| Both | 65 | 30.40% |
| Total | 214 | 100.00% |
| Age: Mean (SD); Min-Max | 43.1(10.7); 22-70 | |
| Years of experience: Mean (SD); Min-Max | 18.7 (9.8); 1-45 | |
| Daily working hours: Mean (SD); Min-Max | 7.4 (1.98); 2-12 | |
| Weekly working days: Mean (SD); Min-Max | 5.2 (0.82); 2-6 | |
Table 1: Distribution of dentists by demographic characteristics in relation to the prevalence of MSD.
Prevalence of MSD
92.7% of the participants suffered from musculoskeletal disorders. Overall, 40% of the practitioners had a prevalence of at least one MSD symptom over the twelve past months. 60% of the participants had pain in more than one side. The most common areas affected with MSD in order of magnitude were: low back (61.8%), neck (51.4%), shoulders (39.5%), fingers (14.1%), wrists (11.8%), and elbows (8.6%) (Figure 1).
Variables analysis
Pain was statistically significant by specialty. Back pain was the highest among paediatric dentists (67%) and general dentists (66%), and the lowest for oral surgeons (47%) (Figure 2).
Area wise predilection of MSD in relation to specialty of the dental practitioners.
MSD in the low back area was the highest among paediatric dentists and general dentists, and the lowest among oral surgeons.
Neck pain was the highest among endodontic dentists (60%) and the lowest among paediatric dentists (33%) (Figure 3).
MSD in the neck area was the highest among endodontics and surgeons, and the lowest among paediatric dentists.
Shoulder pain was the highest among oral surgeons (52.6%). In reverse endodontic dentists hadn’t complained from shoulders’ pain (Figure 4).
MSD in the shoulder area was the highest among surgeons, and they’re no pain among endodontics.
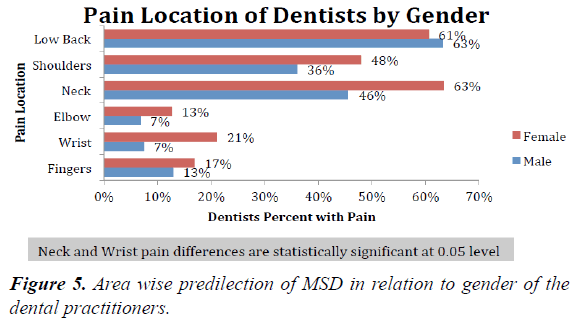
The comparison between male and female showed that females had more pain in almost anatomical areas (neck, shoulders, elbows, wrists and fingers). Differences in the neck pain and wrists pain were statistically significant at level 0.05.
Working hours per day seems to have relation with neck pain.
63% of female suffered from neck pain compared to 46% of males. 21% of female dentists suffered from wrists pain compared to 7% of male dentists (Figure 5).
Prevalence of MSD in the involved area was higher for female dentists than for male dentists. Female dentists suffer much more than male dentists in both neck and wrists areas.
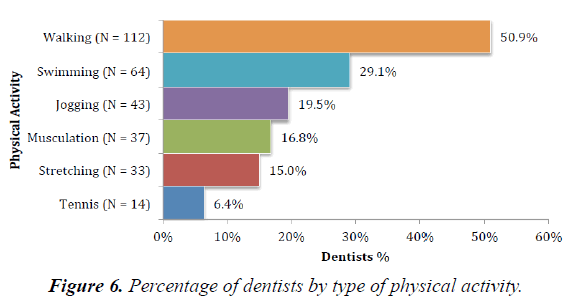
It seemed that the most physical activity practiced by Lebanese dentist was walking 50.9% (Figure 6).
50.9% of dentists choose walking as physical activity while 29% of dentists choose swimming.
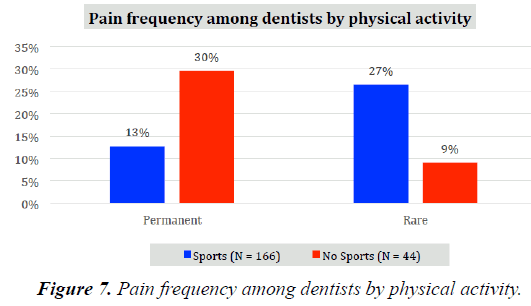
The relationship between pain and physical activity was inversely proportional. The frequency of pain decreased with physical activities. In particular, pain became rare instead of permanent (Figure 7).
The frequency of pain is decreasing with physical activities. The relation between pain and physical activities is inversely proportional.
There are no relationships between MSDs symptoms and neither age, nor years of practice.
Discussion
The importance of maintaining healthy life is irrefutable. As the prevalence of MSD across the world is high [12,13], dentists need to understand the factors that contribute to this disease so they can make better choices regarding ergonomic equipment’s, physical exercises, and healthy lifestyle. The comparison between the two latest studies conducted in Lebanon in 2001 and 2013 shows that the number of dentists suffering from MSDs is increasing. In fact, 66% of Lebanese dentists suffered from MSDs in 2001 [14], whereas 92.7% of Lebanese dentists suffered from MSDs in 2013. While only 7.3% of Lebanese dentists hadn’t complained from MSDs, 40% of Lebanese dentists had at least one MSD symptom over the twelve past months, and 60% of Lebanese dentists suffered from pain in more than one side. These results suggest that dentists’ awareness in preventing and managing work-related musculoskeletal problems in their practice is sufficient. The increasing prevalence of MSDs between 2001 and 2013 is probably due to: 1: The frequency and duration of awkward body positioning, 2: Movements made by dentists in their daily work, and 3: The lack of recovery time and physical activity. In fact, taking breaks between cases are extremely recommended [15]. Moreover, using micro pauses and stretching during dental procedure are very efficient [4,16,17]. Many studies pointed out to the efficacy of these preventive remedies. In particular, stretching increases the blood flow to muscle, the production of joint synovial fluid, the nutrient supply to vertebral disks, and reduces formation of trigger points [18]. The results of both surveys in Lebanon confirm that MSDs symptoms are decreasing with physical activity (P=0.07), and with frequency and period of breaks during the work day (P=0.05) [14].
There are many studies concerning MSD among dentists. A targeted look at the upper and lower body, neck, shoulders, and wrists are common in all studies. These studies have shown a high prevalence in musculoskeletal disorders. Studies in Lebanon as well in New Zealand and in Saudi Arabia [19] have shown that most common areas affected by MSD in order of magnitude were Low back pain, followed by neck pain, followed by shoulders pain.
Based on the final results, low back pain was the highest for paediatric dentists and general dentists, and the lowest for dental surgeons. It seems that paediatrics dentists in Lebanon are bending or twisting their upper bodies to reach the small working spaces (mouths of the young patients). During bending and twisting motions of the spine, the pressure on the lumbar discs is increased by 200%. This can cause compression on a spinal nerve (Fish, 1987). Repeated twisting in one direction may result in muscle imbalances leading to low back pain [20].
While the prevalence of back pain was 61.8% among Lebanese dentists, review of articles shows us that the prevalence of back pain was: 64% in Australia, 53% in Queens Land Australia, 50% Denmark, and 32.3% in Teheran [20]. However musculoskeletal pain in the lower back remains a constant cause of loss of work for dentists [21].
Neck pain prevalence was: 51.4% in Lebanon, Queensland Australia (57%) [22,23], in Dutch (51%) [24], Iran (47%) [20], Saudi Arabia (39.3%) [19] and New Zealand (57%) [18]. Similar to my results, in China daily working hours were significantly associated with the presence of neck pain [4]. Based on the final results, neck pain was the highest for endodontic dentists and oral surgeons, and the lowest for paediatrics dentists. Endodontic as well as surgeon spend their workday in awkward head positions to perform precise procedures. Besides, they have a high level of stress while performing treatments, which increases the potential risk of injuries. Use of loupes or surgical telescope is very helpful while doing endodontic treatments. In particular, dentists could maintain their bodies so the body could be maintained in a neutral working posture. Head over the shoulder, head and back are aligned [4,25].
Shoulders pain in this study was 39.5%, it was the highest among surgeons, approximately similar results are found in USA [3]. In New Zealand, the prevalence of shoulders pain was 52% [18]. It seems that dentists in China have complained more from shoulders pain 83.3% than in others part of the body [26]. While extracting a tooth, surgeons raise the upper arms. This causes a significant impairment in blood circulation within the shoulders and neck regions.
Gender pain differences were found also in Lithuania, New Zealand, India [3] and Saudi Arabia [19]. Females had more pain than males. In my study, neck and wrist pains were statistically significant. In Saudi Arabia, shoulder’s pain was double for the females [19].
As a result, dentists should manage their health by adopting ergonomic guidelines in their work places. They should attempt to use a wide range of positions around the patients heads, often referred to as “o’clock positions”. The head and the back should be aligned. The upper arm should be parallel to the floor. Weight should be balanced. Hip angle should be more than 90 degrees. Practitioners should have their seat positioned low enough so that they are able to rest the heels of their feet on the floor [25]. Dentists should position instruments within easy reach and avoid twisting or reaching across the body [25]. The use of loupes, surgical telescopes allow dentists to maintain a neutral working posture while increasing their visual acuity, level of motor control, and diagnostic ability (UBC, 2008) [4].
Dentists should vary their work positions to shift the workload from one group of muscles to another [13,16]. Dentists should alternate between standing and sitting. In fact, alternating between standing and sitting lets one group of muscles rest, while the workload is shifted to another group of muscles [26]. Repositioning the feet can also shift the workload from one group of low back muscles to another [26]. Patients should be placed in a semi supine position for mandibular and maxillary procedures [16].
The developments of fourhanded operatory techniques contribute to working more efficiently and increase productivity [15]. Fourhanded seats were suggested, and equipment’s were developed mainly because of complaints of musculoskeletal disorders in dentists. The results emphasize the importance of continuing education in the form of training courses, and conferences.
Conclusion
This study illustrates clear work-related MSDs, as Musculoskeletal Disorders represent a significant barrier for dentists. Promoting prevention programs regarding ergonomic postures is a necessity to dentists during their clinical practices. Dentists must educate themselves and their staff members by adopting healthy habits that include: positioning strategies, selecting ergonomic equipment, incorporating frequent work breaks, doing physical activities, and looking for stress relief.
References
- Rabiei M, Shakiba M, Dehgan-Shahreza H, et al. Muscoloskeletal Disorders in Dentists. Int J Occup Hyg. 2012; 4(1): 36-40.
- Burke FJ, Main JR, Freeman R. The practice of dentistry: an assessment of reasons for premature retirement. Br Dent J. 1997; 182: 250-4.
- Muralidharan D, Fareed N, Shanthi M. Musculoskeletal Disorders among Dental Practitioners: Does It Affect Practice?. Epidemiol Res Int. 2013.
- Feng B, Liang Q, Wang Y, et al. Prevalence of Work-related Musculoskeletal symptoms of the neck and upper extremity among dentists in china. BMJ open. 2014; 4.
- Saraji JN, Hosseini MH, Shahtaheri SJ, et al. Evaluation of ergonomic postures of dental profession by Rapid Entire Body Assessment (REBA), in Birjand, Iran. J Dent Med. 2005; 18 (1): 61-7.
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Org 2003; 81(9): 646-56.
- Identification and control of work related diseases. Report of a WHO expert committee; 1985. World Health OrganizationTechnical Report Series 714.
- Aloraibi SFA. Musculoskeletal disorders among dentists in Nepal. J Canadian Dent Assoc. 2011; 11(2):107-13.
- Chopra A. Musculoskeletal Disorders in Dentistry- A review. JSM Dent. 2014; 2(3): 1-4.
- Ergonomics and Dental Work. Occupational Health Clinics for Ontario Workers Inc. Available from: http://www.ohcow.on.ca/edit/files/workbooks/ERGONOMICS%20AND%20DENTAL%20WORK.pdf
- Thornton LJ, Barr AE, Stuart-Buttle C, et al. Perceived musculoskeletal symptoms among dental students in the clinic work environment. Ergonomics. 2008; 5(4): 573-86.
- Lehto TU, Helenius HY, Alaranta HT. Musculoskeletal symptoms of dentists assessed by a multidisciplinary approach. Community Dent Oral Epidemiol.1991; 19(1): 38-44.
- Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010; 35(4): 419-29.
- Ghoussoub MS, Ghoussoub K, Moucharrafieh L, et al. Trouble Musculo-Squelettique Chez Une Population De Chirurgiens-Dentistes Libanais : Fréquence Et Facteurs De Risque. Leb Med J. 2005; 53(1): 21-7.
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: Strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003; 134(12): 1604-12.
- Mclean L, Tinglay M, Scott RN, et al. Computer terminal work and the benefit of microbreaks. Appl Ergon. 2001; 32(3): 225-37.
- Shaik AR, Rao SB, Husain A, etal. Work-related musculoskeletal disorders among dental surgeon: A pilot study. 2011; 2(4): 308-12.
- Samotoi A, Moffat SM, Thomson. WM Musculoskeletal symptoms in New Zealand dental therapists: prevalence and associated disability. N Z Dent J. 2008; 104(2): 49-53.
- Al-MohrejOA, AlShaalan NS, Al-Bani WM, et al. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open.2016; 6.
- Lalumandier J, McPhee SD, Parrott CB, et al. Musculoskeletal pain: Prevalence, prevention, and differences among dental office personnel. Gen Dent. 2001; 49(2): 160-6.
- Bhandari SB, Bhandari R, Uppal RS, et al. Musculoskeletal Disorders in clinical dentistry and their Prevention. J Orofac Res. 2013; 3(2): 106-14.
- Sakzewski L, Naser-Ud-Din S. Work-related musculoskeletal disorders in Australian dentists and orthodontists: Risk assessment and prevention. Work. 2015; 52(3):559-79.
- Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J. 2006; 51(4): 324-7.
- Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work. 2005; 25(3): 211-20.
- Ergonomics and office organization in endodontics. Endodontics. Available from: http://www.information-dentaire.fr/011025-22783-Ergonomie-et-organisation-du-cabinet-en-endodontie.html
- Fish DR, Morris-Allan DM. Musculoskeletal Disorders in dentists. NYS Dent J. 1998; 64(4): 44-8.