Research Article - Journal of Pain Management and Therapy (2017) Volume 1, Issue 1
Manual Therapies Reduce Pain Associated with Trigeminal Neuralgia.
Susan Vaughan Kratz*Special Therapies, Inc. 1720 Dolphin Drive, Unit B Waukesha, Wisconsin 53186, USA
- *Corresponding Author:
- Susan Vaughan Kratz
Special Therapies, Inc.
1720 Dolphin Drive, Unit B Waukesha, Wisconsin 53186
USA
Tel: 262-347-2222
E-mail: info@specialtherapies.com
Accepted date: November 24, 2016
Abstract
Introduction: Trigeminal Neuralgia (TN) can be an extremely debilitating condition effecting quality of life, emotional well-being, and engagement in daily occupation. Surgical and medication treatments are cited extensively through the literature but can have undesired side effects, can lose effectiveness over time, or are quite invasive. Little is reported about craniosacral therapy, lymphatic drainage, or other gentle manual techniques as treatment options. Objective: This paper introduces and summarizes the experiential process and outcomes of three adults receiving manual therapies to treat TN. This review investigates low-risk, conservation clinical options and explores for treatment guidelines for TN. Method: Chart review and client interviews in multiple follow-up contacts of a convenience sample to explore immediate and long term outcomes. All treatment techniques utilized per clients are summarized, and include: Upledger’s CranioSacral Therapy (U-CST); Chikly’s brain curriculum for lymphatic enhancement and nerve down-regulation techniques; and Wanveer’s glia structure and glymphatic mobilization techniques. One occurrence of a spontaneous Somato-Emotional Release technique was also called for. Measurement of baseline and outcomes was conducted using: Verbal descriptor scale; Verbal numeric rating scale; Visual analog scale (VAS); and Self-report of quality of life and pain’s impact upon performing daily activities. Data were analyzed using qualitative content analysis Conclusion: Three adults reported individual positive changes or resolution of TN pain. All three reported restoration of quality of life and emotional well-being. One made use of techniques for self-help Comparison to other methods, or variations of these methods utilizing the same names or terminologies, should be avoided. This report is an attempt to aid in the needed clarification between different approaches used in clinical practices. Positive responses suggest that these methods hold value for further study as a viable treatment option to address the agony of neuralgia.
Keywords
Trigeminal neuralgia, Craniosacral therapy, Lymphatic drainage, Glia and glymphatic mobilization method, soft tissue and fluid mobilization
Introduction
Trigeminal neuralgia (TN) is a common pain syndrome. The classic form (Type 1) is characterized by sudden onset of extreme, sporadic, burning or shock-like facial pain that is temporary or episodic [1]. The atypical form (Type 2), is characterized by constant aching, burning, stabbing pain of somewhat lower intensity than Type 1. The intensity of pain can be physically and mentally incapacitating [1-3]. Secondary Symptomatic Trigeminal Neuralgia results from demyelinating conditions such as multiple sclerosis [1,4]. Post- Herpetic Neuralgia results from herpes zoster or other viral outbreak [5,6]. Further differentiation of such neuropathic pain can be a result from injury from facial trauma, oral or other surgery, cerebral vascular accident, or infection. This pain is described as dull, burning, or boring and is usually constant. Hypersensitivity, numbness and tingling are also signs of a damaged nerve [7,8].
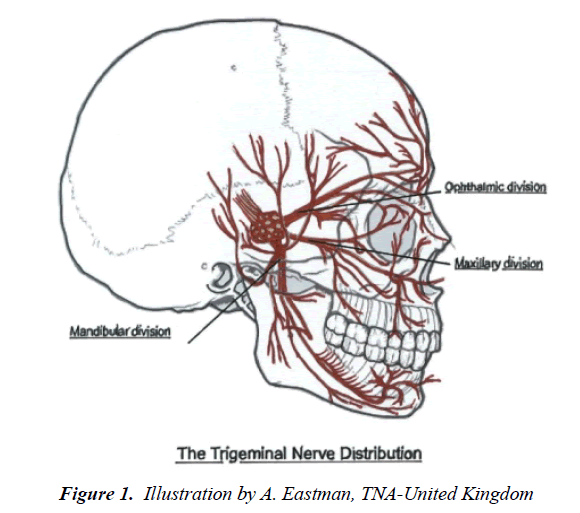
A common structural problem associated with TN is a compression between a blood vessel and the trigeminal nerve base [8]. A less common cause may be from a tumor compressing the trigeminal nerve [8]. One definitive etiology of interest to the manual therapy practitioner is the conviction that facial trauma can produce a sphenopetrous distortion, with resulting restrictions of the dural membrane of the cranial nerve. The strain may be over the petrous ridge or within Meckel's cave, as well as the various foramina [9]. As a result circulatory stasis and faulty cerebrospinal fluid metabolic function contribute to the irritability. Differential diagnosis of TN is based solely on clinical findings and careful evaluation of the patient history and a thorough medical examination are essential [1,10]. Though most often occurring in women over age 50, TN can manifest at any age, including infancy [8]. The trigeminal nerve has three branches that conduct sensations from the upper, middle, and lower portions of the face, as well as the oral cavity [8,11] (Figure 1).
Emerging theories about idiopathic and neurogenic pain
The trigeminal ganglion is comprised of neuron and distinct types of glia: Schwann and satellite glial cells [12]. Traditional belief held that peripheral tissue insult led to excitation of trigeminal nerves thus releasing inflammatory molecules back into the periphery. However, recent findings have demonstrated that increased interactions between neuronal cell bodies and satellite glial cells within the trigeminal ganglion are at play [13]. Increased signaling between neuronal cell bodies and satellite glia cells in trigeminal ganglia may lead to the development of persistent pain. These cell-to-cell interactions, which involve the transfer of key regulatory mediators via channels or gap junctions as well as paracrine signaling, are thought to play an important role in the induction and maintenance of peripheral sensitization of trigeminal nociceptors [13-15].
While there is much evidence to support the role of increased neuron-glia interactions contributing to hyperalgesia and chronic pain, the significance of neuron-satellite glial cell interactions within trigeminal ganglia is only now being elucidated. It has been suggested that neuronal–glial cell communication via gap junctions and paracrine signaling may also be involved in the development of peripheral sensitization within the trigeminal ganglion, and therefore play an important role in the underlying pathology of diseases involving trigeminal nerve activation [13]. Furthermore there is now compelling evidence implicating astrocytes, microglia, and other glial cells are pivotal regulators of multiple aspects of CNS inflammatory responses and pain hypersensitivity after nerve insult [16,17].
Lymphatic and glymphatic systems
Numerous articles have been published describing the scientific discovery of the lymphatic system of the peripheral body, but few of these articles have focused on the origin and development of manual techniques addressing this complex system of vessels, valves, nodes, and organs [18]. Chikly is one of the world’s foremost experts in the field of lymphatic function and teaches specific manual lymphatic drainage (LD) techniques that are in-sync with the precise anatomy of the lymph vessels and nodes [19]. Little to no clinical outcome research is available for LD directly treating the central nervous system, though its use is extensive in treating lymphedema and reduction of edema [20,21]. Upledger proposed through gentle, sustained stretch and mobilization of the cranial membranes [the Upledger CranioSacral Therapy 10-Step Protocol], facilitated to enhance of flow and exchange of cerebral fluids, though this method did not address intracranial drainage pathways [22].
The brain lacks a lymphatic circulation and must clear extracellular proteins by an alternative mechanism. Though it is not clear how solutes from the brain interstitium move between the parenchyma to the cerebral spinal fluid, one recent study showed that cerebral spinal fluid (CSF) enters the parenchyma along perivascular spaces that surround penetrating arteries and that brain interstitial fluid is cleared along paravenous drainage pathways [23]. In addition, the paravascular space may serve as a lymphatic equivalent that represents a separate highway for the transport of lipids and signaling molecules [24]. It can be argued based on this science that lack of movement of noxious fluids in the synaptic spaces may contribute to the inflammatory environment leading to idiopathic nerve pain. Thus, the therapeutic facilitation of movement of fluids around and through the central nervous system offers a theoretical treatment approach [19,21,22,25-28].
A surprising finding of a lymphatic vessel network in the dura mater of the mouse brain demonstrated that dural lymphatic vessels absorb CSF from the adjacent subarachnoid space and brain interstitial fluid via the glymphatic system [29]. The glymphatic system is a recently discovered macroscopic waste clearance system that utilizes a unique system of perivascular tunnels, formed by astroglial cells, to promote efficient elimination of soluble proteins and metabolites from the central nervous system [30]. In the periphery, the lymphatic circulation facilitates the clearance of extracellular proteins and excess fluid from the interstitium, a role critical to tissue homeostasis and function. Yet it was long believed that the brain lacks a lymphatic circulation and must clear extracellular proteins by an alternative mechanism [31]. Though it is not clear how solutes from the brain interstitium move between the parenchyma to the cerebral spinal fluid, one recent study showed that CSF enters the parenchyma along paravascular spaces that surround penetrating arteries and that brain interstitial fluid is cleared along paravenous drainage pathways [23]. The glymphatic system is a recently discovered macroscopic waste clearance system that utilizes a unique system of perivascular tunnels, formed by astroglial cells, to promote efficient elimination of soluble proteins and metabolites from the central nervous system [32].
Treatment Options for TN
A large variety of treatment options for TN are available, ranging from allopathic medicine, surgical, osteopathic, and ancient methods such as acupuncture [8,33-38] Standards of care for many procedures have been thoroughly cited. However, empirical data and standards of care of other low risk and noninvasive, complimentary treatments for TD are lacking. Osteopathic manipulation treatment guidelines for TN have been suggested in the past [9]. CranioSacral Therapy (CST) techniques were created to directly treat the fascial and fluids of the central nervous system to address a multitude of diagnostics [22,25]. Parallel fluid models of the physiology of the central nervous system as well as studies on the effects of gentle sustained stretch on tissues provide theoretical foundation to justify such manual techniques as CST [27,39-41]. Chikly’s Lymphatic Drainage methods also have explored methods to therapeutically influence fluids of the central nervous system [19,21]. Nerve down-regulation release technique follows tension patterns along any nerve distribution towards its nucleus [42].
Many therapists who practice manual interventions commonly combine the various methods listed here. There have been several attempts at scientific inquiry into the mechanisms of the craniosacral system of the body and the effects of CST upon function, but still it remains hypothetical and incomplete due to the complexity of the subject [43]. A systematic review to evaluate the clinical benefits of CST provides available evidence of the clinical benefits of CST, citing that progress has been seen over the last decade in the methodological quality of studies, scarce as it is [44]. A few stronger studies demonstrated that CST showed positive effects in the realm of pain remediation. In a randomized controlled study comparing CST to a sham control, patients with chronic neck pain reported statistically relevant effects [45-47]. CST improved medium-term pain related symptoms in patients with fibromyalgia [48] and alleviate migraine symptoms [49]. Perception in some patients suffering from trigeminal neuralgia following cranio-cervical decompression could be triggered by scar tissue and was reportedly reduced by manual treatment [50]. Increasingly CST is being sought as a preferential treatment as evidenced in a National Institute of Health’s decade-long review of the U.S. trends in the personal use of complementary health approaches [51]. Other than for lymphedema studies, there have been little clinical outcome studies of the effects of lymphatic drainage therapies upon pain or nerve function.
Assessment Measures
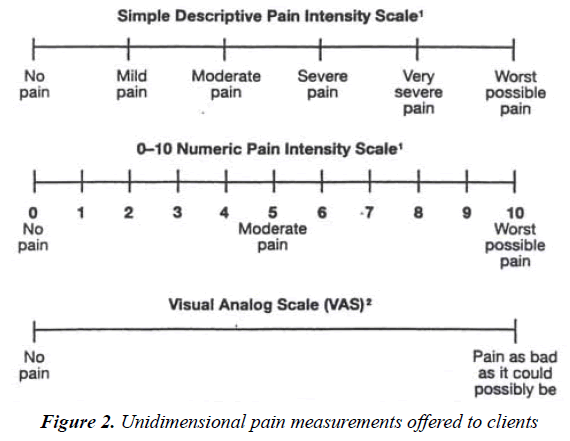
Pain is a personal, subjective experience influenced by cultural learning, the meaning of the situation, attention, and other psychological variables [52]. Patient Reported Outcomes assessments may not parallel a patient’s actual pain or disability though clients should be the ones to decide whether or not their clinical change is meaningful to them [53]. We chose measurement tools that were easily recognized and previously used by the clients in other situations. Clinical outcomes were measured using an array of three pain rating measurements tools to record reported pain levels at different intervals of the treatment process: Initial visit; start and end of every treatment sessions, and in follow-up contacts. These unidimensional pain measurements used included:
1) Simple Descriptive Pain Intensity Scale,
2) Numeric rating scale [54];
3) Visual analog scale (Figure 2).
The Numeric Pain Rating Scale Instructions General Information: The patient is asked to make three pain ratings, corresponding to current, best and worst pain experienced over the past 24 hours. The average of the 3 ratings was used to represent the patient’s level of pain over the previous 24 hours. Furthermore narrated patient-reported outcomes when asked to described their current pain, quality of life, ability to engage in daily activities, and emotional health.
Practioner Descriptor’s and Therapeutic Intervention
The author is an occupational therapist with 32 years of neurological and general rehabilitation experience in a private practice in a Midwestern state. Utilizing clinical reasoning and judgement, various manual therapies were incorporated into treatment planning in the individualized nature of a typical treatment session. Combinations of these methods were utilized for the sample group depending upon the presentation of both symptoms and tissue responses throughout the sessions:
• Upledger CranioSacral Therapy (U-CST) ranging from basic levels of 10 step protocol into advanced somatoemotional release and more subtle tissue techniques. With U-CST 10 step protocol, the techniques are designed to safely mobilize and facilitate the meningeal fields and facilitate exchanges of fluids beyond (within and around the central as well as the peripheral nervous system). Specific techniques: Thoracic inlet / horizontal plane of fascia release, frontal lift, parietal lift, sphenoid decompression [22,25,54].
• Lymphatic drainage of evacuating lymph fluids of first full body, then head/neck/torso [21]. Chikly has introduced to the manual therapy professions techniques of ‘directional mapping’ of lymph fluids aligning with the known tributaries of the lymph anatomy. More recently he has developed techniques to hypothetically treat the fluid interplay between CSF and lymphatics within the central nervous [19,21,40]. A specific method to desensitize or down regulate hyper-activated nerve fibers and ganglia is an advanced level technique.
• An advanced method emerging from the experiential work of CST is a collection of glia mobilization and glymphatic enhancement techniques [27]. Though this work also remains theoretical, the clinical outcomes are interesting to consider.
These techniques represent a synthesis and eclectic blending of gentle, non-invasive manual therapies utilized by manual practitioners worldwide [55].
Sample Group
Three adult clients, a sample of convenience from the author’s clinical practice received CST in isolation of any other treatments. All three had confirmed TN by either a medical neurologist or internist. Two clients initiated contact with the clinic specifically to treat symptoms of TN, and one client was a regular client involved in a long-term therapy process when TN first emerged. Baseline status was collected from the usual intake and history taking procedures. Treatments initiated immediately with the summarized techniques, individually applied in response to initial palpation assessment, clinical judgment and reasoning from the practitioner. Techniques were either sustained or altered or modified throughout the course of sessions based upon clients’ behavioral, verbal, and/or physical responses. Testing or treatment that held any threat of inducing or increasing pain was mindfully avoided. Responses to treatment were noted throughout and recorded at end of each session in typical daily documentation. Because of the observed outcomes and client satisfaction, long term follow-up contacts were planned for.
Client One: 63 year old female presented with two year duration of Type 1 and 2 TN symptoms and had previously sought relief through dental treatments and medication trials. Face pain was a direct result of thermal injury from prolonged exposure to weather-related extreme cold and sleet. She participated in a total of 4 therapy sessions over the span of four weeks and experience completed resolution of pain symptoms by third session. The fourth session was a follow up treatment session to maintain pain-free level achieved. Clinical follow ups were conducted at intervals of 6 months, 1 year, and 3 year post treatment.
Client Two: 66 year old female presented with bilateral Type 1 TN with co-occurring with Parkinson Disease, arthritis, bladder infection, and irritable bowel history, loss of taste and smell, light sensitivity, depression and anxiety, and chronic fatigue. She initiated treatment to specifically address TN pain and once resolved participated in ongoing treatment to address other symptoms which included: muscle rigidity, intention and resting tremors, weakness from deconditioning, depression, and generalized low grade body pains.
Client Three: 53 year old female presented with confounding and episodic symptoms post-treatment for Lyme disease.
Symptoms included: three year durations of various autoimmune flare ups, migrating nerve pains through spinal nerve roots, hypersensitivity of skin, fibromyalgia. TN symptoms first appeared follow prolonged antibiotic treatments and eventually were believed to be viral (likely post herpetic). Client had been receiving manual therapies of CST and lymphatic drainage to address these complex symptoms and specifically inquired if treatment could address this new occurrence of Type 1 and 2 TN. Four treatment sessions specifically addressing TN was provided over the course of 4 months (one per month).
Results
Each client had unique presentation of neuralgia symptoms and nerve branch involvement and all had confirmed medical diagnosis of TN by either a neurologist or internist. All three clients experienced total freedom, or manageable freedom, from severe TN pain and/or significant reduction of symptoms of their symptoms following the applications of these manual therapy methods. Duration of treatment ranged between 1–3, one-hour sessions.
Each session was unique in the techniques utilized by treating therapist based upon the daily presentation of needs. If superficial edema was present, lymphatic drainage massage was administered. If 5 grams of touch pressure (the prescribed palpation for U-CST induced pain as it did in Client #1), than another method was utilized. Having the various methods available for the therapist made each session less of a strict protocol and more like an improvisation depending upon how the body and tissues respond on the particular day. Taking these variables into account will be a factor in future study.
Summarizing the long term follow-up phone contacts revealed lasting results and/or life skills at pain management for all three clients. No further intervention required or sought by client 1 and follow up as far out as 3 years reveals her TN had not reoccurred.
Client 2 summarized in a 3 year follow up that she has not experienced the level of excruciating pain since receiving the series of U-CST. She did report that she can still feel onsets of ‘twinges’ of right sided face pain when cold air hits her face. For that reason, three years ago she trialed Gabapentin and takes it daily to prevent nerve attacks. She credits U-CST for soothing the excruciating pain and a combination of U-CST and Gabapentin for preventing future attacks. She also credits the Gamma knife procedure in lowering the extreme intensity of pain, but not eliminating it.
Client 3 asked for and was taught self-help administration of specific techniques she found the most soothing, (frontal bone lift, temporal bone decompression, Chikly nerve down-regulation and Wanveer’s methods of glymphatic drainage method. She continues to seek periodic treatment for other systemic consequences of the auto immune condition, but self-reports the trigeminal neuralgia is ‘under control’ with the combination of self-treating and taking L-Lysine during nerve flare ups apparently linked to systemic inflammation flares.
The three cases and clinical outcomes are summarized in Tables 1A-1C.
| Client # 1 | Diagnosis | Nerve distribution involved | Initial symptoms | Other treatments trialed |
|---|---|---|---|---|
| Female; age 59 | Thermal injury after face exposed for 30 minutes in sleet storm Combined TN Type 1 & 2 |
Entire V Cranial Nerve Right side: ophthalmic, maxillary, and mandibular branches |
2 years constant thumping and burning pain Initial pain level: 10 |
Occasional marginal relief from Baclofen Multiple root canals on four upper teeth = no relief of TN |
| Description of intervention: A total of 4, 1-hour manual therapy sessions over the course of 5 weeks First session: Upledger 10-step protocol techniques utilized included: cranial base release, front bone lift, parietal bone lift, sphenoid bone decompression. A reduction in pain from 10 to 5 by session’s end. Worst possible pain changed to Moderate pain. Second session: 3 days later. Pain remained consistently lowered at 4-5. Same techniques in same order of administration as session one. Unfortunately the results from the same series of techniques increased a pressure sensation in the face and by the next day pain had escalated back to 9-10. Moderate pain escalated to Worst possible pain. Third session: Client returned in 2 weeks reporting that her pain had stayed at 9-10 level since leaving the clinic from session 2. She stated she returned on the hope of again achieving at least the same level of relief achieved in the first session. This session the Chikly nerve technique and fluid mapping with gentle finger placement over greater wings of sphenoid, engaging the fascial proximity and treatment intention to follow the tissue and/or fluid tensions medially towards ganglion of cranial nerve V. This technique was the sole treatment administered for the duration of 60 minutes. Bilateral branches of cranial nerve were treated simultaneously to provide a comparison of palpation observation. Therapist subjectively observed through tactile palpation vibration and pulsations at skin level and medially into cranium, and following treatment protocol, held those tensions until they finished vibrating. Time elapsed: 50 minutes. By session end, client reported a full resolution of pain and exclaimed, “My face does not hurt at all”. Worst possible pain changed to No Pain. Fourth session: Client returned for follow up 1 week later reporting her face pain never returned after session three. Same technique applied for ‘good measure’ and the stimulation of the treatment did not exacerbate any neuralgia. Only mild vibration was palpated along any of the bilateral branches of cranial nerve V. All pain reported resolved by end of session. Follow up telephone calls were conducted at 3 intervals: 6 months, 1 year and 3 years. Client reported that her face pain did not return in any fashion or intensity since the third treatment session. Results: At all three contacts the client reported complete resolution of TN with no recurrence and a total resumption of daily life and quality of life prior to face injury. |
||||
Table 1A. Summary of treatment process and outcomes for Client #1
| Client # 2 | Diagnosis | Nerve distribution involved | Initial symptoms | Other treatments trialed |
|---|---|---|---|---|
| Female; age 66 | -Sudden TN Type 1; onset 6 months prior to CST -Parkinson with tremors and rigidity -Depression -Deconditioned state -Jaw stiffness |
-Bilateral: ophthalmic and maxillary branches -Equal severity of pain: self rated as 20 on a 1-10 scale when pain was at its worst |
-Hot poker pain exacerbated by light touch and cold temperature of air | -Gamma knife procedure 1 month after onset-marginal relief gained -Various pain medications which lowered quality of life |
| Description of intervention: Three 1-hour, weekly sessions to achieve resolution of TN pain is summarized. Two episodes of recurrence occurred over the next 18 months and were treated, reaching full pain resolution and client satisfaction with one session. Session One: U-CST techniques utilized: Thoracic inlet release, frontal lift, and sphenoid decompression. Chikly nerve regulation technique following structural tensions along facial nerve branches. Frontal lift and Chikly technique yielded immediate relief to pain intensity level. Pain level reported 8 initially and was at 5 at session’s end. Session Two: Began sessions with Chikly nerve regulation technique and discussion and dialog with client led to her insights of past frights and traumas. The opportunity arose to lead client into the technique defined by Upledger as Somato-Emotional Release. Initial pain level 8 and 3 at session’s end. Patient also reported a deep sense of relief and burden resolution of the memories of the events she processed in the session. Session Three: Chikly nerve regulation technique utilized for session’s entirety. Pain level at beginning of session: 6 and was reported as 0 at end of session Client continued to attend regular weekly sessions (an additional 6 sessions) for manual therapies to address other symptoms listed. She returned in 6 months when TN flared again. Session Ten: Recurrence of isolated right side TN pain. Reported at level 10. U-CST technique of frontal life, cranial base release, and Chikly’s nerve regulation technique completed. One hour later client reports TN pain at level 0. Follow up sessions were at the client’s discretion since travel to the clinic was problematic. She did seek local CST services and reported sporadic use, but no TN occurrences. She returned to our clinic with another TN flare up of pain 18 months later. Session Eighteen: TN symptoms had remained absent for 18 months since last session. Client returns with another flare up with facial pain restricted to right side only. She made an appointment before pain ‘ramped up too high’. Pain report at onset was 7. U-CST cranial base release, thoracic inlet technique, and Chikly nerve regulation technique applied. Pain level at end of session reported as 0. Follow up intervals were conducted either in person or by phone contact at 1 month, 6 months, 2 years of last TN treatment. The client shared a lengthy descriptive understanding of her TN. The initial occurrence was so debilitating that she was confined to her couch for an entire month taking maximal doses of various pain medications. She developed an extreme fear of moving for fear of escalating pain intensity with any input. She opted for the Gamma knife procedure on the recommendation from her neurologist. CST was initiated at the insistence of her daughter 5 months following the Gamma procedure, with outcomes reported as ‘encouraging and moderately effective’. The procedure did not eliminate the pain but it allowed me to ‘rejoin the living’. However, I was told the effects may take up to 3 months to be evident but it took a lot longer than that. When I started CST intense pain was just started to ebb. The ear pulls was a big difference it releases tension in I have since started taking Gabapentin (1 dose daily) about 2 years ago as it proved to keep the nerve pain down and stop flare ups. I won’t go off it. I have come to believe the CST loosens things up and when the tension is less the nerve is quiet. Weather changes still bother the nerve, especially cold. But I can now travel down south for winter. I’ve become accustomed to not be afraid of the twinges and twitches as I’ve learned they are telling me what I need to do for it. I don’t know if the face pain is related to the Parkinson. I have so many things going on with me. The tightness pain could be arthritis and Parkinson. CST helped relax all of that. There have been a lot of positive changes. With the fear of moving gone, I was able to join an exercise group specific for people with Parkinson’s and that really improved my ability to move and enjoy life. The CST and the Gamma knife, with the backup of the Gabapentin keep my TN away. I haven’t had a flare up in 3 years. But as soon as I feel my face tightening up I know it’s time for CST. |
||||
Table 1B. Summary of treatment process and outcomes for Client #2
| Client # 3 | Diagnosis | Nerve distribution involved | Initial symptoms | Other treatments trialed |
|---|---|---|---|---|
| Female; age 54 | -Recurring suspected herpetic neuralgia -Unspecified autoimmune disorder associated with Lyme infection treatments & recovery |
Bilateral ophthalmic branches of Cranial Nerve V | -Diffuse, burning, tingling pain -Recurring - Altered sensory perception of time, space, and balance when TN is at a 10 - Painful skin tightening |
-L-Lysine to suppress herpes outbreak -Over the counter anti-inflammatories -Curcumin for pain |
| Description of intervention: Three 1-hour sessions over the course of 12 months First session: Client is a regularly returning client, but had never experience such spontaneous bilateral face/forehead/scalp pain until first occurrence. Currently under medical care for Lyme Disease and herpes and/or shingles outbreak was an unexpected co-occurring event during treatment. Rapid pain level escalating for the days prior from 5 to 9-10 prompted the appointment. Treatment techniques utilized: Full body Chikly Lymphatic Drainage procedure completed to mobilize detox pathways; U-CST frontal and parietal lift; Chikly nerve down regulation technique. Follow up was left to the discretion of the client. Client reported taking L-lysine to suppress viral load. Reported pain level: 9-10 changed to 1-2 by session’s end. Second session: 2 months later TN pain re-occurred and client made another appointment. Pain had quickly escalated from 2-3 to 10 over a 12 hour period. Techniques utilized included: Modified Chikly lymphatic drainage protocol applied to just head and neck, Chikly’s down regulation of nerve pathway, and Wanveer’s generalized glial and glymphatic structural release techniques. No pain medications needed. L-Lysine taken after the session. Client very interested in the treatment techniques and has begun to teach her self-help methods of the same. Reported pain level: 10 changed to 0 by session’s end. Third session: 10 months later pain re-occurred following a specific anti-bacterial treatment. Pain reported to be extremely burning, tight, and pulling at a full 10 level. Upper branch of both trigeminal nerve distributions appear affected. Techniques utilized included combining Chikly’s down regulation of nerve pathway along with Wanveer’s global/generalized Glial structural release technique. Pain reported to reduce to ½ following 45 minutes of treatment. Over the counter anti-inflammatory medication taken following the session along with L-lysine dose. Client states she does not take any medications until after these treatments to test isolated results. Client was taught both techniques to test outcomes of self-help. Reported pain level: 10 changed to 0 by session’s end. Follow up at 6 months and 9 months: Client continues to be a regular attendee to address lymphatic drainage and myofascial release needs associated with her Lyme treatments. TN symptoms have flared twice but she reported being able to self-treat using Chikly nerve down-regulation method. She feels the lymphatic drainage helps clear the systemic inflammation and this may (or may not) lessen the TN flare ups. She reports CST and lymphatic drainage methods given more relief from the skin drawing up tightly and the altered sensory signals than the anti-inflammatory agents and those regular doses of L-Lysine seem to help control the nerve flare ups. |
||||
Table 1C. Summary of treatment process and outcomes for Client #3
Discussion
Trigeminal Neuralgia is a condition that is well known for its impact upon decreased quality of life and negative impact upon human productivity potential. Manual therapies are getting more attention as a treatment option for many conditions of chronic pain. CranioSacral Therapy has been clinically suggested as effective for such things as TN because the methods are believed to be able to achieve fluid motion as well as relief of meningeal and osseous restrictions near and around to the facial nerve [25]. But while evidence of the effectiveness of craniosacral therapy (CST) for pain management is growing, the efficacy of it remains unclear [56]. Improving fluid exchange and enhance drainage through manual evacuation of lymphatic and glymphatic pathways is suggested as a way to support the body’s ability to self-correct and promote healing [21,27,40].
Pain is a subjective experience influenced by cultural learning and meaning, attention, and other psychological variables. Because of this pain the patient's self-report provides the most valid measure of the experience [51]. In many situations, a simple, one-item instrument is not sufficient to truly capture pain or quality of life. Many comprehensive measures of pain exist. These instruments typically measure several dimensions of pain, with differing combinations of (among other things): pain intensity, quality, affect, interference with functioning, and effects on general quality of life. By assessing the pain experience in a more complex way, these scales may circumvent the commonly observed lack of association between pain intensity and disability [57].
The intention of this preliminary study is to highlight 3 cases of adults with Trigeminal Neuralgia where gentle, noninvasive touch and manual therapy techniques contributed to significant reduction of pain symptoms in a relatively short period of time. Outcomes reported from the medical records and follow up studies suggest all three clients attributed some or all pain relief or reduction to the manual therapies experienced. Manual therapies such as CST and lymphatic drainage may assist the mobilization and exchange of fluids as one treatment option to address idiopathic neurogenic pain. We suggest that these methods be included in considerations for future research to further explore standards of care for treatment of neuropathic pain.
Limitations
The author recognizes the strong inherent bias of this study due to the sample size and lack of any controls. Being as there was only one practitioner providing the intervention, there was no control over professional skill level of the techniques applied. There was no control over the implication that mearing touch of a therapeutic nature might alter the pain reports, though both Client #1 and Client #2, not all sessions produced full pain relief, while other sessions yielded a full resolution of TN pain. The effect of Gamma knife procedure was alluded to for Client #2 to require up to 3 months taking full effect. She reported that after 5 months, though initially helpful in reducing the intensity and severity of pain the procedure did not eliminate the pain or her fear of moving to avoid setting off a flare up. In Client #3 case we saw that she quickly asked to be taught self-care techniques so that she could try to control flare ups on her own. She demonstrated the ability to benefit from the self-care of Chikly’s nerve downregulation and Wanveer’s glymphatic drainage method. There was no control for placebo, but has Haller (2014) has demonstrated clearly, CST could easily been studied with a strong sham control in future studies.
Nonetheless measuring pain as significant as TN, it is reasonable to assume that any appreciable reduction in pain, even unidimensionally assessed and quality of life subjectively recorded, is note-worthy and clients should be the ones to decide whether or not their clinical change is actually meaningful. Though no formal quality of life measurement was included in the medical intake, specific questioning was conducted during each treatment session. In our quality of life questioning, only one of the three clients acknowledged that the pain interfered with any ability to engage in daily activities, to the point of becoming extremely fearful of moving off the couch. All three reported the TN impacted their quality of life to varying degrees. All three reported a full resolution of quality of life and ability to engage in daily occupational life.
Greater examination of the role of the lymphatic and newly emerging idea of a glymphatic system in nervous system physiology and disease is called for. Further exploration of the premise that manual therapies may be mobilizing lymph and glymphatic fluids to have a positive effect upon the CNS to bring tissues and nerves into homeostasis is justified. Manual therapists have a unique role to play in pain treatment to be with the pain and learn the structural and textural aspects associated with the client’s pain.
Through palpation the manual therapist learns the intimate and structural details associated with the pain presentation; far more telling than from verbal description alone. In the world of professional body work, various manual therapies are believed to reduce the effects of inflammation through the mechanics of evacuating fluid residuals of inflammation.
Implications for practice
It is imperative that prior to any manual therapy for TN, an accurate and differential diagnosis is made by a qualified neurologist prior to any treatment process since the condition to avoid missing vital structural issues [1,3]. In real life, learning the described therapy techniques are taught in isolation of each other in order to get through an enormous amount of information. In clinical practice, however, the wise therapist synthesizes the various methods and intertwines them into an eclectic treatment approach for their clients. Perhaps scientific inquiry could mimic what clinicians do on a daily basis by investigating the whole system instead of parts. Client responses may reflect more of the therapist’s reaction to the client’s body and tissue, rather than adhering strictly to some protocol.
References
- Singh MK. Trigeminal Neuralgia 2015.
- Cruccu G, Finnerup NB, Jensen TS, Scholz J, Sindou M, Svensson P, et al. Trigeminal neuralgia New classification and diagnostic grading for practice and research. Neurology 2016; 87: 220-8.
- Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurgical focus 2005; 18: 1-3.
- Jensen TS, Rasmussen P, Reske‐Nielsen E. Association of trigeminal neuralgia with multiple sclerosis: clinical and pathological features. Acta Neurologica Scandinavica 1982; 65: 182-9.
- Devor M, Amir R, Rappaport ZH. Pathophysiology of trigeminal neuralgia: the ignition hypothesis. The Clinical journal of pain 2002; 18: 4-13.
- Truini A, Galeotti F, Haanpaa M, Zucchi R, Albanesi A, Biasiotta A, et al. Pathophysiology of pain in postherpetic neuralgia: a clinical and neurophysiological study. Pain 2008; 140: 405-10.
- Burcheil KJ. Trigeminal neuralgia. In: Conn's Current Therapy 1999; 948-50.
- Koroshetz WJ. NINDS Trigeminal Neuralgia Information 2015.
- Lay EM. The osteopathic management of trigeminal neuralgia. The Journal of the American Osteopathic Association 1975; 74: 373.
- Yoon SZ, Lee SI, Choi SU, Shin HW, Lee HW, Lim HJ, et al. A case of facial myofascial pain syndrome presenting as trigeminal neuralgia. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2009; 107: e29-31.
- Eastman, Anne. Illustration of Trigeminal Nerve Distributions. 2015.
- Hanani M. Satellite glial cells in sensory ganglia: from form to function. Brain research reviews 2005; 48: 457-76.
- Durham PL, Garrett FG. Emerging importance of neuron-satellite glia interactions within trigeminal ganglia in craniofacial pain. Open Pain J 2010; 3: 3-13.
- Thalakoti S, Patil VV, Damodaram S, Vause CV, Langford LE, Freeman SE, et al. Neuron–glia signaling in trigeminal ganglion: implications for migraine pathology. Headache: The Journal of Head and Face Pain 2007; 47: 1008-23.
- Vit JP, Jasmin L, Bhargava A, Ohara PT. Satellite glial cells in the trigeminal ganglion as a determinant of orofacial neuropathic pain. Neuron glia biology 2006; 2: 247-57.
- Beggs S, Salter MW. Microglia: critical mediators of pain hypersensitivity after peripheral nerve injury. V: McMahon S, Koltzenburg M, Tracey I, Turk DC (ur.) Wall & Melzack’s Textbook of Pain, 6th Edition, Elsevier. 2013.
- Sofroniew MV. Astrocyte barriers to neurotoxic inflammation. Nature reviews Neuroscience 2015; 16: 249-63.
- Chikly B. Who discovered the lymphatic system?. Lymphology 1997; 30: 186-93.
- Chikly B. Silent Waves: Theory and Practice of Lymph Drainage Therapy: An Osteopathic Lymphatic Technique. IHH Pub 2004.
- Vairo GL, Miller SJ, Rier NC, Uckley WI. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. Journal of Manual & Manipulative Therapy 2013.
- Chikly BJ. Manual techniques addressing the lymphatic system: origins and development. Journal-American Osteopathic Association 2005; 105: 457.
- Upledger JE, Vredevoogd JD. Craniosacral therapy. Eastland Press; 1983.
- Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Science translational medicine 2012; 4: 147.
- Thrane VR, Thrane AS, Plog BA, Thiyagarajan M, Iliff JJ, Deane R, et al. Paravascular microcirculation facilitates rapid lipid transport and astrocyte signaling in the brain. Scientific reports 2013; 3: 2582.
- Upledger JE. Craniosacral therapy Part I: Its origins and development. Subtle Energies & Energy Medicine Journal Archives 1995; 6.
- Novey D. Clinician's Complete Reference to Complementary/alternative Medicine: Edited by Donald W. Novey. Mosby Inc; 2000.
- Wanveer, Tad. Brain Stars: Glia Illuminating Craniosacral Therapy. Upledger Productions 2015.
- Chikly B, Quaghebeur J. Reassessing cerebrospinal fluid (CSF) hydrodynamics: a literature review presenting a novel hypothesis for CSF physiology. Journal of bodywork and movement therapies 2013; 17: 344-54.
- Aspelund A, Antila S, Proulx ST, Karlsen TV, Karaman S, Detmar M, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. The Journal of experimental medicine 2015; 212: 991-9.
- Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The glymphatic system: a beginner’s guide. Neurochemical research 2015; 40: 2583-99.
- Iliff JJ, Nedergaard M. Is there a cerebral lymphatic system?. Stroke 2013; 44: S93-S95.
- Johnston M. The Importance of Lymphatics in Cerebrospinal Fluid Transport. Lymphatic Research and Biology 2004; 1: 41-45.
- Jorns TP, Zakrzewska JM. Evidence-based approach to the medical management of trigeminal neuralgia.Br J Neurosurg 2007; 21: 253-61.
- Anderson VC, Berryhill PC, Sandquist MA, Ciaverella DP, Nesbit GM, Burchiel KJ. High-resolution three-dimensional magnetic resonance angiography and three-dimensional spoiled gradient-recalled imaging in the evaluation of neurovascular compression in patients with trigeminal neuralgia: a double-blind pilot study. Neurosurgery 2006; 58: 666-73.
- Galluzzi KE. Management of neuropathic pain. The Journal of the American Osteopathic Association 2005; 105: S12-S19.
- Galluzzi KE. Managing neuropathic pain. The Journal of the American Osteopathic Association, 2007; 107: ES39-ES48.
- Pollock BE, Ecker RD. A prospective cost-effectiveness study of trigeminal neuralgia surgery. The Clinical journal of pain 2005; 21: 317-22.
- Allam N, Brasil-Neto JP, Brown G, Tomaz C. Injections of botulinum toxin type a produce pain alleviation in intractable trigeminal neuralgia. The Clinical journal of pain 2005; 21: 182-4.
- Moskalenko YE, Frymann V, Weinstein GB, Semernya VN, Kravchenko TI, Markovets SP, et al. Slow rhythmic oscillations within the human cranium: phenomenology, origin, and informational significance. Human Physiology 2001; 27: 171-8.
- Chikly, “Manual Techniques: Addressing the Lymphatic System: Origins and Development,” Journal of the American Osteopathic Association 2005; 457–64.
- Downey PA, Barbano T, Kapur-Wadhwa R, Sciote JJ, Siegel MI, Mooney MP. Craniosacral therapy: the effects of cranial manipulation on intracranial pressure and cranial bone movement. Journal of Orthopaedic & Sports Physical Therapy 2006; 36: 845-53.
- Korpiun OJ. Cranio-sacral-SELF-waves: A Scientific Approach to Craniosacral Therapy. North Atlantic Books 2011.
- Jäkel A, von Hauenschild P. A systematic review to evaluate the clinical benefits of craniosacral therapy. Complementary therapies in medicine 2012; 20: 456-65.
- Haller H, Ostermann T, Lauche R, Cramer H, Dobos GJ. Controlling for Placebo Effects in Clinical Trials of Craniosacral Therapy: Blinding Success and Credibility of a New Sham-Control Protocol. The Journal of Alternative and Complementary Medicine 2014; 20.
- Haller H, Ostermann T, Lauche R, Cramer H, Dobos G. Credibility of a comparative sham control intervention for Craniosacral Therapy in patients with chronic neck pain. Complementary therapies in medicine 2014; 22: 1053-9.
- Haller H, Lauche R, Cramer H, Rampp T, Saha FJ, Ostermann T, et al. Craniosacral Therapy for the Treatment of Chronic Neck Pain: A Randomized Sham-controlled Trial. The Clinical journal of pain 2016; 32: 441-9.
- Castro-Sánchez AM, Matarán-Peñarrocha GA, Sánchez-Labraca N, Quesada-Rubio JM, Granero-Molina J, Moreno-Lorenzo C. A randomized controlled trial investigating the effects of craniosacral therapy on pain and heart rate variability in fibromyalgia patients. Clinical rehabilitation 2011; 25: 25-35.
- Arnadottir TS, Sigurdardottir AK. Is craniosacral therapy effective for migraine? Tested with HIT-6 Questionnaire. Complementary therapies in clinical practice 2013; 19: 11-4.
- Zegarr-Parodi R, Allamand P. Osteopathic management of an adult patient suffering from trigeminal neuralgia after a post-operative Arnold Chiari type 1 decompression: Case report. International Jounral of Osteopathic Medicine 2010; 4: 136.
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. National health statistics reports 2015; 10: 1.
- Katz J, Melzack R. Measurement of pain. Surgical Clinics of North America. 1999; 79: 231-52.
- Lee JY. Measurement of Trigeminal Neuralgia Pain: Penn Facial Pain Scale. Neurosurgery Clinics of North America 2016; 27: 327-36.
- McCaffery M, Beebe A. Pain: Clinical manual for nursing practice, Mosby St. Louis, MO. 1989.
- Upledger JE. Somato Emotional Release and Beyond. UI Publishing. Palm Beach Gardens, FL. 1990
- Upledger Institute Data Base. 2015.
- Brough N, Lindenmeyer A, Thistlethwaite J, Lewith G, Stewart-Brown S. Perspectives on the effects and mechanisms of craniosacral therapy: A qualitative study of users’ views. European journal of integrative medicine 2015; 7: 172-183.
- Younger J, McCue R, Mackey S. Pain outcomes: a brief review of instruments and techniques. Current pain and headache reports 2009; 13: 39-43.