Case Report - Journal of Gastroenterology and Digestive Diseases (2017) Volume 2, Issue 3
Local recurrence from poorly differentiated transverse colon cancer treated with multidiscipline therapy: A case report.
Yoshifumi Nakayama1,2*, Masaki Akiyama1,2, Yusuke Sawatsubashi1,2, Jun Nagata1,2, Koichi Arase1,Noritaka Minagawa1, Takayuki Torigoe1, Keiji Hirata1
1Department of Surgery, School of Medicine, University of Occupational and Environmental Health. 1-1 Iseigaoka, Yahata-nishi-ku, Kitakyushu, Japan
2Department of Gastroenterological and General Surgery, Wakamatsu Hospital of University of Occupational and Environmental Health, 1-17-1 Hamamachi, Wakamatsu-ku, Kitakyushu, Japan
- Corresponding Author:
- Yoshifumi Nakayama
Department of Gastroenterological and General Surgery
Wakamatsu Hospital of University of Occupational and Environmental Health
Wakamatsu-ku, Kitakyushu
Japan
Tel: +81937610090
Fax: +81935883904
E-mail: nakayama@med.uoeh-u.ac.jp
Accepted Date: September 07, 2017
Citation: Nakayama Y, Akiyama M, Sawatsubashi Y, et al. Local recurrence from poorly differentiated transverse colon cancer treated with multidiscipline therapy: A case report. J Gastroenterol Dig Dis. 2017;2(3):21-25.
Abstract
This report describes a rare curative case of local recurrence from poorly differentiated transverse colon cancer treated with resection and chemoradiation. A 49-year-old Japanese man presented with epigastralgia, abdominal fullness and vomiting. Colonoscopy revealed advanced transverse colon cancer. Partial resection of the transverse colon with lymph node dissection and combined resection of the pancreas tail and spleen were performed because of macroscopic direct invasion to the pancreas tail from the tumor. A histopathological examination revealed poorly differentiated adenocarcinoma. Adjuvant chemotherapy was administered using 5-FU/LV. At 6 months later, CT demonstrated a hen-egg-sized mass measuring 4 cm × 3 cm in diameter at the antero-lateral side of the left kidney. Resection of this tumor was therefore performed. A histopathological examination of the tumor specimen revealed metastatic poorly differentiated adenocarcinoma. After resection of the recurrent tumor, chemoradiation was performed. Sequentially, chemotherapy was administered using an oral fluorouracil analog. The patient has been followed up in the outpatient clinic without recurrence for approximately 15 years since undergoing the operation.
Keywords
Poorly differentiated adenocarcinoma, Colon cancer, Local recurrence.
Introduction
According to the WHO grading system, poorly differentiated tumors that occupy < 50% of the area are pathologically diagnosed as poorly differentiated adenocarcinoma [1], and account for 14% to 18% of all CRC [2-4]. Poorly differentiated CRCs has been shown to predominantly located in the proximal colon [5,6], and to be more invasive and have a greater frequency of advanced-stage disease and worse prognosis than other CRCs [2-7]. Furthermore, poorly differentiated CRCs are generally considered to be associated with a high risk of lymph node metastasis as well as distant metastasis [5-7].
The reported incidence of recurrent disease after primary curative resection of CRCs ranges from 20% to 30% [8-10]. Isolated locoregional disease accounts for 5% to 19% of colon cancer recurrence and 7% to 33% of rectal cancer recurrences [11]. Relatively few studies have addressed locoregional recurrence in colon cancer [11-14]. Salvage surgery for locoregional recurrent colon cancer is appropriate for select patients [14]. However, it is very difficult to select the most suitable therapy for each case, as the pattern of locoregional recurrence differs among patients.
This report describes a curative case of local recurrence from poorly differentiated transverse colon cancer treated with multidiscipline therapy.
Case Report
A 49-year-old Japanese man patient presented with epigastralgia, abdominal fullness and vomiting. A clinical examination revealed an elastic firm, fixed, painless, hen-egg-sized tumor in his left upper abdomen. Colonoscopy revealed an ulcerated lesion of the left-sided transverse colon. He was referred to the surgical outpatient clinic to undergo treatment for advanced transverse colon cancer.
His laboratory data were as follows: white blood cell count, 6.500/mm3; hemoglobin, 14.3 g/dl; hematocrit, 41.2%; and platelets count, 305.000/mm3. He had normal electrolytes and normal blood urea nitrogen levels, but his liver function was slightly poor. His CEA and CA 19-9 levels were 2.0 ng/ml and 33.3 U/ml, respectively.
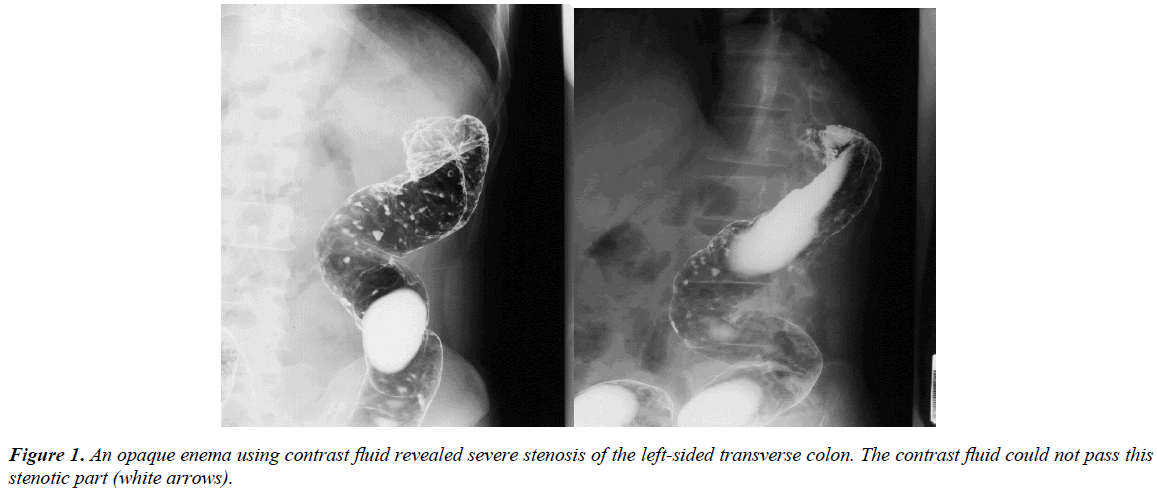
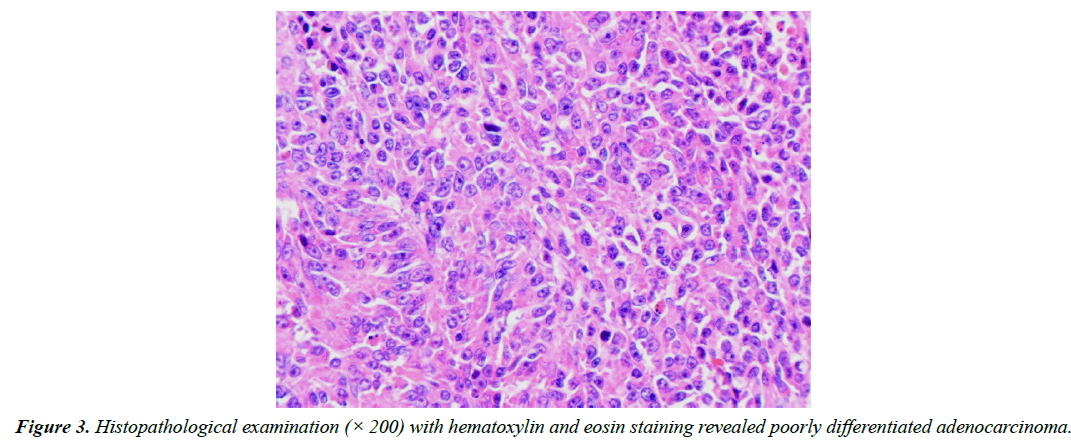
Abdominal computed tomography (CT) demonstrated wall thickness at the transverse colon nearby the splenic flexure and no evidence of distant metastasis from the transverse colon cancer. An opaque enema, using contrast fluid, revealed severe stenosis of the transverse colon nearby the splenic flexure (Figure 1). The contrast fluid could not pass through the stenosis (Figure 1). The pathological diagnosis of the biopsy specimens from this lesion indicated poorly differentiated adenocarcinoma. At laparotomy, macroscopically direct invasion to the pancreas tail from the transverse colon cancer was observed. Partial resection of the transverse colon with lymph node dissection and combined resection with pancreas tail and spleen was performed.
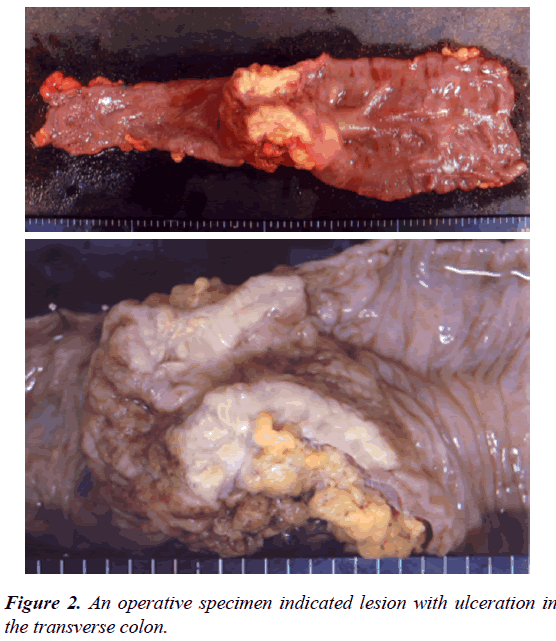
An operative specimen revealed an ulcerative lesion in the transverse colon (Figure 2). A histopathological examination with hematoxylin and eosin staining of the tumor specimen revealed poorly differentiated adenocarcinoma (Figure 3). The tumor cells were limited to the subserosal layer. No metastatic regional lymph nodes were identified. Some lymphatic and venous invasion of the carcinoma cells was also observed. The patient had an uneventful recovery and was discharged from the hospital on 21st day after surgery. Adjuvant chemotherapy was administered using 5-FU/LV.
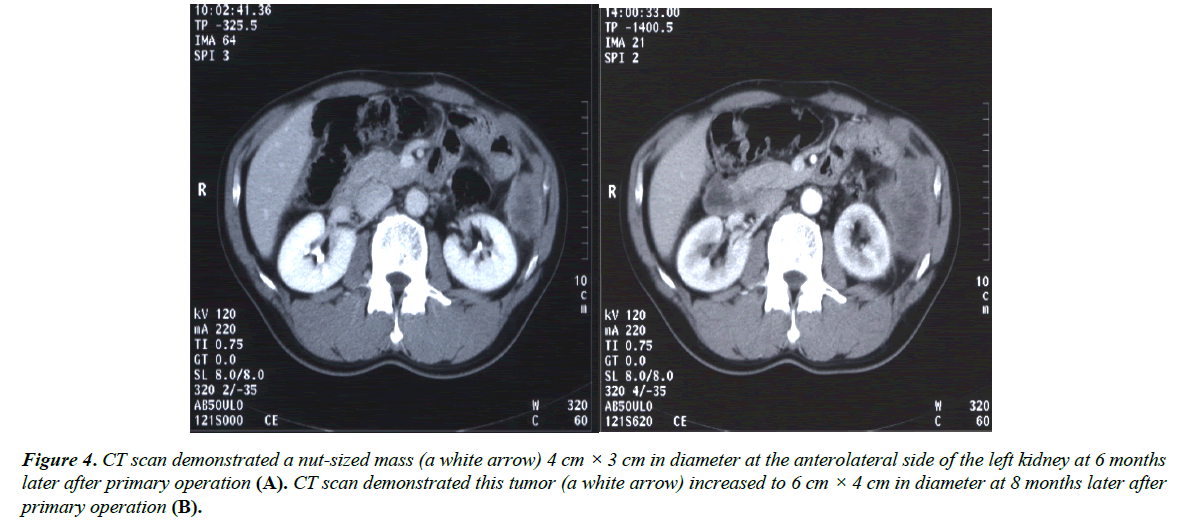
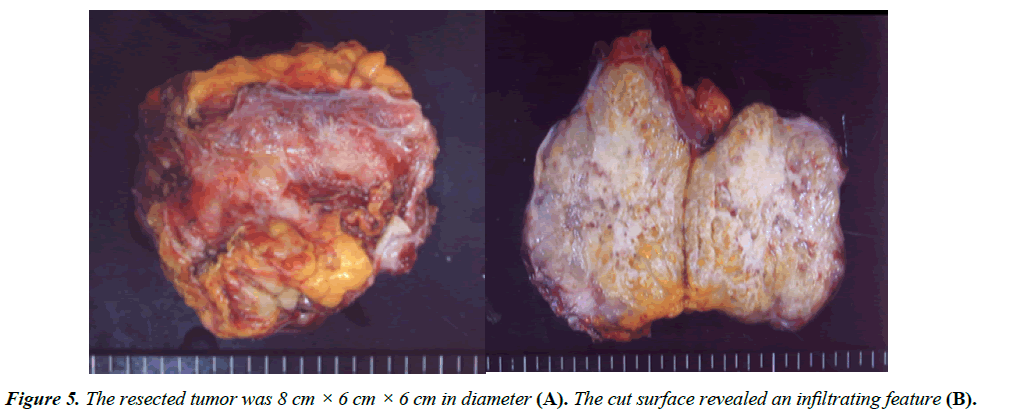
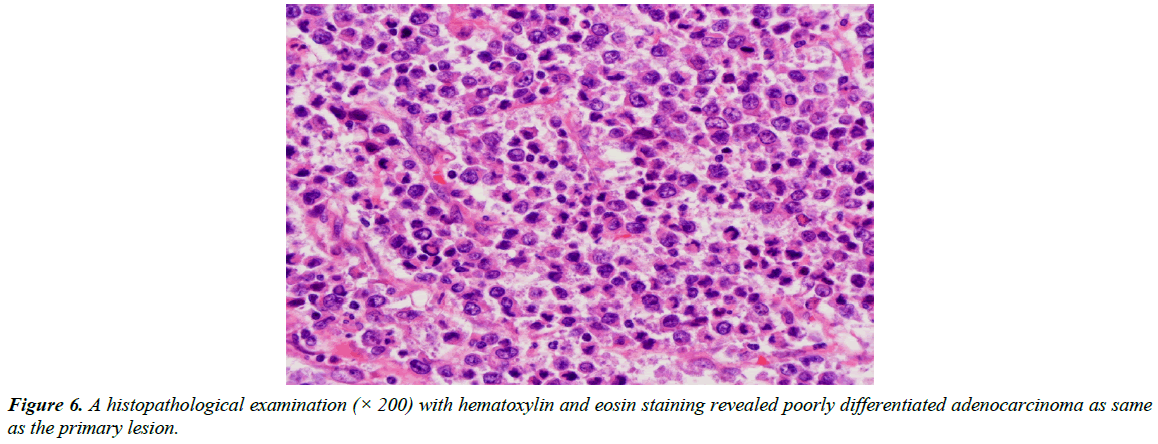
At 6 months after surgery, CT demonstrated a nut-sized mass which is 4 cm × 3 cm in diameter at the anterolateral side of the left kidney (Figure 4A). At 8 months after surgery, this tumor had increased to 6 cm × 4 cm in diameter (Figure 4B). Resection of this tumor was therefore performed. At the laparotomy, this tumor was found to have directly invaded part of the left diaphragm, so combined resection of this part was performed. The resected tumor was 8 cm × 6 cm × 6 cm in diameter (Figure 5A). The cut surface revealed infiltrating features (Figure 5B). A histopathological examination with hematoxylin and eosin staining of the tumor specimen revealed metastatic poorly differentiated adenocarcinoma like previous transverse colon cancer (Figure 6). After resection of the recurrent tumor, chemoradiation was performed. Low-dose CDDP (5 mg/day) and 5-FU (400 mg/day) administered with radiation was performed for 5 consecutive days a week. The total dose of radiation therapy was 50 Gy (2 Gy × 25 Gy). Sequentially, chemotherapy was administered using an oral fluorouracil analog.
Figure 4: CT scan demonstrated a nut-sized mass (a white arrow) 4 cm × 3 cm in diameter at the anterolateral side of the left kidney at 6 months later after primary operation (A). CT scan demonstrated this tumor (a white arrow) increased to 6 cm × 4 cm in diameter at 8 months later after primary operation (B).
The patient has been followed up in the outpatient clinic without recurrence for approximately 15 years since undergoing the operation.
Discussion
Despite apparently complete resection of the colorectal cancer, many patients develop recurrence in the area in which their primary cancer was excised and in more distant organs. There are several theories to explain such malignant recurrence including unrecognized metastasis to the lymphatic channels, shedding of cells from the primary lesion, positive margins, and mishandling of the tumor during initial resection [15]. The sites of first recurrence of CRCs include liver (more than 30%), lung (20%), locoregional disease (20% to 25%), other intraabdominal sites (15% to 20%), and elsewhere (10%) [11]. The overall recurrence rate of CRCs was 27.9%, the anastomotic recurrence rate was 11.7%, and the distant metastasis rate was 14.4% [16]. The local recurrence rate after curative resection of the colon cancer is 3.1%-5.4%, and that of rectal cancer is 16.7% [16,17]. The average time to local recurrence is 13.0 to 21.3 months [16,17]. Although the average time for recurrences is about two years, very aggressive tumors can recur within six months to a year [18]. If no disseminated disease is found, patients deemed candidates for re-excision.
Tumor differentiation was found to be related to local recurrence of colon cancer, with no instances in well-differentiated tumors, a recurrence rate of 2.8% in moderately differentiated tumors, and a rate of 6.8% in poorly differentiated tumors [17]. Ricciardi et al. indicated that CRC patients with poorly differentiated tumors were much more likely to be nodepositive (52%) than those with well-differentiated tumors (29%) [6]. Furthermore, the prognosis of CRC patients with poorly differentiated adenocarcinoma is typically reported to be poor and more unfavorable than in patients with well or moderately differentiated adenocarcinoma [19,20].
Factors associated with a prolonged disease-specific survival in locoregional recurrent colon cancer included R0 resection (p< 0.001), age< 60 (p< 0.01), an early stage of primary disease (p=0.05), and no associated distant disease (p=0.030) [10]. Poor prognostic factors included more than 1 site of recurrence (p=0.05) and the involvement of the mesentery/ nodal basin (p=0.03) [10]. Complete resection of the recurrent tumor is critical to the long-term survival and is associated with a single site of recurrence, perianastomotic disease, low pre-salvage carcinoembryonic antigen level, and absence of distant disease [10].
Surgery for recurrent disease has been reported in the literature to have a 5-year survival rate of up to 30% [10,12,21,22]. However, it is well known that the chemotherapy for CRCs has significantly improved in the last decade and may have contributed to successful outcomes. Radiation therapy has also been used either alone or in combination with chemotherapy as an adjuvant after surgery to reduce the risk of recurrence. Willett et al. reported an improved survival in patients treated with adjuvant external beam radiotherapy following surgery for locally advanced colon cancer [23]. A multimodality approach using en bloc surgical resection with radiotherapy and chemotherapy affords some patients with locally advanced and recurrent colon cancer a chance for a long-term survival [22]. Taylor et al. indicated that seventy-three patients treated for recurrent colon carcinoma had a median survival of 33.3 months from the time of recurrence, with a 5-year survival of 24.7%. Of note, the 38 patients with recurrent disease whose disease was completely resected had a 37.4% 5-year survival rate [22].
Conclusion
This report presents a rare curative case of local recurrence from poorly differentiated transverse colon cancer treated with local resection and chemoradiation. Multidiscipline therapy may be needed to treat the local recurrence of poorly differentiated colon cancer.
References
- Bruckner HW, Piterlli J, Merrick M. Carcinoma of the colon and rectum. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, (eds). WHO Classification of Tumors of the Digestive System. Lyon* IARC Press, France. 2010:138-9.
- Chung CK, Zaino RJ, Stryker. Colorectal carcinoma: Evaluation of histologic grade and factors influencing prognosis. J SurgOncol. 1982;21(3):143-8.
- Umpledy HC, Bristol JB, Rainey JB, et al. Survival of 727 patients with single carcinomas of the large bowel. Dis Colon Rectum. 1984;27(12):803-10.
- Bjerkest T, Morild S, Mork S, et al. Tumor characteristics in colorectal cancer and their relationship to treatment and prognosis. Dis Colon Rectum. 1987;30(12):934-8.
- Imai Y. Poorly differentiated adenocrcinoma of the colon: subsite location and clinicopathologic features. Int J Colorectal Dis. 2015;30(2):187-96.
- Ricciardi R, Madoff RD, Rothenberger DA, et al.Population-based analyses of lymph node metastasis in colorectal cancer. Clin Gastroenterol Hepatol. 2006;4(12):1522-7.
- Komori K, Kanemitsu Y, Ishiguro S, et al. Clinicopathological study of poorly differentiated colorectal adenocarcinoma: Comparison between solid-type and non-solid-type adenocarcinoma. Anticancer Res. 2011;31(10):3463-8.
- Fuzun M, Terzi C, Sokmen S, et al. Potentially curative resection for locoregional recurrence of colorectal cancer. Surg Today. 2004;34(11):907-12.
- Meyers M, Sasson A, Sigurdson E. Locoregional strategies for colorectal hepatic metastasis. Clin Colorectal Cancer. 2003;3(1):34-44.
- Bowne W, Lee B, Wong W, et al. Operative salvage for locoregional recurrent colon cancer after curative resection: An analysis of 100 cases. Dis Colon Rectum. 2005;48(5):897-909.
- Turk PS, Wanebo HJ. Results of surgical treatment of nonhepatic recurrence of colorectal carcinoma. Cancer. 1993;71(12):4267-77.
- Gwin J, Hoffman J, Eisenberg B. Surgical management of nonhepatic intra-abdominal recurrence of carcinoma of the colon. Dis Colon Rectum. 1993;36(6):540-4.
- Goldberg RM, Fleming TR, Tangen CM, et al. Surgery for recurrent colon cancer: Strategies for identifying resectable recurrence and success rates after resection. Annals of Internal Med. 1998;129(1):27-35.
- Stipa S, Nicolanti V, Botti C, et al. Local recurrence after curative resection for colorectal cancer: Frequency, risk factors and treatment. J SurgOncol. 1991;2:155-60.
- Sagar P, Pemberton J. Surgical management of locally recurrent rectal cancer. Br J Surg. 1996;83(3):293-304.
- Obrand DI, Gordon P. Incidence and patterns of recurrence following curative resection for colorectal carcinoma. Dis Colon Rectum. 1997;40(1):15-24.
- Harris GJ, Church JM, Senagore AJ, et al. Factors affecting local recurrence of colonic adenocarcinoma. Dis Colon Rectum. 2002;45(8):1029-34.
- Waldron RP, Donovan IA. Clinical follow-up and treatment of locally recurrent colorectal cancer. Dis Colon Rectum. 1987;30(6):428-30.
- Takeuchi K, Kuwano H, Tsuzuki Y, et al. Clinicopathological characteristics of poorly differentiated adenocarcinoma of the colon and rectum. Hepatogastroenterol. 2004;51(60):1698-702.
- Sugao Y, Yao T, Kubo C, et al. Improved prognosis of solid-type poorly differentiated colorectal adenocarcinoma: A clinicopathological and immunohistochemical study. Histopathology. 1997;31(2):123-33.
- Minton JP, Hoehn JL, Gerber DM. Results of a 400-patient carcinoembryonic antigen second look colorectal cancer study. Cancer. 1985;55(6):1284-90.
- Taylor W, Donohue JH, Gunderson LL, et al. The Mayo Clinic experience with multimodality treatment of locally advanced or recurrent colon cancer. Ann Surgical Oncol. 2002;9(2):177-85.
- Willett CG, Fung CY, Kaufman DS, et al. Postoperative radiation therapy for high-risk colon carcinoma. J ClinOncol. 1993;11(6):1112-7.