Research Article - Journal of Bacteriology and Infectious Diseases (2018) Journal of Bacteriology and Infectious Diseases (Special issue 1-2018)
Evaluation of Inhibitory Zone Diameter (IZD) of crude Spondias mombin (Linn.) extracts (root, leaf, and stem bark) against thirty infectious clinical and environmental isolates.
Oludare Temitope Osuntokun*Department of Microbiology, Adekunle Ajasin University, Akungba Akoko, Ondo State, Nigeria
- *Corresponding Author:
- Oludare Temitope Osuntokun
Department of Microbiology
Adekunle Ajasin University
Akungba Akoko
Ondo State
Nigeria
Tel: 08063813635
E-mail: oludare.osuntokun@aaua.edu.ng
Accepted Date: February 22, 2018
Citation: Osuntokun OT. Evaluation of Inhibitory Zone Diameter (IZD) of crude Spondias mombin (Linn.) extracts (root, leaf, and stem bark) against thirty infectious clinical and environmental isolates. J Bacteriol Infec Dis. 2018;2(1):8-16
Abstract
The purpose of this research work is to evaluate the Inhibitory Zone Diameter (IZD) of crude Spondias mombin extracts against thirty infectious clinical and environmental organisms. The root, leaf and stem-bark of S. mombin were harvested and air-dried. The dried S. mombin was milled into powdered form using manual grinder. Powdered S. mombin (1kg) each of the different S. mombin parts was extracted with 3 L of 70% (v/v) ethanol, ethyl acetate and distilled water for 72 h at room temperature. The antimicrobial assay of crude Spondias mombin extracts on the test bacteria was determined by the agar diffusion method. A 0.1 ml of 1:10,000 dilutions (equivalent to 106 cfu /ml) of fresh overnight broth culture of the test bacteria was seeded on molten Mueller-Hinton agar plate. Using a sterile cork borer of 6 mm diameter, equidistant wells were bored on the agar. One millimeter of the various re-suspended extracts (7.5, 15, 30 and 60 mg / ml) was introduced into the wells. Ofloxacin (5 µg) was used as control. The plates were then incubated at 37°C for 24 to 48 hours. Antifungal assay of crude root, leaf, and stem bark of Spondias mombin extracts were determined using Agar well diffusion method. A 5- day old fungal culture on potato dextrose agar (PDA) was flooded with 2 ml of sterile distilled water containing 3% glycerol. The spores were harvested by scraping with a sterile inoculating loop. Sterile PDA plates were inoculated with 0.1 ml of the fungal spore suspension using the spread plate technique. Five wells were bored on the potato dextrose agar (PDA) plates using a 6 mm sterile cork borer. The plates were allowed to stand on the bench for 1 hour before incubating at 25°C for 5 days. Diameter of zones of growth inhibition was then measured in millimeter with a vernier caliper. Aqueous leaf extract of S.mombin had the zone of inhibition of 23 mm against B. cepacia at 60 mg/ml. The aqueous stem bark and root of S. mombin extracts at 60 mg/ ml had the highest zone of inhibition of 23 mm, each against C. koseri and K. ozaenae. However, the aqueous Stem bark extract of S.mombin did not show any antibacterial activity against M. abscessus neither did the aqueous root extract show antibacterial activity against E. coli. This study revealed that the plant extracts possessed antibacterial and antifungal activities against some highly infectious clinical and environmental pathogens which justified their use in ethnomedicine for treatment of infectious diseases.
Introduction
Spondias mombin linn is a small tree that grows up to 20 m (60 ft.) high and 1.5 m (5 ft.) in girth, moderately buttressed; stem bark is thick, corky, deeply fissured, slash pale pink, darkening rapidly, branchlets glabrous; leaves pinnate, leaflets 5-8 opposite pairs with a terminal leaflet. It belongs to the family Anacardiaceae. It flowers develop between January - May and fruits between July-September, The fruits have a sharp, somewhat acid taste and are edible. The matured fruit has a leathery skin and a thin layer of pulp. The fruit pulp is either eaten fresh, or made into juice, concentrate, jellies, and sherbets. The fruit-juice is used as a febrifuge and diuretic. The roots are also used as febrifuge in Ivory Coast. The bark is used as a purgative and in local applications in the treatment of leprosy. The stem bark decoction is also used in the treatment of severe cough. It serves as an emetic, a remedy for diarrhea, dysentery, hemorrhoids and a treatment for gonorrhea and leucorrhea [1]. The decoction of the astringent stem bark is believed to expel calcifications from the bladder. The juice of crushed leaves and the powder of dried leaves are used on wounds and inflammations. The gum is employed as an expectorant and to expel tapeworms [2]. A decoction of the mashed leaves is used by the Ibos (Nigeria) for washing a swollen face. A leaf infusion is a common cough remedy or used as a laxative for fever with constipation. A leaf decoction is used in treatment of gonorrhea. The leaves are used in Ivory Coast for fresh wounds to prevent inflammation [3].
Nworu et al. [4], were the first to formulate groupings of genera in the Anacardiaceae, dividing the family into two tribes, the Anacardieae and Spondieae [sic]. Subsequently, Mitchell et al. [5], published the tribe Spondiadeae was the first to formulate a relatively modern concept of Spondias, in which he included Evia Blume, Cytheraea Wight & Arn., and Wirtgenia Jung. ex Hassk. (nom. illegit., non Wirtgenia Sch. Bip.).
The pulp of the fruit is sometimes eaten directly, especially when found in the forest, but is too acid to be considered attractive; it can also be boiled or dried. It is especially used for syrup, ice cream, drinks and jellies. Juices improve with keeping overnight as the mild astringency of the fresh fruit disappears. Fermented products are also good. The fruit is a good source of vitamins A and C; vitamin C quantities vary between 34 and 54 mg/g, and carotenoids are presumably present in reasonable concentrations. There is great variation in fruit quality from region to region, some being sweet and pleasant and others quite disagreeable in flavor [6]. Nworu et al. [4], reported the several uses of the plant based on oral communication and not on any recorded scientific investigation. Infusion of its leaves has been used since long time, without any report of collateral effects, due to its activity.
Materials and Methods
Chemical and reagent
All chemical reagents were of analytical grade and purchased from Sigma chemical company Limited United kindom (UK).
Microorganism for the research work
Thirty clinical and environmental microorganisms were used for this research work, which comprised 20 bacteria and 10 fungi. The breakdown of the thirty organisms used include; 10 typed bacterial isolates,10 locally isolated bacteria and 10 locally isolated fungi. The typed test bacteria included Mycobacterium fortuitum ATCC 6841, Mycobacterium smegmatis ATCC 19420, Mycobacterium abscessus ATCC 19977, Mycobacterium phlei ATCC 19240, Staphylococcus aureus ATCC 29213, Escherichia coli ATCC 25922, Klebsiella pneumoniae ATCC 35659, Salmonella typhi ATCC 35723, Pseudomonas aeruginosa ATCC 25619, and a fungus, Candida albican ATCC 90029. The locally isolated bacteria include Salmonella choleraesuis, Salmonella arizonae, Proteus mirabilis, Aeromonas hydrophilia, Bacillus subtilis, Salmonella typhi, Shigella dysenteriae, Burkholderia cepacia, Citrobacter koseri and Klebsiella ozaenae. The test fungi include Aspergillus niger, Fusarium solani, Saccharomyces cerevisiae, Aspergillus flavus, Phytophera megakarya, Candida kruise, Rhizopus stonifer, Trichoderma horizionum, Fusarium vortercelium and Syncephalastrum racemosum.
Sources of microorganisms
All typed strains used for this research work were purchased from the University of Pennsylvania, School of Medicine, Philadelphia, United States of America (USA), in an America Type Culture Collection (ATCC), and the other locally isolated bacteria and fungi were clinical organisms collected from Central Medical Laboratory (CML), Obafemi Awolowo University Teaching, Hospital (OAUTH), Ile Ife, Osun State, and the Institute of Advance Medical Research and Training (IMRAT), University College Hospital, Ibadan, Oyo State Nigeria. All isolates were from the clinical sources which include wound infection, Urinary tract infection, Upper respiratory tract infection, pneumonia cases, gastrointestinal disorder (diarrhea) and skin infection.
Authentication of test microrganisms
The identity of the test organisms was confirmed using Biomerieux API 20E Kits for bacteria as specified by the manufacturer’s instruction. The test fungi were authenticated by ID 32 C system (Biomerieux, France) following the manufacturer’s instructions. The yeast isolates were identified by the ID 32 C Analytical Profile Index [7].
Standardization of organisms: The organisms were standardized using a serial dilution technique i.e., the stock sample on a slant was introduced in an already prepared nutrient broth and incubated overnight (18-24 hours). A 0.1 ml of the broth was introduced into 9.9 ml of sterile distilled water to make a dilution of 1:1000 and also from the dilution; another 0.1 ml was pipetted into 9.9 ml of sterile distilled water to make a dilution of 1:10,000. It was then standardized according to National Committee for Clinical Laboratory Standards [8] by adding normal saline gradually and its turbidity compared with McFarland standard of 0.5 which was approximately (1.0 × 106 Cfu /ml). The same procedure was repeated for the fungi using potatoes dextrose broth.
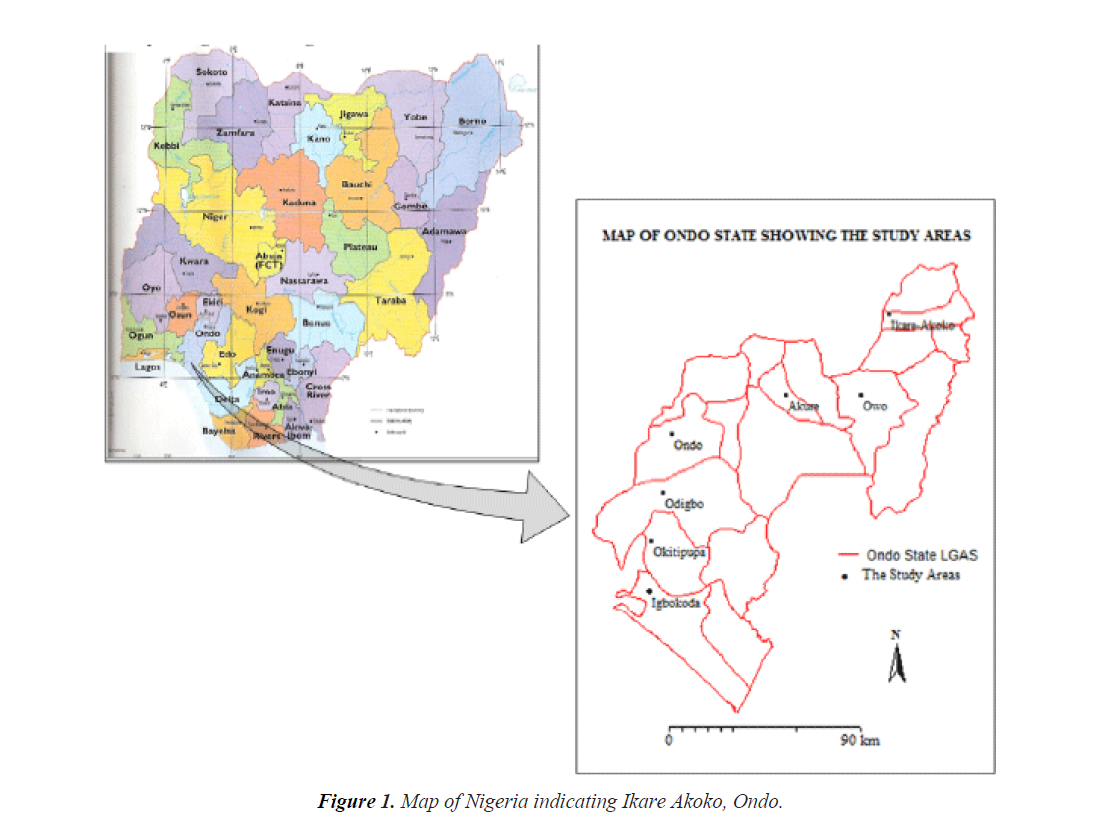
Collection of plant materials
The root, leaf, and stem bark of Spondias mombin tree were harvested early in the morning into a polythene bag at Oja Oba market, Ikare Akoko, Ondo State, a tropical rainforest of Ondo State, Nigeria with latitude (7.21692 North) and longitude (5.21561 East). The plant was authenticated at the herbarium of the Department of Pharmaceutical chemistry, Obafemi Awolowo University, Ile -Ife, Osun State, Nigeria and voucher was deposited. A voucher number was issue at the herbarium for proper documentation (DPC-SPM 0340) (Figure 1).
Preparation and extraction of Spondias mombin plant
The root, leaf and stem-bark of Spondias mombin plant were harvested and air-dried. The dried leaves were milled into powdered form using manual grinder. Powdered plant material (1 kg) each of the different plant parts was extracted with 3 L of 70% (v/v) ethanol, ethyl acetate and distilled water for 72 h at room temperature. The extraction process was repeated four times until the extract became clear. The filtrates were combined and concentrated under reduced pressure Rotatory Evaporator at 35°C to give, SMRE, SMREA and SMRAQ for root part; SMLE, SMLEA and SMLAQ for the leaf part; and SMSBE, SMSBEA and SMSBAQ for the stem-bark part. The dry extracts were kept in tightly stoppered bottles in a refrigerator at 20°C for further analysis.
Antimicrobial assay of Spondias mombin extracts
The antimicrobial activities of the Spondias mombin extracts were assessed on the test organisms. The test bacteria and fungi were selected on the basis of the diseases against which Spondia mombim was used. The antibacterial assay of the extracts was determined by the agar well diffusion method [9].
Antibacterial assay of crude Spondias mombin extracts (root, leaf, and bark): The antimicrobial assay of crude Spondias mombin extracts on the test bacteria was carried out by the agar diffusion method [9]. A 0.1 ml of 1:10,000 dilutions (equivalent to 106 cfu /ml) of fresh overnight broth culture of the test bacteria was seeded on molten Mueller-Hinton agar plate. Using a sterile cork borer of 6 mm diameter, equidistant wells was made in the agar. One millimeter of the various re-suspended extracts (7.5, 15, 30 and 60 mg/ml) was introduced into the wells. Ofloxacin (5 μg) was used as control. The plates were allowed to stand on the bench for 1 hour, to allow pre-diffusion of the extracts before incubation. The plates were then incubated at 37°C for 24 to 48 hours. The zones of inhibition were measured to the nearest millimeter (mm) using a transparent ruler.
Antifungal assay of crude of Spondias mombin extracts (root, leaf, and stem bark): Antifungal assay of crude root, leaf, and stem bark of Spondias mombin extracts was done using Agar well diffusion method. A 5-day old fungal culture on potato dextrose agar (PDA) was flooded with 2 ml of sterile distilled water containing 3% glycerol. The spores were harvested by scraping with a sterile inoculating loop. Sterile PDA plates were inoculated with 0.1 ml of the fungal spore suspension using the spread plate technique. Five wells were bored on the potato dextrose agar (PDA) plates using a 6 mm sterile cork borer. The first, second, third and fourth well were filled with 60, 30, 15 and 7.5 mg/ml of the extracts, respectively, while the fifth well was filled with fluconazole which served as control. The plates were allowed to stand on the bench for 1 hour before incubating at 25°C for 5 days. Diameter of zones of growth inhibition was then measured in millimeter with a vernier caliper [10].
Determination of minimum inhibitory concentration (MIC) of crude Spondias mombin extracts (root, leaf, and stem bark): A serial dilution of the extracts ranging from 1:10 to 10.009 was made. The bacterial strain was cultured in Muller Hinton broth and suspended in 5 ml peptone water. To the suspension, 5 ml of each extract concentration was added into Muller Hinton broth and then 1.0 ml of standardized broth culture containing 1.0 × 106 cfu/ml was introduced into each test tube and then incubated at 37°C for 18–24 hrs. Following incubation, turbidity was examined; the concentration at which no turbidity was observed was regarded as the MIC value [11].
Determination of minimum bactericidal concentration (MBC) of crude Spondias mombin extracts (root, leaf, and stem bark): Suspensions from the MICs were used for the MBC determination. A bacterial streaking of equal streaks was made from the MIC test tubes onto Mueller-Hinton agar plates and the procedure was repeated all through the required numbers of the corresponding isolates. The isolated organism on the Mueller-Hinton agar was incubated at 37°C for 18–24 hrs. After incubation, the plates were observed; the concentration that exhibited no bacterial growth was considered as the MBC [11].
Results
Antimicrobial activities of Spondias mombin extracts
Tables 1 and 2 shows the diameter of zones of growth inhibition of leaf, stem bark and root crude extracts of S. mombin on the test bacteria and fungi at concentrations of 60, 30, 15 and 7.5 mg/ml, respectively. Aqueous leaf extract of S. mombin had the zone of inhibition of 23 mm against B. cepacia at 60 mg/ ml. The aqueous stem bark and root of S. mombin extracts at 60 mg /ml had the highest zone of inhibition of 23 mm each against C. koseri and K. ozaenae. However, the aqueous Stem bark extract of S. mombin did not show any antibacterial activity against M. abscessus neither did the aqueous root extract show antibacterial activity against E. coli. The aqueous leaf and root extracts of S.mombin did not show any zone of growth inhibition against P. megakarya and T.horizionum at 7.5 mg/ ml (Table 1). The MIC and MBC) of the aqueous leaf, root and Stem bark extracts on all the susceptible test bacteria was 15 mg/ml and 7.5 mg/ml, respectively (Table 1). Meanwhile, the MIC and MFC of the aqueous leaf, root and stem bark extracts on all the susceptible test fungi were 30 mg/ml and 15 mg/ml, respectively (Table 2).
Table 1.Diameter of zones of inhibition of crude aqueous extracts of Spondias mombin on the test bacteria.
| Diameter of zone of growth inhibition (mm) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LEAF | ROOT | STEM BARK | ||||||||||||||
| Bacteria | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin(5 µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin(5 µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin(5 µg) | MIC (15 mg/ml) , MBC (7.5 mg/ml) |
| Mycobacterium fortuitum | 17 | 9 | 7 | 3 | 28 | 18 | 7 | 4 | 2 | 25 | 17 | 10 | 6 | 4 | 27 | |
| Mycobacterium smegmatis | 18 | 11 | 7 | 4 | 27 | 17 | 7 | 3 | 2 | 25 | 19 | 6 | 4 | 2 | 24 | |
| Mycobacterium abscessus | 19.0) | 6 | 4 | 2.0) | 27 | 10 | 4 | 2 | 0 | 32 | 19 | 5 | 3 | 4 | 32 | |
| Mycobacterium phlei | 14 | 6 | 2 | 1 | 24 | 14 | 6 | 3 | 1 | 25 | 20 | 6 | 4 | 2 | 29 | |
| Staphylococcus aureus | 15 | 10 | 6 | 4 | 23 | 15 | 10 | 7 | 3 | 25 | 14 | 10 | 5 | 2 | 29 | |
| Escherichia coli | 17 | 13 | 7 | 3 | 25,0 | 12 | 6.0. | 3 | 2 | 26 | 21 | 6 | 3.0) | 0 | 24 | |
| Klebsiella Pneumoniae | 13 | 7 | 4 | 3 | 23 | 13 | 7 | 5 | 2 | 25 | 19 | 7 | 4 | 2 | 27 | |
| Salmonella typhi | 17 | 11 | 6 | 2 | 22 | 13 | 8 | 5 | 3 | 25 | 19 | 17 | 6 | 3 | 26 | |
| Pseudomonas aeruginosa | 19 | 12 | 7 | 4 | 21 | 14 | 10 | 6 | 3 | 20 | 17 | 11 | 7 | 2 | 23 | |
| Salmonella choleraesuis | 12 | 9 | 7 | 5 | 20 | 13 | 10 | 8 | 6 | 20 | 15 | 10 | 9 | 9 | 19 | |
| Salmonella arizonae | 21 | 18 | 17 | 5 | 21 | 21 | 18 | 17 | 5 | 22 | 21 | 18 | 15 | 9 | 22 | |
| Proteus mirabilis | 21 | 19 | 17 | 8 | 22 | 18 | 16 | 15 | 6 | 23 | 18 | 17 | 9 | 6 | 19 | |
| Aeromonas hydrophilia | 19 | 14 | 6 | 2 | 20 | 15 | 11 | 7 | 2 | 20 | 13 | 6 | 4 | 2 | 18 | |
| Bacillus subtilis | 17 | 12 | 9 | 5 | 18 | 17 | 10 | 7 | 4 | 20 | 19 | 10 | 7 | 4 | 19 | |
| Salmonella typhi | 12 | 9 | 5 | 3 | 1.5 | 19 | 13 | 7 | 4 | 20 | 18 | 12 | 7 | 4 | 17 | |
| Shigella dysenteriae | 18 | 15 | 10 | 4 | 21 | 20 | 19 | 15 | 9 | 22 | 21 | 18 | 12 | 6 | 20 | |
| Burkholderia cepacia | 23 | 19 | 8 | 3 | 26 | 21 | 17 | 8 | 5 | 25 | 18 | 10 | 6 | 2 | 25 | |
| Citrobacter koseri | 22 | 10 | 7 | 1 | 26 | 23 | 18 | 12 | 5 | 25 | 23 | 20 | 10 | 7 | 21 | |
| Klebsiella ozaenae | 20 | 16 | 9 | 3 | 21 | 23 | 20 | 15 | 5 | 19 | 20 | 19 | 15 | 6 | 19 | |
P value- <0.0001, P value summary**** Differences significant (P <0.05), significantly different standard deviations (P <0.05), MIC (1mg/ml), MBC (7.mg/ml)
Table 2.Diameter of zones of inhibition of crude aqueous extracts of Spondias mombin on the test fungi.
| Diameter of zone of growth inhibition (mm) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LEAF | ROOT | STEM BARK | ||||||||||||||
| Fungi | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole (5 µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole(5 µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole(5 µg) | MIC: Minimum Inhibitory Concentratio-30 mg/ml), |
| Aspergillus niger | 17 | 15 | 8 | 4 | 20 | 19 | 15 | 9 | 5 | 21 | 19 | 13 | 8 | 3 | 18 | |
| Candida albican | 18 | 8 | 6 | 3 | 26 | 11 | 8 | 5 | 2 | 25 | 17 | 8 | 4 | 2 | 27 | |
| Fusarium Solani | 18 | 16 | 12 | 7 | 19 | 15 | 12 | 8 | 3 | 17 | 19 | 17 | 10 | 8 | 20 | |
| Saccharomyces cerevisiae | 19 | 15 | 10.0) | 6 | 22 | 18 | 15 | 13 | 7 | 20 | 18 | 15 | 10 | 7 | 22 | |
| Aspergillus flavus | 18 | 15 | 10 | 7 | 20 | 18 | 14 | 9 | 5 | 23 | 18 | 14 | 8 | 4 | 21 | |
| Phytophera megakarya | 5.0) | 2 | 1 | 0 | 19 | 10 | 5 | 2 | 0 | 19 | 0 | 0 | 0 | 0 | 20 | |
| Candida kruise | 19 | 15 | 10 | 6 | 22 | 20 | 15 | 8 | 3 | 22 | 18 | 17 | 10 | 5 | 20 | |
| Rhizopus stonifer | 7 | 5 | 2 | 1 | 15 | 15 | 12 | 10 | 7 | 16 | 0 | 0 | 0 | 0 | 16 | |
| Trichoderma horizionum | 10 | 5 | 2 | 0 | 18 | 18 | 15 | 11 | 9 | 20 | 0 | 0 | 0 | 0 | 15 | |
| Fusarium vortercelium | 18 | 15 | 10 | 9 | 21 | 16 | 12 | 7 | 3 | 19 | 20 | 17 | 12 | 10 | 22 | |
| Syncephalastrum Racemosum | 17 | 12 | 9 | 4 | 22 | 16 | 12 | 8 | 3 | 23 | 15 | 12 | 7 | 2 | 20 | |
Note: MIC: Minimum Inhibitory Concentratio-30 mg/ml), MFC: Minimum Fungicidal Concentration -15 mg/ml, P value- < 0.0001, P value summary**** Significantly different standard deviations (P <0.05)
The antibacterial activity of crude ethyl acetate extracts of S. mombin (Leaf, Stem-bark and Root) at concentrations of 60, 30, 15 and 7.5 mg/ml is represented in Tables 3 and 4. The diameter of zones of growth inhibition varied with the various test bacteria with significant activity observed at 60 mg/ml, with the highest inhibition zone of 30.0 mm against S. choleraesuis. The root extract exhibited considerable level of antimicrobial activity with the zone of inhibition of 23.0 mm each against C. koseri and B.cepacia (Table 3). The ethanolic extracts (Leaf, root and stem bark) demonstrated varied antibacterial and antifungal activity against the test bacterial and fungi (Tables 5 and 6). However, the leaf extract at all the concentrations used did not show any zone of antifungal inhibition against R. stonifer, likewise against P. megakarya at 15. 0 and 7.5 mg/ml, respectively (Table 6).
Table 3.Diameter of zones of inhibition of crude ethyl acetate extracts of Spondias mombin on the test bacteria.
| Diameter of zone of growth inhibition (mm) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LEAF | ROOT | STEM BARK | ||||||||||||||
| Bacteria | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin (5 µg ) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin (5 µg ) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin (5 µg ) | MIC (15mg/ml) , MBC (7.5mg/ml) |
| Mycobacterium fortuitum | 15 | 10 | 6 | 4 | 29 | 12 | 8 | 4 | 2 | 26 | 20 | 8 | 6 | 4 | 28 | |
| Mycobacterium smegmatis | 17 | 13 | 7 | 3 | 28 | 14 | 9 | 6 | 3 | 28 | 17 | 13 | 7 | 3 | 28 | |
| Mycobacterium abscessus | 13.0( | 8 | 4 | 2 | 34 | 10 | 4 | 2 | 0 | 32 | 18 | 6 | 4 | 2 | 35 | |
| Mycobacterium phlei | 14 | 6 | 3 | 1 | 25 | 11 | 7 | 4.0) | 20 | 27 | 18 | 6 | 3 | 2 | 28 | |
| Staphylococcus aureus | 17 | 11 | 7 | 4 | 25 | 16 | 8 | 4 | 2 | 27 | 14 | 17 | 4 | 2 | 26 | |
| Escherichia coli | 15 | 10 | 6 | 5 | 24 | 12 | 6 | 3 | 3 | 26 | 10 | 5 | 3 | 1 | 27 | |
| Klebsiella Pneumoniae | 13 | 7 | 2 | 6 | 26 | 14 | 7 | 3 | 4 | 24 | 15 | 8 | 4 | 3 | 23 | |
| Salmonella typhi | 18 | 10 | 6 | 2 | 24 | 16 | 8 | 4 | 2 | 23 | 15 | 19 | 3 | 1 | 25 | |
| Pseudomonas aeruginosa | 16 | 11 | 6 | 3 | 20 | 19 | 13 | 9 | 3 | 23 | 18 | 13 | 7.0) | 2 | 22 | |
| Salmonella Choleraesuis | 13 | 9 | 6 | 4 | 20 | 14 | 9 | 7 | 6 | 19 | 12 | 10 | 8 | 5 | 20 | |
| Salmonella arizonae | 20 | 18.0) | 14 | 7 | 20 | 21 | 19 | 17 | 5 | 26 | 21 | 18 | 13 | 8 | 19 | |
| Proteus mirabilis | 20 | 19 | 15 | 6 | 17 | 22 | 19 | 16 | 8 | 19 | 19 | 18 | 12 | 8 | 22 | |
| Aeromonas hydrophilia | 19 | 12 | 10 | 4 | 22 | 15 | 9 | 5 | 3 | 19 | 16 | 17 | 12 | 9 | 20 | |
| Bacillus subtilis | 18 | 15 | 7 | 4 | 19 | 19 | 14 | 8 | 3 | 16 | 18 | 14 | 7 | 3 | 20 | |
| Salmonella typhi | 16 | 8 | 5 | 2 | 18 | 19 | 14 | 8 | 6 | 19 | 10 | 6 | 3 | 1 | 16 | |
| Shigella dysenteriae | 20 | 18 | 15 | 5 | 20 | 18 | 15 | 14 | 6 | 19 | 20 | 18 | 15 | 4 | 20 | |
| Burkholderia cepacia | 18 | 15 | 6 | 2 | 23 | 19 | 18 | 7 | 4 | 26 | 20 | 18 | 7 | 3 | 24 | |
| Citrobacter koseri | 23 | 20 | 18 | 9 | 24 | 20 | 10 | 4 | 25 | 20 | 15 | 19 | 6 | 2 | 24 | |
| Klebsiella ozaenae | 20 | 17 | 9 | 2 | 23 | 23 | 20 | 16.0) | 7 | 23 | 20 | 16 | 9 | 4 | 15 | |
Note: P value-<0.0001, P value summary**** Significantly different standard deviations -(P <0.05), MIC (30 mg/ml), MFC (15 mg/ml)
Table 4.Diameter of zones of inhibition of crude ethyl acetate extracts of Spondias mombin on the test fungi.
| Diameter of zone of growth inhibition (mm) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LEAF | ROOT | STEM BARK | ||||||||||||||
| Fungi | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole(5µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole(5µg) | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Fluconazole(5µg) | MIC: Minimum Inhibitory Concentratio-30mg/ml),MFC: Minimum Fungicidal Concentration -15mg/ml |
| Candida albican | 19 | 9 | 5 | 3 | 28 | 14 | 7 | 4 | 2 | 26. 0 | 11 | 5 | 3 | 0 | 25 | |
| Aspergillus niger | 19 | 17 | 10 | 5 | 23 | 18 | 15 | 8 | 5 | 21 | 20 | 18 | 15 | 9 | 22 | |
| Fusarium solani | 20 | 18 | 15 | 9 | 22 | 18 | 15 | 10 | 6 | 20 | 19 | 15 | 10 | 8 | 21 | |
| Saccharomyces cerevisiae | 17 | 10 | 5 | 1 | 18 | 19 | 17 | 12 | 8 | 20 | 18 | 15 | 9 | 5 | 19 | |
| Aspergillus flavus | 12 | 8 | 5 | 3 | 18 | 19 | 15 | 10 | 6 | 23 | 10 | 5 | 2 | 1 | 20 | |
| Phytophera megakarya | 8 | 5 | 2 | 0 | 18 | 3 | 2 | 0 | 0 | 20 | 10 | 0 | 0 | 0 | 17 | |
| Candida kruise | 18 | 13 | 8 | 4.0) | 20 | 18 | 13 | 10 | 7 | 20 | 19 | 15 | 9 | 6 | 22 | |
| Rhizopus stonifer | 9 | 6 | 4 | 1 | 12 | 7 | 4 | 3 | 0 | 12 | 10 | 7.0) | 5 | 1 | 10 | |
| Trichoderma horizionum | 10.0) | 7 | 5 | 2 | 12 | 18 | 15 | 10 | 8 | 20 | 19 | 10 | 3 | 1 | 21 | |
| Fusarium vortercelium | 17 | 12 | 9 | 5 | 21 | 21 | 16 | 10 | 4 | 22 | 20 | 15 | 9 | 3 | 21 | |
| Syncephalastrum racemosum | 19 | 10 | 6 | 2 | 21 | 17 | 15 | 10 | 4 | 30 | 19 | 16 | 10 | 4 | 23 | |
Note: P value-<0.0001, P value summary**** Significantly different standard deviations -(P < 0.05), MIC: Minimum Inhibitory Concentratio-30mg/ml, MFC: Minimum Fungicidal Concentration -15 mg/ml
Table 5.Diameter of zones of inhibition of crude ethanolic extracts of Spondias mombin on the test bacteria.
| Diameter of zone of growth inhibition (mm) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LEAF | ROOT | STEM BARK | ||||||||||||||
| Bacteria | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin 5 µg | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin 5 µg | 60 mg/ml | 30 mg/ml | 15 mg/ml | 7.5 mg/ml | Ofloxacin 5 µg | MIC (15mg/ml) , MBC (7.5mg/ml) |
| Mycobacterium fortuitum | 12 | 9 | 7 | 3 | 28 | 14 | 7 | 4 | 2 | 25 | 23 | 10 | 6 | 4 | 27 | |
| Mycobacterium smegmatis | 14 | 11 | 7 | 4 | 27 | 10 | 7 | 3 | 2 | 25 | 11 | 6 | 4 | 2 | 24 | |
| Mycobacterium abscessus | 13 | 6 | 4 | 2 | 27 | 10 | 4 | 2 | 0 | 32 | 17 | 5 | 3 | 4 | 32 | |
| Mycobacterium phlei | 14 | 6 | 2 | 1 | 24 | 14 | 6 | 3 | 1 | 25 | 10 | 6 | 4 | 2 | 29 | |
| Staphylococcous aureus | 15 | 10 | 6 | 4 | 23 | 15 | 10 | 7 | 3 | 25 | 14 | 10 | 5 | 2 | 29 | |
| Escherichia coli | 17 | 13 | 7 | 3 | 25 | 12 | 6 | 3 | 2 | 26 | 12 | 6 | 3 | 0 | 24 | |
| Klebseilla pneumoniae | 13 | 7 | 4 | 3 | 23 | 13 | 7 | 5 | 2 | 25 | 11 | 7 | 4 | 2 | 27 | |
| Salmonella typhi | 17 | 11 | 6 | 2 | 22 | 13 | 8 | 5 | 3 | 25 | 15 | 10 | 6 | 3 | 26 | |
| Pseudomonas aeruginosa | 19 | 12 | 7 | 4 | 21 | 14 | 10 | 6 | 3 | 20 | 17 | 11 | 7 | 2 | 23 | |
| Salmonella choleraesuis | 30 | 25 | 20 | 10 | 19 | 16.R | 8 | 5 | 3 | 20 | 17 | 12 | 9 | 6 | 20 | |
| Salmonella arizonae | 18 | 15 | 10 | 8 | 19.0) | 20 | 18 | 17 | 9.R | 25 | 20 | 17 | 12 | 6 | 18 | |
| Proteus mirabilis | 21 | 19 | 13 | 6 | 21 | 20 | 15 | 7.0) | 3 | 21 | 19 | 17 | 8 | 5 | 21 | |
| Aeromonas hydrophilia | 17 | 10 | 5 | 2 | 18 | 16 | 12 | 8 | 5 | 18 | 22 | 8 | 3 | 1 | 16 | |
| Bacillus subtilis | 18 | 15 | 9 | 4 | 20 | 16 | 12 | 7 | 4 | 18 | 12 | 8 | 3 | 2 | 15 | |
| Salmonella typhi | 16 | 10 | 8 | 3 | 19 | 17 | 12 | 7 | 4 | 18 | 15 | 9 | 5 | 2 | 18(I) | |
| Shigella dysenteriae | 20 | 16 | 10 | 5 | 20 | 21 | 19 | 15 | 5 | 21 | 18 | 15 | 9 | 4 | 19 | |
| Burkholderia cepacia | 21 | 18 | 7 | 3 | 24 | 19 | 11 | 6 | 2 | 23 | 15 | 12 | 10 | 7 | 18 | |
| Citrobacter koseri | 21 | 20 | 18 | 8 | 24 | 23 | 19 | 10 | 6 | 25 | 21 | 17 | 10 | 7 | 23 | |
| Klebsiella ozaenae | 23 | 19 | 15 | 10 | 25 | 23 | 19 | 15 | 10 | 23 | 21 | 18 | 15 | 10 | 23 | |
Note: P-value-<0.0001, P value summary**** Significantly different standard deviations (P 0.05), MIC (15 mg/ml), MBC (7.5 mg/ml)
Table 6.Diameter of zones of inhibition of crude ethanolic extracts of Spondias mombin on the test fungi.