Case Report - Archives of General Internal Medicine (2022) Volume 6, Issue 5
Erythromelalgia- An atypical manifestation of reactive thrombocytosis in Dengue fever.
Nandini Sanjeev Bandil1, Divit Shah1, Shubhi Gupta1*, Shubhangi Setia1, Sourya Acharya1, Samarth Shukla2
1Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, India
2Department of Pathology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, India
- *Corresponding Author:
- Shubhi Gupta
Department of Medicine
Jawaharlal Nehru Medical College
Datta Meghe Institute of Medical Sciences
Wardha
India
E-mail: guptashu01@hotmail.com
Received: 21-Apr-2022, Manuscript No. AAAGIM-22-61434; Editor assigned: 23-Apr-2022, PreQC No. AAAGIM-22-61434 (PQ); Reviewed: 07-May-2022, QC No. AAAGIM-22-61434; Revised: 09-May-2022, Manuscript No. AAAGIM-22-61434 (R); Published: 16-May-2022, DOI: 10.4066/ 2591-7951.100122
Citation: Bandil SN, Shah D, Gupta S, et al. Erythromelalgia- An atypical manifestation of reactive thrombocytosis in Dengue fever. Arch Gen Intern Med. 2022;6(5):122
Abstract
Dengue, also referred to as break bone fever or dandy fever is a febrile viral illness commonly found in tropical and sub-tropical climates worldwide, with a higher prevalence in urban and semi urban areas. Dermatologic manifestations of dengue infection can be erythema, morbilliform eruptions, and hemorrhagic lesions. Erythromelalgia is characterised by intense redness, burning pain and increased local temperature of the affected extremities that may occur episodically or continuously. Erythromelalgia may be primarily idiopathic or may be caused by underlying disorders like nerve damage due to injuries, autoimmune diseases like lupus vasculitis, multiple sclerosis and infection like viral fever. Reactive thrombocytosis (RT) refers to abnormally high platelet count in absence of chronic myeloproliferative disease occurring in response to any pre-existing inflammatory, infectious or hemorrhagic condition. The common infections that are associated with RT are skin/soft tissue, urinary tract infection, pneumonia followed by gastrointestinal infection. We present a case of an elderly male with dengue fever induced reactive thrombocytosis causing erythromelalgia.
Keywords
Dengue, Reactive thrombocytosis, Erythromelalgia.
Introduction
Current statistics of dengue states that the cases of dengue are on up rise with approximately 390 million cases per year, of which 96 million presents clinically. India reported 6837 cases till May 31, 2021 [1].
Dengue, an arthropod borne acute viral illness is a global health problem that causes an alarming impact on the human health as well as the nation’s economy. The causative agent of this viral presentation is an RNA virus of family Flaviviridae which spreads through a vector mosquito which may be Aedes aegypti, Aedes albopictus and Aedes polynesians, of which the primary and most important one is Aedes aegypti [2]. There is a significant rise in dengue cases during the monsoon months due to ambient temperature, humidity, improper and inadequate drainage of garbage and waste water, which serve as breeding grounds for the mosquitoes [3].
The virus includes four serotypes according to certain immunological and biological criteria that are, DEN1,2,3,4, of which—is most prevalent and DEN2 which presents with the most severe manifestations. It presents with a wide spectrum of symptoms, ranging from undifferentiated fever to classical dengue fever to life-threatening complications, such as dengue haemorrhagic fever and dengue shock syndrome. Commonly seen symptoms of dengue include acute onset high fever, muscle and joint pain classically referred to as break bone fever, myalgia, cutaneous rash, hemorrhagic episodes, and circulatory shock. Rare manifestations can be oral pathology and erythromelalgia (EM).
Erythromelalgia is a rare condition, characterised by intense burning pain, redness and localised increase in temperature in the extremities, which is typically bilateral, which can be presented with other dermatological features such as paraesthesia, livedo reticularis The reasons for this are still under research including gene mutations affecting the ion channels or changes in the small nerve fibres that affect the circulation in the small blood vessels causing significant redness in the extremities. Abnormal aggregation and consumption of platelets results in EM associated with thrombocythemia like essential thrombocytosis and reactive thrombocytosis [4].
Leukopenia and thrombocytopenia are the hallmarks of acute dengue which normalises with recovery but progression of dengue fever from thrombocytopenia to thrombocytosis is relatively uncommon. Reactive thrombocytosis refers to elevated platelet count (more than 450000 per mcl) that develops secondary to a coexisting inflammatory condition like infection or any chronic inflammatory [5]. It is generally a self-limiting condition resolving with the management of the causative condition. This thrombocytosis itself does not lead to complication like thrombosis or bleeding. Other studies were also done showing dengue fever that led to reactive thrombocytosis.
Case Report
A 60-year-old Indian female, labourer by occupation, presented to us with symptoms of headache, fever, myalgia and arthralgia for 4 days. There was no history of cough, expectoration, breathlessness, and seizures. There was no history of Covid-19 infection in the past and he had been vaccinated with two doses of AstraZeneca (covishield) vaccine.
On the day of admission, the body temperature was 38.5°C, pulse rate was 94 bpm regular, peripheral pulses were palpable, BP was 110/70 mmHg, respiratory rate 20/min and O2 Sat was 98%. There was no pallor, icterus and lymphadenopathy. Cardiovascular and respiratory system examination was within normal limits. On per abdomen examination no hepatomegaly, splenomegaly or abdominal tenderness was seen. There was no ascites. There were no abnormal neurological signs.
Investigations
Complete blood count was within normal limits. Absolute platelet count - were done to rule out dengue, scrub typhus, Leptospira, malaria, Widal test. The patient tested positive for dengue fever antigen NS1. IgM and IgG antibodies were negative. Torniquet test was done and found to be negative which ruled out any bleeding or thrombotic complication.
Laboratory investigations showed: Hb was 10 g/dL, WBC was 9.5 × 10^3 uL and platelet count was 45 × 10^3 per micro-L. C-reactive protein -8 mg/L, Ig M Dengue was positive. Parachek for malaria, Ig M scrub Typhus, Ig M Leptospira was negative. Chest radiograph, ECG, Echocardiogram, abdominal USG and arterial duplex of lower limbs were normal. The patient was started on empirical oral doxycycline and IV fluids and antipyretics.
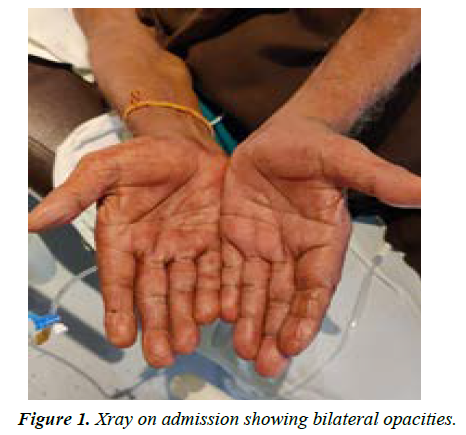
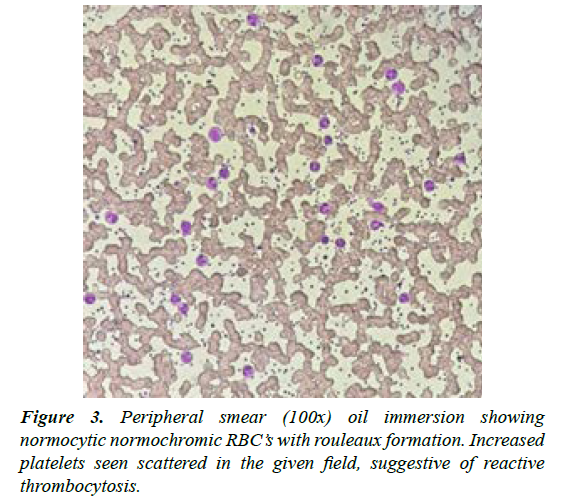
On day 3 of admission, the patient presented with new complaints that included intense redness and pain in palms and soles with increased local redness (Figures 1 and 2). Laboratory investigations were repeated on same-day. Though other laboratory parameters were normal, absolute platelet count was -1015 × 10^3 uL. Symptomatic Management was continued. Tab. Pregabalin 150 mg and tab. Fexofenadine 180 mg was initiated for EM. The platelets remained elevated above 500 × 10^3 uL, for 10 more days and then gradually declined and normalized to 450 × 10^3 uL by the 14th day. The patient was investigated for JAK 2 mutation but was found to be negative (Figure 3).
Discussion
The chronological pattern which was seen in this case was dengue followed by reactive thrombocytosis which w in turn caused erythromelalgia. The basic pathology involved in Dengue fever is thrombocytopenia, that decreases progressively from the third day onwards, the exact aetiology for which is still unknown. In dengue fever thrombocytopenia is seen that leads to increase level of an enzyme named Thrombopoietin (TPO). TPO regulates platelet production by acting on the TPO receptor leading to secondary thrombocytosis [6]. Serum levels of TPO are inversely related to circulating platelet count, thus due to thrombocytopenia in dengue, TPO production is increased. There is also release of pro-inflammatory cytokines such as IL-1, IL-6, IL-11, CRP and elevated ESR. These factors lead to increased megakaryocytopoiesis which consequently leads to secondary or reactive thrombocytosis. The platelets being acute phase reactant can increase due to stimuli like systemic infections inflammatory conditions and tumors including viral fever like dengue which is different from primary or essential thrombocythemia which is a myeloproliferative disorder due to a clonal expansion of bone marrow progenitor cells.
The term erythromelalgia is derived from Greek words: erythrose (red), Melos (limb) and algos (pain), which essentially form the triad of this condition [7]. The presentation shows a bilateral distribution in maximum cases, but it can also present unilaterally in secondary cases. It may be primary, which may be genetic or idiopathic, or secondary, which is caused as a result of infections, myeloproliferative disorders, medications etc. Other terms for this condition are burning feet syndrome, erythermalgia, Gerhardt disease, and Mitchell disease. The connection between erythromelalgia and thrombocytosis can be established from skin biopsy samples revealing excess aggregation of platelets, decreased platelet survival and some role of prostaglandins and cyclooxygenase.
The management of erythromelalgia includes avoidance of triggers, such as heat, physical activity and standing. For primary erythromelalgia, the mainstay is symptomatic treatment whereas secondary erythromelalgia can be resolved with the treatment of the causative factor. Drugs such as Lidocaine, carbamazepine and mexiletine have shown promise in the therapy of primary EM [8-14]. The drug of choice for secondary EM (associated with thrombocytopenia or myeloproliferative disorder) is aspirin. Pain rehabilitation programs and patient counselling can lead to a positive outcome.
Complications can include ulceration, blistering, cyanosis, gangrene and necrosis of the affected extremity. Quality of life is dramatically affected. Malnutrition and hypothermia can result. Hence regular follow up is advocated and annual blood work up is essential to prevent morbidity.
Conflict of Interest
None
References
- Bhatt S, Gething PW, Brady OJ, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504-7.
- Hasan S, Jamdar SF, Alalowi M, et al. Dengue virus: A global human threat: Review of literature. J Int Soc Prev Community Dent. 2016;6(1):1-6.
- Panda S, Bhargava B, Gupte MD. One World One Health: Widening horizons. Ind J Med Res. 2021;153(3):241.
- Schafer AI. Thrombocytosis and thrombocythemia. Blood Rev. 2001;15(4):159-66.
- Acharya S, Shukla S, Lahole S, et al. Thrombocytopenia to Reactive Thrombocytosis in Scrub Typhus- The Play of Platelets. J Clin Diagn Res. 2020; 14:01-02.
- Jha SK, Karna B, Goodman MB. Erythromelalgia. 2021
- Tham SW, Giles M. Current pain management strategies for patients with erythromelalgia: a critical review. J Pain Res. 2018;11:1689–98.
- Patil PS, Chandi DH, Damke S, et al. A Retrospective Study of Clinical and Laboratory Profile of Dengue Fever in Tertiary Care Hospital, Wardha, Maharashtra, India. J Pure Appl Microbiol. 2020;14(3):1935-39.
- Bhayani P, Acharya S, Shukla S. 'Boomerang sign'in dengue encephalitis. In J Medi Speciali. 2019 ;10(1):52.
- Patil A, Acharya S, ShuklA S. Opsoclonus-Myoclonus Syndrome (OMS) Due to Dengue Meningoencephalitis. J Clin Diagnostic Res. 2019;13(11).
- Steinmetz JD, Bourne RRA, Briant PS, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Global Health. 2021;9(2):E144–60.
- Franklin, Richard Charles, Amy E. Peden, et al. The Burden of Unintentional Drowning: Global, Regional and National Estimates of Mortality from the Global Burden of Disease 2017 Study. Injury Prev. 2017;26(1): 83–95.
- James SL, Castle CD, Dingels ZV, et al. Estimating global injuries morbidity and mortality: methods and data used in the Global Burden of Disease 2017 study. Injury Preve. 2020;26(2):125-53.
- James SL, Castle CD, Dingels ZV, et al. Global injury morbidity and mortality from 1990 to 2017: results from the Global Burden of Disease Study 2017.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref