Review Article - Biomedical Research (2017) Volume 28, Issue 18
Emotional alterations in idiopathic Parkinson's disease without dementia
Hurtado-Gonzalez CA1,2*, Ladera V3, Perea MV3, Garcia R3 and De la Cruz-Cifuentes O2
1Faculty of Psychology, Cooperative University of Colombia, Cali Branch Campus, Colombia
2Faculty of Medicine, Libre University, Cali Branch Campus, Colombia
3Department of Basic Psychology, Psychobiology and Behavioral Sciences Methodology, University of Salamanca, Spain
- *Corresponding Author:
- Hurtado-Gonzlez CA
Faculty of Psychology
Cooperative University of Colombia
Cali Branch Campus, Colombia
E-mail: carlos.hurtadog@campusucc.edu.co
Accepted date: August 28, 2017
Abstract
Currently Parkinson’s disease (PD) is no longer considered a disease exclusively motor type, now PD is characterized as cognitive neurobehavioral pathology often results in patients emotional disturbances that degrade their quality of life. This article intended to show an updated review of the affective disorders/emotional as depression, anxiety and apathy significantly affecting physical function, psychological, individual and family of sufferers of PD. It was found that the prefrontal cortex, hippocampus, anterior cingulate cortex, limbic system and thalamic nuclei are related to depression, such as frequent psychopathological disorder in PD, also dysfunctions in the putamen, dopamine and norepinephrine are associated with emotional disturbances that characterize to anxiety or psychosocial stress states. Next, the deregulation of fronto circuits-subcortical and frontal lobe dysfunction with loss of connections to the basal ganglia, lead to generate in subjects with PD a state of discouragement to many tasks (Apathy). The results suggest that the implementation of new lines of research and intervention to detect emotional disorders in PD, with the aim of generating strategies to help improve the quality of life in patients diagnosed with PD.
Keywords
Anxiety, Apathy, Depression, Emotional disorders, Parkinson's disease
Introduction
Parkinson's disease (PD) is one of the most prevalent neurodegenerative diseases (1% of the population over 60 y) and with great impact on activities of daily living and quality of life of patients [1]. It is the second most common neurodegenerative disease after Alzheimer's disease.
The PD is considered a multifactorial process which is characterized by the presence of non-motor symptoms (sensory, autonomic, sleep disorders, behavioral and cognitive impairments, among others) that accompany the cardinality motricity characteristic to disease; and diffuse deposit of alphasynuclein (component of Lewy bodies), causes dysfunction of different neurotransmission systems such as norepinephrine, serotonin and acetylcholine, also generating neuronal death in different cortical structures, subcortical and brainstem [2].
Patients suffering from this disease tend to have feelings of sadness (depression) are regularly accompanied by stress levels (anxiety) distortive their psychological, emotional and individual balance [3] likewise, some patients (but less frequently) exhibit behaviors that are characterized by demotivational aspects (apathy) that eventually locate these people diagnosed with PD, in a state of lack of interest in various tasks [4].
Emotional disturbances such as depression, anxiety and apathy are the subject of study, not only for their appearance in the early stages of the disease, but also for other causes such as their relationship with quality of life, low self-esteem, stress states psychosocial and selflessness presented by patients in activities of daily life [5].
This article aims to analyse emotional alterations such as depression, anxiety and apathy that may be present in idiopathic PD without dementia, as well as the brain areas involved.
Method
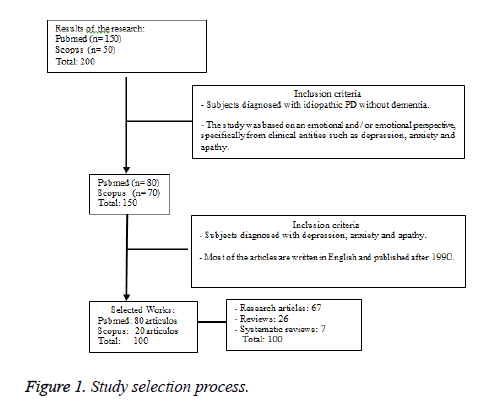
For the preparation of this review are used 100 primary references, 67 research articles conducted to study emotional disturbances in PD, 26 review articles and 7 systematic reviews. The search for the information was made in PubMed bases and Scopus data. The initial search is performed using the keywords (emotional disturbances, anxiety, depression, apathy, PD), obtaining a total of 200 references. Summaries of these studies were analysed and selected 150. Then continue is selected these works meeting the criteria outlined in Figure 1, obtaining a total of 10 0 (Figure 1).
Results
Depression in Parkinson's disease
Depressive symptoms usually present in many patients with PD, are characterized by continuous sadness, hopelessness, feelings of guilt, permanent tiredness, bodily discomfort and inability to make decisions; its prevalence and incidence is high [6,7], at any stage of the disease [8,9] There is a high correlation between depression, quality life, disability and cognitive impairment [10].
The depression in PD has a prevalence ranging between 50% [11] and 30-40% [12] and it is considered one of the major predictors of deterioration in quality of life and functional impairment of motor cardinality [13,14]. Some studies [15-17] have reported a prevalence of major depression 20-25%; clinical manifestations of mild depression are more common in patients with this pathology, presenting a prevalence of 50%. [18]. A systematic review show a 17% prevalence for major depression, 22% for minor depression and 13% for dysthymia. According to these authors, depressive symptoms presented subjects is significant, regardless of the clinical criteria of [19].
To diagnose depression in PD, it is necessary to be supported by the coexistence of three components to assess and identify depressive symptoms as a mood disorder: 1. Negative affection, 2. Mood and 3. Somatic concerns [20]. The criteria for diagnosing a depressive episode according to the diagnostic and statistical manual of mental disorders, [19] should include: 1. Depressed mood most of the day, 2. Decreased interest or ability to experience pleasure in all or almost all of the day 's activities, 3. Significant weight loss without 4. Insomnia or hypersomnia all day 5. Psychomotor agitation or slowing almost every day 6. Fatigue or loss of energy 7. Feelings of worthlessness or guilt 8. Decreased ability to think or concentrate, 9. Recurrent thoughts of death or recurrent suicidal ideation.
Currently the clinical criteria to diagnose and identify depression based DSM-IV are essential, however, this classification is not specific to PD subjects. For Voss and Hegeman [21] is necessary to consider what criteria of DSMIV can be applied to this population, i.e., what clinical characteristics presented in the DSM-IV adjust to the depressive symptoms presented subjects with PD. Assessment and diagnosis of depression should be accompanied by clinical judgment of several specialists, in order to determine or rule out other conditions that may be predisposing factors or inducers of depression [21].
Emotional disturbance such as anxiety and apathy are common in PD used almente have a superposition with depressive symptoms, especially apathy, which can occur in the absence of clinical depression [22]. Despite this overlap, and although depressive symptoms and apathy share symptoms such as decreased of the interest, fatigue and anhedonia, it is important to note that the mood in apathy is objective in nature, unlike depression mood is subjective, negative and associated with despair, anxiety and low self-esteem.
A variety of scales used to assess depression in the general population and have been used in patients with PD, although it is unclear which of these scales are the most appropriate for this population [23]. These include: The Hamilton Depression Scale (HDRS) [24], the Beck Depression Inventory [25], the Depression Scale Geriatric [26] Depression Scale Zung [27] Scale Hospital Anxiety and Depression [28] The Montgomery- Asberg Depression Rating Scale [29]. It would be advisable to carry out investigations that analyse the validity, reliability, sensitivity and specificity of these scales for this population.
The etiology of depression in PD is not clear [21]. Noted that results of the clinical situation [30], the reduction transporter noradrenalin and dopamine mesolimbic and striatal, [7,31-34] typically generates a state of reduced motivation found associated with decreased dopaminergic activity in the nucleus accumbens, ventral striatum, prefrontal cortex, serotonin levels [35] and the effect of various brain regions [7,35,36].
Cardoso et al. [36] indicate that depressive symptoms are related to dysfunctions in the medial prefrontal cortex and the dorso-medial thalamus, which are involved with the organization of emotional, motivational and alert responses. Studies with neuroimaging techniques [7,37-40] indicate alterations lateral orbitofrontal cortex level, hippocampus, anterior cingulate cortex, prefrontal cortex, inferior frontal lobe reduction in basal ganglia, thalamic striatal circuits, subcortical nuclei, cortex Limbic, brain-related areas of mood.
Depression not only affects the quality of life for patients, family, friends and immediate caregivers are also affected, social and family structure [41,42], generating a negative impact [41,43,44] which interferes with activities of daily living and in aspects such as communication, stigma and social support that are accompanied by irritability, restlessness and feelings of emptiness.
The presence of depressive symptoms can also affect the patient’s cognitive status. For example, low yields in naming tasks, memory, verbal fluency, visuospatial functioning, learning, planning and flexibility are related depressive symptoms [8,12,45,46]. Attentional deficits and executive are related to disruption of neural circuits that communicate the caudate and PFC (secondary to loss of dopaminergic projections nigrostriatal) and the direct loss of dopaminergic projections tegmental ventral brainstem to cortical areas [47], deficits may be related to mood disorders like depression. Depression is also being seen as a possible predictive factor in predicting cognitive impairment in early stages of the disease [48].
Tremblay, Achim, Macoir and Monetta [49] suggest that it is necessary to develop new research to understand more precisely the possible relationship between cognitive deficits and depression in PD, with the aim of generating plans neurorehabilitation not only guided at correcting the motor dysfunction of the subjects, but also to improve social, family and individual aspects.
Table 1 presents the main findings related to PD and depression.
| Authors | Participants | Main results |
|---|---|---|
| Bewernick and Schlaepfer [50] | Review study | Depression is associated with cell loss in the prefrontal cortex, paraventricular nucleus of the hypothalamus and reduction of the hippocampus. |
| Skidmore et al. [51] | 22 patients with idiopathic PD without dementia. | Depression, apathy, and increased motor symptoms are associated with distinct activity profiles in PD. |
| Xuyun and Wu [52] | 33 patients with idiopathic PD with dementia and with depression, compared with a group with PD without depression. | Patients with PD have abnormal levels of neural activity in various areas of the brain associated with the limbic prefrontal network. |
| Yamanishi et al. [9] | 117 patients with idiopathic PD | Depression and anxiety are common alterations in PD, are associated with quality of life, regardless of the severity of the motor stage. |
| Even and Weintraub [6] | Systematic review. | More research is needed, with different techniques (cluster analysis, latent analyses, clinical correlates, biomarkers, etc.) to delimit the subtypes of depression in PD. |
| Cardoso et al. [36] | 36 male patients with idiopathic PE. 20 of them were diagnosed with major depression. | Depression in patients with PD is associated with a decrease in the activity of the dorsomedial nucleus of the thalamus and the prefrontal cortex of the medial dorsum. |
| Costa et al. [8] | 83 patients with idiopathic PE without dementia | Depression in PD is associated with alteration of the prefrontal cortical and limbic areas. |
| Remy et al. [7] | 20 patients with idiopathic PE without dementia. | Depression is associated with a specific loss of dopamine and norepinephrine innervation of the cortical and subcortical components of the limbic system. |
Table 1. Summary of principal and studios on depression in Parkinson's disease.
Anxiety in Parkinson's disease
Anxiety in PD is a common emotional disorder characterized by symptoms such as feelings of fear, uneasiness, worry, sweating, tremors, dizziness, tachycardia, muscle tension, among others; it has a prevalence of 36% to 40% [53-55]. Walsh and Bennet show that states of psychosocial stress (anxiety), as well as depression, are associated with psychological events that are distressing for the subject, which tend to be related to the emotional situation generated by PD.
Other studies [56-58] indicate that anxiety related to depression and impairment of quality of life. It has been associated with l motor cardinality having each patient (tremor, bradykinesia, rigidity, and postural instability), gait disorders (festination, freezing, dyskinesia’s, motor fluctuations) and oscillations in periods on-off [58-60]. There are several theories to explain anxiety and emotional disturbance in PD, but little known, anxiety is attributed to a set of medical, biological and psychosocial factors that attempt to explain in detail this syndrome, however, what is known today is that anxiety is a secondary response or reaction to the diagnosis of the disease [61].
DSM IV [19] presents a number of criteria to diagnose an anxiety disorder, but these are not specific for PD still can be applied informally in the clinical setting by a trained and qualified person to do [62]. The diagnosis of anxiety in PD remains ambiguous, because there is overlap of anxiety with various mental and physical symptoms that are associated with PD, symptoms that characterize anxiety are often attributed to depressive symptomatology and pictures mixed clinicians fail classified in the DSM IV [19,61].
The different diagnostic categories such as generalized anxiety disorder, panic disorder, obsessive-compulsive disorder and depression makes it difficult to establish an objective diagnosis of anxiety in PD [62]. In order to perform an objective analysis of anxiety in PD, it is necessary to carry out a detailed analysis of the patient's history, also based on the information that the main caregiver can provide, in order to know the patient's behavior in the different contexts in which develops [61].
Chen and Marsh [61]; Shulman et al. [63] Point out the need for a periodic evaluation of patients with PE in order to detect, evaluate and intervene in PE. At present there are no specific scales that measure anxiety property in PD, for Leentjens et al. [64], these scales tends to focus on the symptoms of panic disorder, but not in the clinical picture of anxiety presenting subjects with a diagnosis of PD.
The scales have been validated or used in PD patients, are the Beck Anxiety Inventory (BAI) [65], Anxiety Inventory-State Spielberg [66] and Anxiety and Depression scale (HADS) [28].
Etiologically related anxiety is a psychological response to the motor and physical symptoms experienced by patients with PD, found that dysregulation in chemical factors such as norepinephrine, serotonin, dopamine and γ-amino acid or butyric acid (GABA) they are involved in the pathogenesis of anxiety [55]. Dopamine deficiency may be due to the interactions that occur between dopaminergic deficits and the variability (deficits) occurring in norepinephrine and serotonin occurring in subjects with PE [55,67,68], generating neuronal loss in the tegmental area ventral and locus ceruleus.
Anxiety can also be caused by alterations in serotonin transporter, there appears a functional polymorphism and genetic defect which can play a role in the pathology of anxiety in PD [55,69] and dysfunctions to brain areas such as the anterior putamen, [7,43,70,71], the limbic cortex, basal ganglia and amygdala as areas instinctive regulation emotional are altered by dysfunction or deficiency presenting dopamine to the amygdala [32,72].
Leentjens et al. [60] indicate that anxiety is one of the emotional disturbances little studied, the authors see the need for research to measure, prevent and intervene the negative impact that anxiety has on the quality of life in patients with PD [73]. What is clear so far is that anxiety is associated with depressive disorders, and both disease entities, impact to impair the physical, psychological, social and family stability of these patients [71,74].
Anxiety also tends to be associated with motor fluctuations PD, although these studies are not robust, [71] indicate that it is an association that possibly is related to cardinal signs like the march, the dysfunction of the same and the postural instability [60].
Regarding cognitive functioning, some studies have found no relationship [75,76]. In contrast, Foster et al. [77] indicate that anxiety affects operative memory in patients who are in the early stages of their disease, particularly in the onset of left hemibody disease. Despite these results, currently the relationship between anxiety and cognitive functioning is still unknown and needs further investigation of experimental type [12].
Authors as Thanvi et al. [76] are clear in stating that anxiety sufferers third of patients so far have not found a possible link between cognitive functioning and the clinical symptoms of psychosocial stress (anxiety). Research on this psychopathology in PD is still very incipient, it is hoped that in the medium term the new lines of research will be focused on aspects of neurorehabilitation.
Table 2 shows a series of studies on anxiety in PD.
| Authors | Participants | Main results |
|---|---|---|
| Yamanishi et al. [9] | 117 patients with idiopathic PE without dementia. | Anxiety is an important clinical condition that is associated with quality of life in patients with PD. |
| Gallagher and Schrag [43] | Review article. | Anxiety is highly correlated with PD and occurs in the context of motor and non-motor fluctuations. |
| Hanna and Cronin [73] | 38 participants with PE without dementia 20 males - 18 females. | The impact of anxiety is related to quality of life. |
| Leentjens et al. [60] | 342 patients with idiopathic PE without dementia. Cross-sectional international study. | Anxiety is poorly studied in PD, research is hampered by the questionable validity of DMS IV and the anxiety disorders defined in PD. |
| Prediger et al. [71] | Critical review study. | Anxiety impairs the quality of life of patients with PD, more robust investigations are needed to alleviate this pathology in subjects with PD. |
| Dissanayaka et al. [53] | 79 patients with idiopathic PE without dementia. | Anxiety increases the complexity of PE. |
| Quelhas and Costa [3] | 43 patients with idiopathic PE without dementia. | Anxiety is the strongest predictor of quality of life in patients with PD. |
| Carod et al. [78] | 132 patients with idiopathic PE without dementia. | Anxiety affects the quality of life of patients with PD. |
Table 2. Summary of principal and studios on anxiety in Parkinson disease.
Apathy in Parkinson's disease
Apathy is characterized by the loss of interest or persistent emotional liability, p resenting n subjects with PD to the variety of tasks, and aims motivation to carry out [4,79,80].
Apathy is another neurobehavioral syndrome emotional coexisting with the EP, a symptom not motor has a prevalence ranging between 25% and 45% [81] 16% and 48% [82] or from 17% to 70% [83] that same depression and anxiety succeed in diminishing the quality of life of patients suffering from Parkinson's, this deterioration is represented and associated by cognitive deficits, [42] which are characterized by dysfunction of the frontal lobe, temporal, basal ganglia, cerebellar areas, dysfunction of the dopaminergic system and disconnections of the fronto-subcortical that affects planning, organization and mental flexibility (executive functions) [80,84,85].
At present, diagnosis of apathy is a challenge for clinicians, because it is associated with depressive symptoms, cognitive deficits and overlap occurring in the diagnostic criteria [74]. Leentjens [86] show no clinical diagnostic criteria for apathy today. The only criteria available are made by Marin [79]. Starkstein and Leentjens [86] propose a set of criteria that have been retrofitted under Marin diagnostic criteria [79]:
a. The lack of motivation in relation to the patient's previous level of functioning, or the standards of his age and culture, indicated by the subject or observed by others.
b. Presence of at least 4 w during most of the day, at least 1 symptom belonging to each of the following three domains:
Goal directed behavior decreased.
- Dependence of others to carry out daily activities.
- Lack of effort or energy to perform daily activities.
Decreased goal-directed cognition
- Lack of interest in learning new things or new experiences.
- The lack of concern for their personal problems.
Decreased behavior towards a goal
- Flat or unchanging affect
- Lack of emotional responsiveness to positive or negative events.
c. Symptoms cause clinically significant discomfort or impairment in social, work, or other important areas of functioning.
d. Symptoms are not due to decreased level of consciousness or the direct physiological effects of a substance.
Starkstein [4] points out that clinical nosology of apathy require further conceptual and empirical study.
Apathy, having a clinical point depression compared to [87,88], It makes evaluation is made more rigorous, systematic and objective tests that measure this are neurobehavioral syndrome so that does not go unnoticed by the centralization with research in the motor aspects of the disease.
The association between apathy and coexisting depression is caused because both syndromes cohabit in PE [51]. These aspects lead to reaffirm the need to investigate and classify the motor and non-motor disorders of this psychopathology, so that the latter (non-motor dysfunctions) do not go unnoticed by clinical reference.
Garcia et al. [82] indicate that apathy has begun to define itself as an emotional disorder that is caused by social, external and situations; for the authors the apathy syndrome is categorized into cognitive, emotional and behavioral aspects that make it appear as a one-dimensional psychopathological disorder.
That confused association between depression and apathy [4,82] is leading to new research lines focus on investigating apathy as neurobehavioral and differential depression syndrome, it is necessary that studies with more representative samples are made, this will, as far as possible, allow the detection of significant differences between the two clinical syndromes.
Regardless of the relation that apathy presents with depression, it is necessary to emphasize that this syndrome manages to deteriorate the quality of life in people with PD. The most commonly used scales to assess apathy are the scale of apathy Marin [79], the scale of assessment of apathy Lille [89], its adaptation to Castilian by Garcia [90] and the neuropsychiatric inventory in paragraph apathy [91].
Regarding cognitive functioning, some studies have found that apathy is associated with deficits experienced by patients in executive functions and activities of daily living [92-94].
Pluck and Brown, [95] indicate that apathy is associated with deficits in memory, language and executive functions which are also related by the loss of initiative, emotion and self - awareness before performing different tasks [96].
Louis et al. [97], apathy must be operated differently, in order to lay the groundwork for differentiating apathy and emotional syndrome, apathy related cognitive deficits, and especially, apathy differentiated and independent of depression. The theoretical position of these authors is what you should expect more detailed and thorough investigations [83,98].
The high prevalence filing the apathy is expected to be taken as an independent emotional syndrome that need not be related to other neuropsychiatric disorders, especially of emotional.
What is important in this relationship between depression and apathy is that subjects diagnosed with PD can improve their quality of life with activities that have the value of themselves, but also the motivation to be able to do a diversity of tasks, excluding Apathy as an emotional condition.
Table 3 presents the summary of the main studies on apathy in PD.
| Authors | Participants | Main results |
|---|---|---|
| McNamara et al. [92] | 30 patients with idiopathic PE without dementia. | Apathy is a frequent alteration in PD, with a higher risk of dementia. |
| Louis et al. [97] | 39 patients with PD without dementia, compared with 79 patients with essential tremor and 20 patients with dystonia. | Apathy can occur independently of depressive symptoms. |
| Laatu et al. [93] | 73 patients with idiopathic PE without dementia. | Apathy is significantly associated with ADL in PE |
| Robert et al. [85] | 45 patients with idiopathic PE without dementia and without depression. | The frontal, temporal and cerebellar areas are related to apathy in PD. |
| Leonet al. [94] | 557 patients with idiopathic PE without dementia. | Apathy is a clinical determinant that is related to quality of life. |
| Isella et al. [84] | 30 patients with idiopathic PE without dementia. | Apathy is frequent in PD, it is related to subcortical fronto dysfunction. |
| Pluck and Brown [95] | 45 patients with idiopathic PE without dementia compared to 17 patients with osteoarthritis | Apathy is associated with cognitive impairment in PD patients. |
Table 3. Presents the summary of the main studies on apathy in the PD.
Discussion and Conclusions
PD has ceased to be considered motor-exclusive pathology; the latest research has begun to categorize it as a cognitive neurobehavioral disease that coexists with emotional dysfunctions such as depression, anxiety and apathy that in the short, medium and long term end up deteriorating the quality of life of the people who suffer it.
The data obtained indicate that the subjects who are diagnosed with PD will present a disability in the subjectivity of their behavior and behavior, subjectivity that is marked by depression as a psychopathological disorder that impairs the personality of each of the subjects, especially related to cerebral aging, but at the same time associated with the deterioration (physical and cognitive) generated by PD [50,78].
This leads to the conclusion that depression as a frequent emotional disturbance may be a predictive factor in PD, an inference that can be verified by the non-motor dysfunctions that subjects with PD are presenting long before receiving the diagnosis; Depression as an emotional alteration means that mobility, activities of daily living, stigma and social support are impaired and at the same time related to a state of psychosocial stress or anxiety that does not allow subjects to envisage coping strategies that can restore their psychological balance [99].
Anxiety and depression as non-motor alterations of PD need to be studied in a systemic, detailed, experimental and deep way, in order to begin to create intervention plans that aim to minimize the negative impact that the disease has on the different Physical, social, family and individual dimensions of the subject.
Likewise, the lines of intervention should also focus on the treatment of apathy as a syndrome that causes subjects to lose interest and motivation of their daily tasks and habits, apathy in PD should be treated in a systemic manner [100] with pharmacological and non-pharmacological treatment. In this case, psychotherapy is presented as a clinical-psychological strategy that, if possible, will reduce the impact that motivation has on subjects with PD.
It is necessary that new investigations not only focus on the motor aspects of the disease, non-pharmacological treatments should be investigated and structured with a single purpose, mental health, individual and family of the subjects, since the deterioration of health Mental quality means that the quality of life is destabilized in all the psychosocial dimensions in which the subject develops; to this end, the following suggestions are provided to allow future research to centralize the emotional alterations in PD (Depression, anxiety and apathy):
1. Research on PD should operationalize its object of study in the emotional alterations, in order not to go unnoticed by the initial clinical evaluation of health professionals, especially in neurologists.
2. The previous point entails establishing a network or teamwork, where the neuropsychologist plays a relevant role in detecting the emotional dysfunctions that individual with PD present, and as these non-motor dysfunctions have an impact on cognitive, social and family functioning of subjects.
3. Detailed and systemic neuropsychological evaluation, will allow the generation of functional neurorehabilitation plans, which the neuropsychologist will emphasize in the improvement of the quality of life of the subjects and their insertion in the family and society.
4. Each of the topics of evaluation and intervention will allow taking the family as a resilient referent for the improvement of the subject, and where possible preventing a Burnout syndrome in their immediate caregivers.
5. To do this, it is necessary to take as a reference and meeting point the associations or houses of mutual help that tend to each of the previous points.
This, insofar as possible, will allow the social and family insertion of individuals with PD to result in a "stable" quality of life in each of the individual, physical, social and psychological dynamics in which the subject develops, hoping that the outcome of each intervention program may reduce the non-motor symptoms of the disease and that, if possible, delay the cognitive impairment of people with PD.
References
- Samii A, Nutt JG, Ransom BR. Parkinsons disease. Lancet 2004; 363: 1783-1793.
- Rey A. Parkinson's disease and other Parkinsonisms. Case-by-case neurology. Madrid Medica Panamericana 2009.
- Quelhas R, Costa M. Anxiety, depression, and quality of life in Parkinsons disease. J Neuropsych Clin Neurosci 2009; 21: 413-419.
- Starkstein S.E. Apathy in Parkinson’s disease: diagnostic and etiological dilemmas. Mov Disord 2012; 27: 174-178.
- Bonnet AM, Czernecki V. Non-motor symptoms in Parkinson’s disease: cognition and behavior. Geriatr Neuropsych Psychol Aging 2013; 11: 295-304.
- Even CY, Weintraub D. Is depression in Parkinson’s Disease (PD) a specific entity. J Affect Disord 2012; 139: 103-112.
- Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson’s disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005; 128: 1314-1322.
- Costa A, Peppe A, Carlesimo AP, Calta GC. Major and minor depression in parkinson’s disease: a neuropsychological investigation. Eur J Neurol 2006; 13: 972- 980.
- Yamanishi T, Tachibana H, Oguru M, Matsui K, Toda K, Okuda B, Oka N. Anxiety and Depression in Patients with Parkinson’s Disease. Int Med 2013; 52: 539-545.
- Bonnet AM, Jutras MF, Czernecki V, Corvol JC, Vidailhet M. Non motor symptoms in parkinson’s disease in 2012: relevant clinical aspects. Parkinson Dis 2012; 1-15.
- Zesiewicz TA, Hauser RA. Depression in Parkinson’s disease. Curr Psych Rep 2002; 4: 69-73.
- Polletti M, De Rosa A, Bonuccelli U. Affective symptoms and cognitive functions in Parkinson’s disease. J Neurol Sci 2012; 317: 97-102.
- Troeung L, Egan SJ, Gasson N. A meta-analysis of randomised placebo-controlled treatment trials for depression and anxiety in Parkinsons disease. PLoS ONE 2013; 8: e79510.
- Wishart S, Macphee GJ. Evaluation and management of the non-motor features of Parkinsons disease. Ther Adv Chronic Dis 2011; 2: 69-85.
- Cole SA, Woodard JL, Juncos JL, Kogos JL, Youngstrom EA, Watts RL. Depression and disability in Parkinsons disease. J Neuropsych Clin Neurosci 1995; 8: 20-25.
- Dooneief G, Mirabello E, Bell K, Marder K, Stern Y, Mayeux R. An estimate of the incidence of depression in idiopathic Parkinsons disease. Arch Neurol 1992; 49: 305-307.
- Seiler S, Perleth B, Gasser T, Ulm G, Oertel WH, Ellgring H. Partnership and depression in Parkinson’s disease. Behav Neurol 1992; 5: 75-81.
- Reijnders JS, Ehrt U, Weber WE, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinsons disease. Mov Disord 2008; 23: 183-189.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th Ed.). Washington, DC: American Psychiatric Association 1994.
- Zahodne LB, Marsiske M, Okun MS, Bowers D. Components of depression in parkinson disease. J Geriatr Psych Neurol 2012; 25: 131-137.
- Voss T, Hegeman RI. Depression in Parkinsons disease. Parkinsons disease non-motor non-dopaminergic features Jhon Wiley y Sons 2011; 183-192.
- Kirsch-Darrow L, Fernandez HF, Marsiske M, Okun MS, Bowers D. Dissociating apathy and depression in Parkinson disease. Neurology 2006; 67: 33-38.
- Schrag A, Barone P, Brown RG, Leentjens AF, McDonald WM, Starkstein S, Goetz CG. Depression rating scales in Parkinsons disease: critique and recommendations. Mov Disord 2007; 22: 1077-1092.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psych 1960; 23: 56-62.
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psych 1961; 4: 561-571.
- Yesavage JA, Brink TL. Development and validation for a geriatric depression screening scale. a preliminary report. J Psych Res 1983; 17: 37-49.
- Zung WW. A self-report depression scale. Arc Gen Psych 1965; 12: 63-70.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983; 67: 361-370.
- Montgomery SA, Asberg MARIE. A new depression scale designed to be sensitive to change. Br J Psych 1979; 134: 382-389.
- Caap AM, Dehlin O. Sense of coherence is a sensitive measure for changes in subjects with Parkinsons disease during 1 year. Scand J Caring Sci 2004; 18: 154-159.
- Camardese G, Di Giuda D, Di Nicola M, Cocciolillo F, Giordano AJ Guglielmo R. Imaging studies on dopamine transporter and depression: A review of literature and suggestions for future research. J Psych Res 2014; 51: 7-18.
- Klimek V, Scheck JE, Han H, Stockmmeir CA, Ordway GA. Dopaminergic abnormalities in amygdaloid nuclei in major depression: a postmortem study. Biol Psych 2002; 52: 740-748.
- Meyer JH, Kruger S, Wilson AA, Christensen BK, Goulding VS, Schaffer A, Kennedy SM. Lower dopamine transporter binding potential instriatum during depression. Neuro Rep 2001; 12: 4121-4125.
- Neumeister A, Willeit M, Praschakrieder N, Asenbaum S, Stastny J, Hilger E, Kasper S. Dopamine transporter availability in symptomatic depressed patients with seasonal affective disorder and healthy controls. Psychol Med 2001; 31: 1467-1473.
- Frisina PG, Haroutunian V, Libow LS. The neuropathological basis for depression in Parkinson’s disease. Parkinsonism Relat Disord 2009; 15: 144-148.
- Cardoso EF, Martins F, Fregni F, Myczkowski ML, Melo LM, Sato JR, Amaro E. Depression in Parkinson’s disease: convergence from voxel. Based morphometry and functional magnetic resonance imaging in the limbic thalamus. Neuroimage 2009; 47: 467-472.
- Feldmann A, Illes Z, Kostolany P, Illes E, Andrea MA, Kover F, Nagy F. Morphometric changes of gray matter in Parkinson’s disease with depression: a voxel-based Morfhometry study. Mov Disord 2008; 23: 42-46.
- Nilsson FM, Kessing LV, Sorensen TM, Andersen PK, Bolwig TG. Major depressive in Parkinson’s disease: A register-based study. Acta Psychiatrica Scandinavica 2002; 106: 202-211.
- Nilsson FM, Kessing LV, Bolwig TG. Increased risk of developing Parkinson’s disease for patients major affective disorder: A register study. Acta Psychiatrica Scandinavica 2001; 104: 380-386.
- Weintraub D, Burn DJ. Parkinsons disease: the Quitessential neuropsychiatric disorder. Mov Disord 2011; 26: 1022-1031.
- Arabia G, Grossardt BR, Geda YE, Carlin JM, Bower JH, Ahlskog JE, Rocca WA. Increased risk of depressive and anxiety disorders in relatives of patients with Parkinson’s disease. Arc Gen Psych 2007; 64: 1385-1392.
- Blonder LX, Slevin JT. Emotional dysfunction in Parkinson’s disease. Behav Neurol 2011; 1: 201-217.
- Gallagher DA, Schrag A. Psychosis, apathy, depression and anxiety in Parkinson’s disease. Neurobiol Dis 2012; 46: 581-589.
- McDonald WM, Richard IH, De Long R. Prevalence, etiology and treatment of depression in Parkinson’s disease. Soc Biol Psych 2003; 54: 363-375.
- Norman S, Troster A, Fields JA, Brooks R. Effects of depression and Parkinson’s disease on cognitive functioning. J Neuropsych Clin Neurosci 2002; 14: 31-36.
- Santangelo G, Vitale C, Trojano L, Cozzolino A, Grossi D, Barone P. Relationship between depression and cognitive dysfunctions in Parkinson’s disease without dementia. J Neurol 2009; 256: 632-638.
- Carbon M, Marie RM. Functional imaging of cognition in Parkinsons disease. Curr Opin Neurol 2003; 16: 475-480.
- Stefanova E, Potrebic A, Ziropadja L, Maric J, Ribaric I, Kostic V. Depression predicts the pattern of cognitive impairment in early Parkinson’s disease. J Neurol Sci 2006; 248: 131-137.
- Tremblay C, Achim AM, Macoir J, Monetta L. The hetrogeneity of cognitive symptoms in parkinson´s disease: a meta-analysis. J Neurol Neurosurg Psych Pract Neurol 2013.
- Bewernick BH, Schlaepfer TE. Chronic depression as a model disease for cerebral aging. Dialogues Clin Neurosci 2013; 15: 77-85.
- Skidmore FM, Yang M, Baxter L, von Deneen K, Collingwood J. Apathy, depression, and motor symptoms have distinct and separable resting activity patterns in idiopathic Parkinson disease. Neuroimage 2013; 81: 484-495.
- Xuyun W, Xia W, Liu J, Li, K, Yao, L. Abnormal baseline brain activity in non. depressed Parkinsons disease and depressed Parkinson’s disease: a resting-state functional magnetic resonance imaging study. Plos One 2013; 8: 63691.
- Dissanayaka N, Sellbach A, Matheson S, Sullivan JD, Silburn PA, Byrne GJ, Mellick GD. Anxiety disorders in Parkinson’s disease: prevalence and risk factors. Mov Disord 2010; 25: 838-845.
- Pontone GM, Williams JR, Anderson K, Chase G, Goldstein S, Grill S, Marsh L. Prevalence of anxiety disorders and anxiety subtypes in patients with Parkinson’s disease. Mov Disord 2009; 24: 1333-1338.
- Walsh K, Bennett G. Parkinsons disease and anxiety. Postgrad Med J 2001; 77: 89-93.
- Connolly BS, Fox SH. Drug treatments for the neuropsychiatric complications of Parkinsons disease. Expert Rev Neurother 2012; 12: 1439-1449.
- Qureshi SU, Amspoker AB, Calleo JS, Kunik ME, Marsh L. Anxiety disorders, physical illnesses, and health care utilization in older male veterans With Parkinson disease and comorbid depression. J Geriatr Psych Neurol 2012; 25: 233-239.
- Stacy M. Nonmotor symptoms in Parkinsons disease. Int J Neurosci 2011; 121: 9-17.
- Forjaz MJ, Martinez-Martin P, Dujardin K, Marsh L, Richard IH, Starkstein SE, Leentjens AF. Rasch analysis of anxiety scales in Parkinsons disease. J Psychosom Res 2013; 74: 414-419.
- Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH. Symptomatology and markers of anxiety disorders in Parkinsons disease: a cross-sectional study. Mov Disord 2011; 26: 484-492.
- Chen JJ, Marsh L. Anxiety in Parkinsons disease: identification and management. Ther Adv Neurol Disord 2014; 7: 52-59.
- Weintraub D, Hoops S. Anxiety syndromes and panic attacks. Parkinsons disease: non-motor and non-dopaminergic features. John Wiley Sons 2011; 193-201.
- Shulman LM, Taback RL, Rabinstein AA, Weiner WJ. Non-recognition of depression and other non-motor symptoms in Parkinsons disease. Parkinson Relat Disord 2002; 8: 193-197.
- Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE, Goetz CG. Anxiety rating scales in Parkinsons disease: critique and recommendations. Mov Disord 2008; 23: 2015-2025.
- Beck A, Steer R. Beck anxiety inventory. Manual Psychological Corporation. San Antonio TX 1993.
- Spielberger CD, Gorsuch RLL. STAI Manual for the State Trait Inventory (self-evaluation questionnaire). Palo Alto California Consulting Psychologists Press 1970.
- Iruela LM, Ibanez-Rojo V, Palanca I, Caballero L. Anxiety disorders and Parkinsons disease. Am J Psychiatry 1992; 149: 719-720.
- Stein MB, Heuser IJ, Juncos JL, Uhde TW. Anxiety disorders in patients with Parkinsons disease. Am J Psychiatry 1990; 147: 217-220.
- Menza MA, Palermo B, Di Paola R, Sage JI, Ricketts M.H. Depression and anxiety in Parkinsons disease: Possible effect of genetic variation in the serotonin transporter. J Geriatr Psych Neurol 1999; 12: 49-52.
- Kano O, Ikeda K, Cridebring D, Takazawa T, Yoshii Y. Neurobiology of depression and anxiety in Parkinsons disease. Parkinsons Dis 2011; 2011: 143547.
- Prediger R, Matheus FC, Schwarzbold ML, Lima M, Vital M. Anxiety in Parkinson’s disease: a critical review of experimental and clinical studies. Neuropharmacol 2012; 62: 115-124.
- Xiang L, Szebeni K, Szebeni A, Klimek V, Stocm Meir CA, Karolewicz B, Ordway GA. Dopamine receptor gene expression in human amygdaloid nuclei: elevated D4 receptor mRNA in major depression. Brain Res 2008; 1207: 214-224.
- Hanna KK, Cronin Golomb A. Impact of anxiety on quality of life in Parkinson’s disease. Parkinsons Dis 2012; 1-8.
- Tan LC. Mood disorders in Parkinsons disease. Parkinsonism Relat Disord 2012; 18: 74-76.
- Jacob EL, Gatto NM, Thompson A, Bordelon Y, Ritz B. Occurrence of depression and anxiety prior to Parkinsons disease. Parkinsonism Relat Disord 2010; 16: 576-581.
- Thanvi BR, Munshi SK, Vijaykumar N, Lo TC. Neuropsychiatric non-motor aspects of Parkinsons disease. Postgrad Med J 2003; 79: 561-565.
- Foster PS, Drago V, Yung RC, Skidmore FM, Skoblar B, Shenal BV, Heilman KM. Anxiety affects working memory only in left hemibody onset Parkinson disease patients. Cogn Behav Neurol 2010; 23: 14-18.
- Carod-Artal FJ, Ziomkowski S, Mourao H, Martinez P. Anxiety and depression: main determinants of health-related quality of life in Brazilian patients with Parkinson’s disease. Parkinson Relat Disord 2008; 14: 102-118.
- Marin RS, Biedrzycki RC, Firinciogullari S. Reliability and validity of the apathy evaluation scale. Psychiatry Res 1991; 38: 143-162.
- Pedersen KF, Alves G, Aarsland D, Largen JP. Occurrence and risk factors for apathy in Parkinson’s disease: A 4-year prospective longitudinal study. J Neurol Neurosurg Psych 2009; 80: 1279-1282.
- Bottini Bonfanti A, Etcheverry JL, Persi GG, Zezza H, Starkstein S. Apathy in Parkinsons disease. Impairment in quality of life. Medicina (B Aires) 2009; 69: 253-258.
- Garcia-Ramos R, Villanueva C, del Val J, Matías-Guiu J. Apathy in Parkinsons disease. Neurologia 2010; 25: 40-50.
- Varanese S, Perfetti B, Ghilardi MF, Di Rocco A. Apathy, but not depression, reflects inefficient cognitive strategies in Parkinson’s disease. Plos One 2011; 6: 1-6.
- Isella V, Melzi P, Grimaldi M, Iurlaro S, Pioltti R, Ferrarese C, Appollonio I. Clinical, neuropsychological and morphometric correlates of apathy in Parkinson’s disease. Mov Disord 2002; 17: 366-371.
- Robert G, Jeune F, Lozchmeur C, Drapier S, Thibault D, Peron J, Drapier D. Apathy in patients with Parkinson’s disease without dementia or depression. Neurology 2012; 79: 1155-1160.
- Starkstein SE, Leentjens AF. The nosological position of apathy in clinical practice. J Neurol Neurosurg Psych 2008; 79: 1088-1092.
- Ahearn DJ, McDonald K, Barraclough M, Leroi I. An exploration of apathy and impulsivity in Parkinson disease. Curr Gerontol Geriatr Res 2012.
- Starkstein SE, Merello M, Jorge R, Brockman S, Bruce D, Power B. The syndromal validity and nosological position of apathy in Parkinson’s disease. Mov Disord 2009; 8: 1211-1216.
- Sockeel P, Dujardin K, Devos D, Deneve C, Destee A, Defebvre L. The Lille Apathy Rating Scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinsons disease. J Neurol Neurosurg Psych 2006; 77: 579-584.
- Garcia R. Validation of the Lars scale of apathy in Parkinson’s disease. Repositorio Universidad Complutense de Madrid Spain 2010.
- Cummings JL, Mega M, Gray RTS, Carusi DA, Gornbein J. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994; 44: 2308-2314.
- Harris E, McNamara P, Durso R. Apathy in patients with Parkinson disease as a function of side of onset. J Geriatr Psychiatry Neurol 2013; 26: 95-104.
- Laatu S, Karrasch M, Martikainen K, Martila R. Apathy is associated with activities of daily living ability in Parkinson’s disease. Dementia Geriatr Cogn Disord 2013; 35: 5-6.
- Leon JB, Cubo E, Coronell C. Impact of apathy on health-related quality of life in recently diagnosed Parkinson’s disease: the ANIMO study. Mov Disord 2011; 27: 211-218.
- Pluck GC, Brown RG. Apathy in Parkinsons disease. J Neurol Neurosurg Psychiatry 2002; 73: 636-642.
- Zgaljardic DJ, Borod JC, Foldi NS, Rocco M, Mattis PJ, Gordon MF, Eidelberg D. Relationship between self-reported apathy and executive dysfunction nondemented patients with Parkinson’s disease. Cogn Behav Neurol 2007; 20: 184-192.
- Louis ED, Huey ED, Gerbin M, Viner A. Apathy inessential tremor, dystonia, and Parkinson’s disease: a comparison with normal controls. Mov Disord 2012; 27: 432-434.
- Ziropadja LJ, Stefanova E, Petrovic M, Stojkovic T, Kostic VS. Apathy and depression in Parkinson’s disease: the Belgrade PD study report. Parkinson Relat Disord 2012; 18: 339-342.
- Storch A, Schneider CB, Wolz M, Sturwald Y, Nebe A, Odin P, Ebersbach G. Nonmotor fluctuations in parkinson’s disease: severity and correlation with motor complications. Neurology 2013; 80: 800-809.
- Starkstein SE, Brockman S, Hayhow BD. Psychiatric syndromes in Parkinsons disease. Curr Opin Psychiatry 2012; 25: 468-472.