Research Article - Journal of Clinical Dentistry and Oral Health (2023) Volume 7, Issue 1
DMFT Score in Cardiovascular Disorder Versus Non-Cardiovascular Disorder Patients
Sathvika K and Mahalakshmi J*
Department of Conservative dentistry and endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India
- Corresponding Author:
- Mahalakshmi J
Department of Conservative dentistry and endodontics
Saveetha Dental College and Hospitals
Saveetha Institute of Medical and Technical Sciences
Saveetha University
E-mail id: mahalakshmij.sdc@saveetha.com
Received: 26-Dec-2022, Manuscript No. AACDOH-22-84042; Editor assigned: 28-Dec-2022, PreQC No. AACDOH-22-84042 (PQ); Reviewed: 12-Jan-2023, QC No. AACDOH-22-84042 (QC); Revised: 16-Jan-2023, Manuscript No. AACDOH-22-84042(R); Published: 23-January-2023, DOI: 10.35841/aacdoh-7.1.132
Citation: Sathvika K, Mahalakshmi J. DMFT score in cardiovascular disorder versus non-cardiovascular disorder patients. J Clinic Dent Oral Health. 2023;7(1):132
Abstract
Introduction: Cardiovascular disorders are responsible for over 32% of annual global deaths so patients must understand the relationship that exists between cardiovascular disorders and dental concerns. We believe that the DMFT system should efficiently be able to communicate these concerns in easy to understand numbers to the patient if there exists a difference between the DMFT scores of a cardiovascular disorder patient and a non-cardiovascular disorder patient. Aim: The aim of this study is to compare the DMFT scores of cardiovascular disorder patients and non-cardiovascular disorder patients. Materials and methodology: A retrospective cross-sectional study was conducted using established records of calculated DMFT scores as mentioned in the hospital’s online database from Saveetha Dental College between April 2020 and March 2021. Relevant data such as patient age, sex, type of cardiovascular status, DMFT score and their medication utilization status was acquired. This data was recorded in a Microsoft Excel spreadsheet and was later exported to the Statistical Package for the Social Sciences for Windows for statistical analysis. A Chi Square test was used with the level of significance set at p<0.05. Results and discussion: The findings of our study suggest that there is a statistically significant difference between the DMFT scores of a cardiovascular disorder and a non-cardiovascular disorder patient. Conclusion: Within the limitations of the study we may conclude that gender and drug intake have a role to play in elevating the DMFT scores in a cardiovascular disorder patient as compared to a noncardiovascular disorder patient.
Keywords
Cardiovascular disorder, Non-cardiovascular, DMFT, Gender, Innovative
Introduction
The DMF (Decayed, Missing and Filled) index has been successfully employed for almost 80 years [1] and has long since been established as the ‘key measure of dental caries experience in dental epidemiology’ [2]. It is used only on permanent teeth and is expressed as the total number of teeth or surfaces that are decayed (D), missing (M) or filled (F) in an individual [3]. When the index is applied to the teeth as a whole unit it is called the DMFT index and its scores can range from 0 to 28 or 32 depending on whether or not the third molars were included in the scoring [4]. Likewise, when the index is applied only to the tooth surfaces (five surfaces per posterior tooth and four surfaces per anterior tooth), it is called the DMFS index and its scores can range from 0 to 128 or 148 depending on whether or not the third molars were considered in the scoring. While calculating the DMFT of an individual, we do not include teeth which are unerupted, congenitally missing [5,6], supernumerary in number or teeth which were removed for reasons other than dental caries [7]. Choosing to count third molars is optional - but in our present study we have opted not to do so.
An estimated 17.9 million people died from cardiovascular disorders in 2019, representing 32% of all global deaths [8]. Out of these deaths, 85% were due to heart attacks and strokes [9]. Over three quarters of cardiovascular disorder associated deaths take place in low and middle-income countries. They are a group of disorders that affect the heart and blood vessels. They include coronary heart disease, cerebrovascular diseases [10], peripheral arterial disease [11], rheumatic heart disease, congenital heart diseases [12], deep vein thrombosis and pulmonary embolisms [13]. Heart attacks and strokes are generally acute occurrences and are mainly caused by a blockage that obstructs blood from flowing to the heart or to the brain [14]. The most common cause for this is the accumulation of fatty deposits on the inner walls of the blood vessels that supply the heart or the brain. Strokes can also be caused by bleeding from a blood vessel in the brain or from blood clots [15]. These morbid conditions have been known to be associated with exacerbated dental lesions [16], periodontal diseases [17] and oral conditions as of late and thus dental personnel and medical officers must be well informed about cardiovascular disorders.
Cardiovascular disorder patients should be treated with extra care in a dental clinic. This includes giving sound local anaesthesia to minimise the patient’s stress levels, avoiding intravascular medication injections and considering antibiotic prophylaxis. Epinephrine should be avoided or used cautiously in patients with pacemakers or automatic defibrillator devices because of the possible chance of refractory arrhythmia [18]. Cross-consultation with the patient's cardiologist is advised. In the past, cardiovascular drugs have been considered as a possible contributor for poor oral health. Also most cardiovascular patients take anticoagulants and antiplatelet based drugs which must be medically managed for dental procedures involving hemorrhage by the cardiologist and then resumed [19].
Aspirin based therapy is not a contraindication unless the patient is on very high doses for severe arthritis. Continuing medical and dental education credits should emphasize crosstraining the candidates in both areas to ensure comprehensive treatment. These patients should also be advised to quit tobacco habits [20,21], to exercise regularly, follow a low fat diet and to religiously maintain their oral hygiene. They must be comprehensive of the relationship that exists between cardiovascular disorders and dental concerns. We believe that the DMFT system should efficiently be able to communicate these concerns in easy to understand numbers to the patient if there exists a difference between the DMFT scores of a cardiovascular disorde
Our team has extensive knowledge and research experience that has translated into high quality publications [22–41]. Thus, the aim of our current study is to compare the DMFT status and scores of cardiovascular disorder patients and noncardiovascular disorder patients and to study the possible associations it may possess with drug intake and gender.
Materials and Methodology
Study design and setting
This retrospective cross-sectional institution based study examined the records of 88,950 patients from April 2020 to March 2021 undergoing various treatments at Saveetha Dental College, Chennai, India. Ethical approval was obtained from the Institutional Ethics Committee. The study population included patients with established records of calculated DMFT scores as mentioned in the hospital’s online database - Digital Information Archiving System (DIAS) of all ages. They were separated according to the presence or absence of cardiovascular disorders, gender and the use or disuse of cardiovascular drugs. Mentally or physically disabled individuals were excluded from the study.
Data collection
The records of patients who visited the hospital from April 2020 to March 2021 were analysed and were used to identify 100 patients with cardiovascular disorders and 100 patients free of cardiovascular disorders, both with established records of DMFT scores. Relevant data such as patient age, sex, type of cardiovascular status, DMFT score and their medication utilization status was acquired. Repeated patient records and patients with incomplete treatment statuses were excluded. Clinical photos and radiographs were used to verify the number, caries status and restoration status of teeth in a patient whenever necessary. The data obtained was verified by an external reviewer.
Statistical analysis
The obtained data was recorded in a Microsoft Excel 2016 spreadsheet (Microsoft Office 10) and was later exported to the Statistical Package for the Social Sciences for Windows (Version 20.0, SPSS, Inc., Chicago, U.S.A.) and was then subjected to statistical analysis. A Chi Square test was used with the level of significance set at p<0.05.
Results
The final dataset consisted of 200 patients of predominantly South Indian origin undergoing various treatments but with a recorded DMFT score. They were grouped into two equal subsets, 100 of which were patients with no past or current history of cardiovascular disorders (‘Non-Cardiovascular Disorder Patients) and 100 with established cardiovascular disorders (‘Cardiovascular Disorder Patients’). Patients were chosen from the age of 40 years onwards. Both genders were included in the study, classifying them into ‘Male’ and ‘Female’. They were further divided into ‘Yes’ and ‘No’ categories within the ‘Cardiovascular Disorder Patients’ group based on their medication use for the same. Their DMFT scores were segregated into four groups based on their severity of involvement: ‘(0-7) Teeth’, ‘(8-14) Teeth’, ‘(15-21) Teeth’ and ‘(22-28) Teeth’.
Discussion
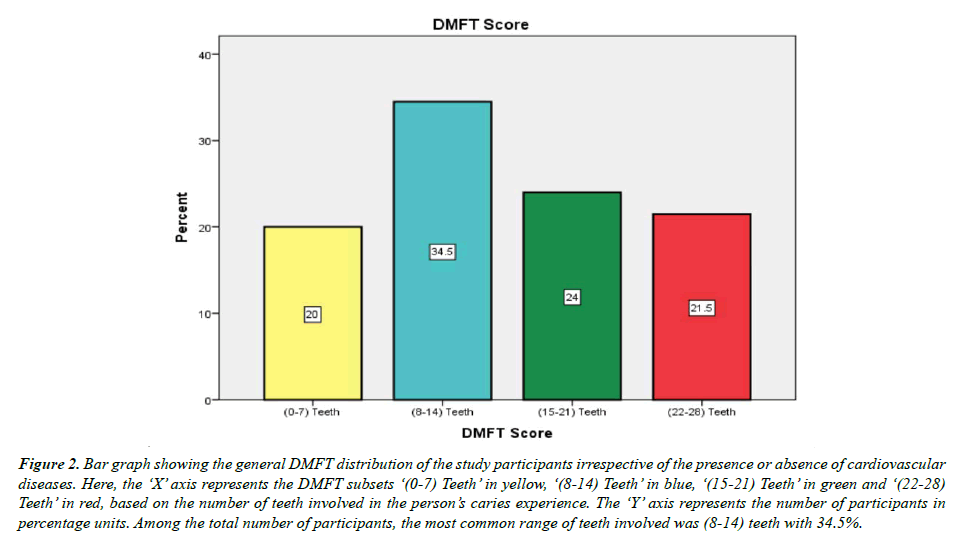
The results of Figure 1 show the general gender distribution of the study participants irrespective of the presence or absence of cardiovascular diseases. Among the total number of participants, 57.5% were females while 42.5% were males. Figure 2 shows the general DMFT distribution of the study participants irrespective of the presence or absence of cardiovascular diseases. The most common range of teeth involved was (8-14) teeth with 34.5%, followed by (15-21) teeth with 24%, followed by (22-28) teeth with 21.5% and finally (0-7) teeth with 20%. This suggests that beyond the age of 40 years it is rarer to see disease free teeth than diseased or once diseased teeth.
Figure 1: Bar graph showing the general gender distribution of the study participants irrespective of the presence or absence of cardiovascular diseases. Here, the ‘X’ axis represents the gender ‘Female’ in maroon and ‘Male’ in green. The ‘Y’ axis represents the number of participants in percentage units. Among the total number of participants, 57.5% were females while 42.5% were males.
Figure 2:Bar graph showing the general DMFT distribution of the study participants irrespective of the presence or absence of cardiovascular diseases. Here, the ‘X’ axis represents the DMFT subsets ‘(0-7) Teeth’ in yellow, ‘(8-14) Teeth’ in blue, ‘(15-21) Teeth’ in green and ‘(22-28) Teeth’ in red, based on the number of teeth involved in the person’s caries experience. The ‘Y’ axis represents the number of participants in percentage units. Among the total number of participants, the most common range of teeth involved was (8-14) teeth with 34.5%.
Figure 3 shows the distribution of the study participants who are and are not on medication for established cardiovascular disorders. Among the total number of cardiovascular disorder patients, 54% were on medication while 46% were not on any medication. These high numbers of diagnosed-but-untreated patients greatly mean that patients should be advised to begin or continue their medication as per their prescriptions more regularly.
Figure 3:Bar graph showing the distribution of the study participants who are and are not on medication for established cardiovascular disorders. Here, the ‘X’ axis represents the medication employment decisions ‘Yes’ in pink and ‘No’ in purple. The ‘Y’ axis represents the number of participants within this group in percentage units. Among the total number of cardiovascular disorder patients, 54% were on medication while 46% were not on medication.
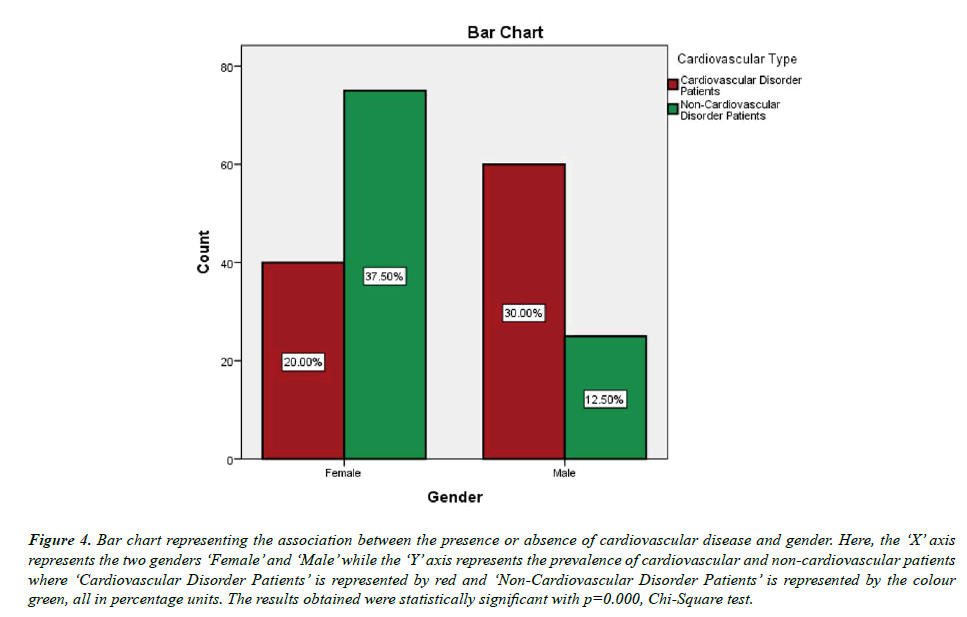
On cross tabulating gender and the presence or absence of cardiovascular disease, we obtained statistically significant results as seen in Table 1 and Figure 4, p=0.000, Chi-Square test. The values suggest that males (30%) are more likely to present with cardiovascular disorders than females (20%), despite our sample having more females in general as inferred from Figure 1. This is in line with the findings of Di Giosia, et al. [42] where they studied the gender differences that existed within cardiovascular disorders and stated that females were less likely to suffer from cardiovascular disorders as opposed to males.
Association between gender and cardiovascular type |
|||
|---|---|---|---|
| Type of Value | Value | df | Asymp. Sig. (2 Sided) |
| Pearson Chi-Square | 25.064 | 1 | 0 |
Table 1. Tabulation showing Chi-Square association between gender and the cardiovascular type, where we have obtained statistically significant results (p=0.000).
Figure 4:Bar chart representing the association between the presence or absence of cardiovascular disease and gender. Here, the ‘X’ axis represents the two genders ‘Female’ and ‘Male’ while the ‘Y’ axis represents the prevalence of cardiovascular and non-cardiovascular patients where ‘Cardiovascular Disorder Patients’ is represented by red and ‘Non-Cardiovascular Disorder Patients’ is represented by the colour green, all in percentage units. The results obtained were statistically significant with p=0.000, Chi-Square test.
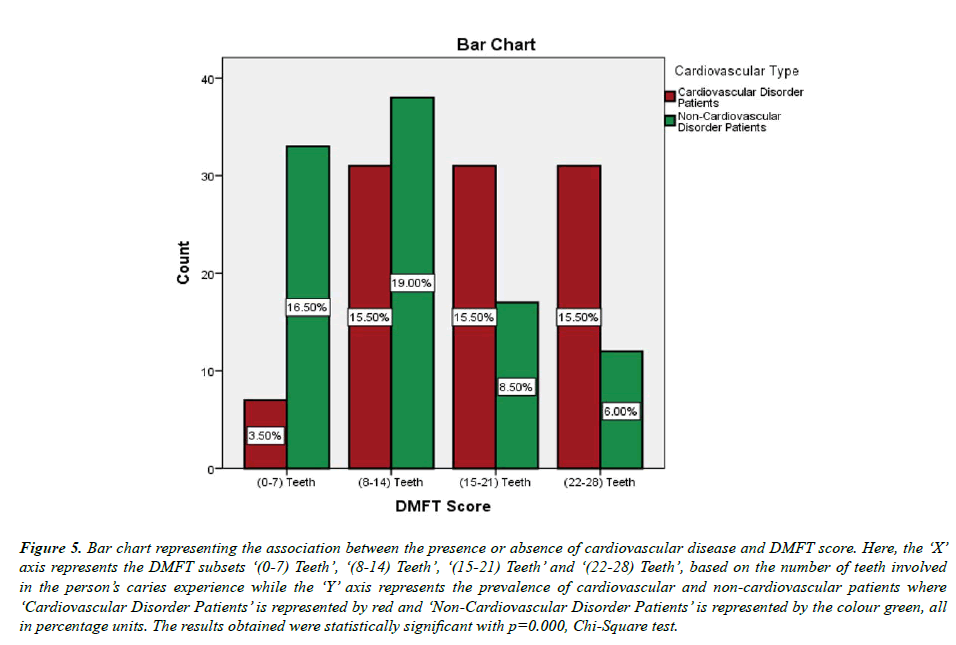
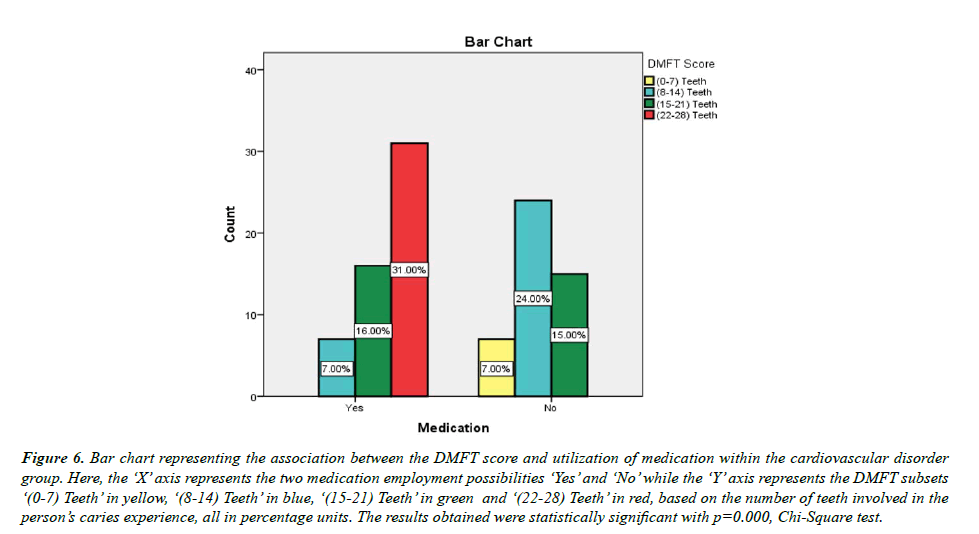
Figure 5 and Table 2 explain the association between the presence or absence of cardiovascular disease and the DMFT score of a patient where we observed statistically significant results, p=0.000, Chi-Square test. It suggests that in the subset of (0-7) teeth and (8-14) teeth, it is more common to appreciate cardiovascular disorder free patients (16.5% and 19% respectively), while in the subsets of (15-21) teeth and (22-28) teeth it is more common to see cardiovascular disorder ridden patients (15.5% for both). Overall this translates into the fact that cardiovascular disorder patients have a more severe caries experience as compared to non-cardiovascular disorder patients. This is in agreement with the results of a study conducted in 2013 by Pimentel et al. [43] in children with congenital heart diseases, where they concluded that higher DMFT scores were associated with heart diseases. They also mentioned that daily drug intake increased the scores and the number of missing teeth. This is similar to the results of Figure 6 and Table 3 where the association between the DMFT score and medication utilization within the cardiovascular disorder group obtained statistically significant results, p=0.000, Chi- Square test. Out of the medication users, most of them had (22- 28) teeth involved (31%), followed by (15-21) teeth in 16% and finally 7% for (8-14) teeth. It is interesting to note that not a single patient on cardiovascular medication had scores in the range of (0-7) teeth as opposed to the medication free group with 7% having (0-7) teeth scores. This conclusively suggests that medication intake greatly plays a role in increasing the DMFT scores of an individual suffering from cardiovascular disorders.
| Association between DMFT Score and cardiovascular type | |||
|---|---|---|---|
| Type of Value | Value | df | Asymp. Sig. (2 Sided) |
| Pearson Chi-Square | 30.089 | 3 | 0 |
Table 2. Tabulation showing Chi-Square association between the DMFT Score and the cardiovascular type, where we have obtained statistically significant results (p=0.000).
| Association between Medication and DMFT Score | |||
|---|---|---|---|
| Type of Value | Value | df | Asymp. Sig. (2 Sided) |
| Pearson Chi-Square | 47.016 | 3 | 0 |
Table 3. Tabulation showing Chi-Square association between the DMFT Score and medication utilization within the cardiovascular disorder group, where we have obtained statistically significant results (p=0.000).
Figure 5:Bar chart representing the association between the presence or absence of cardiovascular disease and DMFT score. Here, the ‘X’ axis represents the DMFT subsets ‘(0-7) Teeth’, ‘(8-14) Teeth’, ‘(15-21) Teeth’ and ‘(22-28) Teeth’, based on the number of teeth involved in the person’s caries experience while the ‘Y’ axis represents the prevalence of cardiovascular and non-cardiovascular patients where ‘Cardiovascular Disorder Patients’ is represented by red and ‘Non-Cardiovascular Disorder Patients’ is represented by the colour green, all in percentage units. The results obtained were statistically significant with p=0.000, Chi-Square test.
Figure 6:Bar chart representing the association between the DMFT score and utilization of medication within the cardiovascular disorder group. Here, the ‘X’ axis represents the two medication employment possibilities ‘Yes’ and ‘No’ while the ‘Y’ axis represents the DMFT subsets ‘(0-7) Teeth’ in yellow, ‘(8-14) Teeth’ in blue, ‘(15-21) Teeth’ in green and ‘(22-28) Teeth’ in red, based on the number of teeth involved in the person’s caries experience, all in percentage units. The results obtained were statistically significant with p=0.000, Chi-Square test.
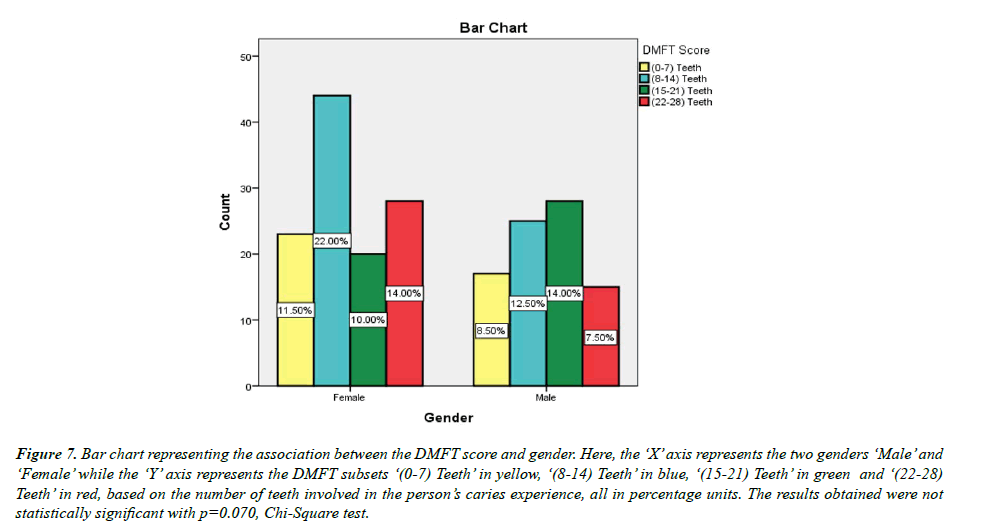
Figure 7 talks about the association between gender and the DMFT score. These results were not statistically significant as seen in Table 4, p=0.070, Chi-Square test.
Figure 7:Bar chart representing the association between the DMFT score and gender. Here, the ‘X’ axis represents the two genders ‘Male’ and ‘Female’ while the ‘Y’ axis represents the DMFT subsets ‘(0-7) Teeth’ in yellow, ‘(8-14) Teeth’ in blue, ‘(15-21) Teeth’ in green and ‘(22-28) Teeth’ in red, based on the number of teeth involved in the person’s caries experience, all in percentage units. The results obtained were not statistically significant with p=0.070, Chi-Square test.
| Association between gender and DMFT score | |||
|---|---|---|---|
| Type of Value | Value | df | Asymp. Sig. (2 Sided) |
| Pearson Chi-Square | 7.054 | 3 | 0.07 |
Table 4. Tabulation showing Chi-Square association between gender and the DMFT score, where we have not obtained statistically significant results (p=0.070).
On analysing all the values we have obtained, we see that cardiovascular disorder patients tend to have higher DMFT scores and that males are more likely to suffer from cardiovascular disorders than females and daily drug intake can influence the DMFT score of a cardiovascular patient. As the study does present certain limitations like the inherent insufficiencies associated with the DMFT index, small sample size, similar ethnicity and bias risk, further research is needed to cross-examine our findings.
Limitations of the Study
Our small sample size where most of the participants are from South Indian cities lowers the reliability and generalizability of our results with respect to other populations.
Future Scope of the Study
The study can be further bettered by involving a higher number of patient records from other ethnicities and populations as well, thus overcoming our geographical barriers and small sample size and increasing the reliability of our findings.
Conclusion
Within the limits of our study, we conclude that DMFT scores of cardiovascular disorder patients are higher than that of a non-cardiovascular disorder patient. Gender and drug intake also present as risk factors for altered DMFT scores and we believe that further research is required to fully understand these relationships for providing efficient long-term treatment.
Acknowledgment
The authors of this study would like to thank and acknowledge the constant help and guidance offered by the Department of Aesthetic Dentistry of Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Chennai.
Funding Support
Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University, India
Conflict of Interest
None declared.
References
- Prabakar J, John J, Srisakthi D. Prevalence of dental caries and treatment needs among school going children of Chandigarh. Indian J Dent Res. 2016;27(5):547–552.
- Zhang S, Liu J, Lo ECM, et al. Dental caries status of Bulang preschool children in Southwest China. BMC Oral Health. 2014;14:16.
- Syamkumar V, Thomas AJ, Oommen S, et al. Relationship between body mass index and dental caries in 13–15-year-old school children of government and private schools in Bengaluru City. J Pharm Bioallied Sci. 2021;13:S841.
- Mohammadi S, Mohammadi MA, Dadkhah B. Dental caries prevalence among elementary school students and its relationship with body mass index and oral hygiene in Ardabil in 2019. J Indian Soc Pedod Prev Dent. 2021;39(2):147–153.
- Mishra R, Singh AK, Tyagi S, et al. Prevalence of oral health status and needs in institutionlized physically challenged children. J Pharm Bioallied Sci. 2021;13(1):184–186.
- Singh AK, Mishra R, Kumar H, et al. Assessment of oral health-care needs for patients under palliative care. J Pharm Bioallied Sci. 2021;13(1):180–183.
- Hung HV, Ngoc VT, Vu Thi H, et al. Early childhood caries in obese children: The status and associated factors in the Suburban areas in Hanoi, Vietnam. Int J Environ Rese Public Health. 2021;18(16):8844.
- Dawwas GK, Barnes GD, Dietrich E, et al. Cardiovascular and major bleeding outcomes with antiplatelet and direct oral anticoagulants in patients with acute coronary syndrome and atrial fibrillation A population-based analysis. Am Heart J. 2021;42:71-81.
- Velde GT, Plasqui G, Willeboordse M, et al. Associations between physical activity, sedentary time and cardiovascular risk factors among Dutch children. PLoS One. 2021;16(8):e0256448.
- Papageorgiou N. Cardiovascular diseases: Genetic susceptibility, environmental factors and their interaction. Academic Press, 2016;252.
- Warrell DA, Cox TM, Benz EJ, et al. Oxford textbook of medicine. Oxford University Press 2003.
- Dhalla NS, Rupp H, Angel A, et al. Pathophysiology of cardiovascular disease. Springer Science and Business Media 2012;648.
- https://nap.nationalacademies.org/catalog/12815/promoting-cardiovascular-health-in-the-developing-world-a-critical-challenge
- Taylor RB. Taylor’s cardiovascular diseases: A handbook. Springer Science and Business Media 2005;294.
- Baune BT, Tully PJ. Cardiovascular diseases and depression: Treatment and prevention in psychocardiology. Springer 2016;533.
- Asai K, Yamori M, Yamazaki T, et al. Tooth loss and atherosclerosis: The Nagahama study. J Dent Res. 2015;94(3):52–58.
- Jiménez C, Garrido M, Pussinen P, et al. Systemic burden and cardiovascular risk to Porphyromonas species in apical periodontitis. Clin Oral Investig. 2022;26(1):993-1001.
- Mask AG. Medical management of the patient with cardiovascular disease. Periodontology. 2000;23:136-41.
- Ataya A, Chung J, Cope J, et al. Pulmonary arterial hypertension medical management of the adult patient with congenital heart disease. Cardiovasc Innov Appl. 2018;3(1):1-8.
- Mahoney MC, Rivard C, Hammad HT, et al. Cardiovascular Risk Factor and disease measures from the Population Assessment of Tobacco and Health (PATH) study. Int J Environ Res Public Health. 2021;18(14).
- Zhao YF, Zhang T, Wang ZQ, et al. Burden of cardiovascular disease from 1990 to 2017 in Henan Province, China. Glob Health Action. 2021;14(1):1959708.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym. 2021;260:117774.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod. 2021;47(8):1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A review of prolonged post-COVID-19 symptoms and their implications on dental management. Int J Environ Res Public Health. 2021;18(10).
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett. 2021;19(3):2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal-A sign of superiority? J Dent Sci. 2020;15(4):562.
- Narendran K, MS N, Sarvanan A. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. Indian J Pharm Sci. 2020;82(5):909-912.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental caries profile and associated risk factors among adolescent school children in an Urban South-Indian city. Oral Health Prev Dent. 2020;18(1):379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal microcracks after root canal instrumentation using instruments manufactured with different NiTi alloys and the SAF system: A systematic review. Adv Sci Inst Ser E Appl Sci. 2021;11(11):4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the antioxidant and cytocompatibility of Mimusops elengi linn extract over human gingival fibroblast cells. Int J Environ Res Public Health. 2021;18(13).
- Karobari MI, Basheer SN, Sayed FR, et al. An in vitro stereomicroscopic evaluation of bioactivity between Neo MTA Plus, Pro Root MTA, BIODENTINE & glass ionomer cement using dye penetration method. Materials. 2021;14(12).
- Rohit Singh T, Ezhilarasan D. Ethanolic extract of Lagerstroemia speciosa (L.) Pers., induces apoptosis and cell cycle arrest in HepG2 cells. Nutr Cancer. 2020;72(1):146–156.
- Ezhilarasan D. MicroRNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol. 2020;885:173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: A multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2018;3(12):845–855.
- Raj RK. β-Sitosterol-assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Mater Res. 2020;108(9):1899–1908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol. 2019;90(12):1441–1448.
- Priyadharsini JV, Girija AS, Paramasivam A. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol. 2018;94:93-98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res. 2020;34:e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent. 2020;44(6):423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J. 2021;230(6):345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. Chem Select. 2020;5(7):2322–2331.
- Di Giosia P, Passacquale G, Petrarca M, et al. Gender differences in cardiovascular prophylaxis: Focus on antiplatelet treatment. Pharmacol Res. 2017;119:36–47.
- Pimentel ELC, Azevedo VMP, de Almeida Lima Castro R, et al. Caries experience in young children with congenital heart disease in a developing country. Bra Oral Res. 2013;27:103–108.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref