Research Article - Journal of Child and Adolescent Health (2025) Volume 9, Issue 1
Differences and factors associated with dyslipidemias in American adolescents of Hispanic and Asian Indian descent.
Naveen Mehrotra1*, Nayan Mehrotra2, Anna Petrova3
1Department of Pediatrics, Shri Krishna Nidhi Foundation, Hillsborough, NJ, USA
2Department of Medicine, Saint George's School of Medicine, St. George, Grenada
3Department of Pediatrics, Rutgers Robert Wood Johnson Medical School, Brunswick, New Jersey, USA
*Corresponding Author:
- Naveen Mehrotra
- Department of Pediatrics,
- Shri Krishna Nidhi Foundation,
- Hillsborough, NJ, USA
E-mail: nmehrotra@sknfoundation.org
Received: 21-Jan-2024, Manuscript No. AAJCAH-24-125562; Editor assigned: 24-Jan-2024, AAJCAH-24-125562 (PQ); Reviewed: 07-Feb-2024, QC No. AAJCAH-24-125562; Revised: 15-Jan-2025, Manuscript No. AAJCAH-24-125562 (R); Published: 22-Jan-2025, DOI: 10.35841/aajcah-9.1.246
Citation: Mehrotra N, Mehrotra N, Petrova A. Differences and factors associated with dyslipidemias in American adolescents of Hispanic and Asian Indian descent. J Child Adolesc Health. 2025;9(1):246
Abstract
Introduction: Hispanics, South Asians, and African American have demonstrated disproportionately high manifestation of abnormal lipid profiles in obese adolescents and those with a family history of Cardiovascular (CV) diseases. Results of lipid screening during routine preventive care pediatric visits in Hispanic and Asian Indian adolescents which have not been routinely reported were analyzed.
Methods: Demographic and clinical data, including age, gender, health insurance coverage, and anthropometric parameters at time of lipid screening were utilized. Blood sugar and lipid profile measurements, including total cholesterol, low-density lipoprotein, triglyceride, and high-density lipoprotein were categorized as acceptable, borderline, high, or as combined dyslipidemia by stages of adolescence of early, middle, and late and sex-age based percentile for body mass index category of overweight and obese adolescents. Univariate analysis using chi-square and analysis of variance identified dyslipidemia categories between Asian Indians and Hispanic adolescents based on age stage.
Results: Overall, 428 adolescents, 244 Asian Indians and 184 Hispanics included 41.4% in early, 45.8% in middle, and 12.8% in late age stages were studied. A significantly higher proportion of Hispanics of any age stage had abnormal BMI. Average blood lipid concentrations of TC, LDL-C, and HDL-C were higher in Asian Indians in early and middle age stages. Combined data of adolescents in middle and late age stages identified a higher rate of multifactorial dyslipidemia in Asian Indians.
Conclusion: Routine lipid screening should be implemented as unidentified overweight/obese adolescents predicted all types of dyslipidemias, irrespective of ethnicity, gender, and age.
Keywords
Adolescents, Dyslipidemia, Asian Indian American, Hispanic, Risk factors
Introduction
The compelling evidence supports the role of racial/ethnic differences in dyslipidemia patterns and Cardiovascular (CV) risk in U.S. adults [1-3]. However, data concerning cultural diversity's role in dyslipidemia occurrence in childhood is limited. Lipids' pathological concentration has often been detected in childhood [4]. Despite the favorable trend of lipid levels in U.S. youth, 1 in 10 adolescents had abnormal levels of Low-Density Lipoprotein (LDL-C) or Total Cholesterol (TC), and 1 in 5 had one of the abnormal lipid test, including TC, High-Density Lipoprotein (HDL-C), or non-HDL-C [5-7]. The American heart association has recognized the association of risk-reduction of early subclinical atherosclerosis with no description of a pathological lipid profile in childhood [8,9]. Therefore, it could be essential to understand the role of different factors, including ethnicity, in developing dyslipidemia in childhood. Moreover, the U.S. Preventive Services Task Force (USPSTF) has suggested the importance of such knowledge for developing strategies to reduce the risk of long-term consequences of dyslipidemias in childhood [10]. Studies have reported a high prevalence of dyslipidemias among U.S. Hispanics and Asians, including the Asian Indian subgroup, as well as a disproportionately high manifestation of CV morbidity and mortality recorded in Hispanic and Asian Indian adults [11]. Therefore, it becomes essential to analyze the pattern of dyslipidemia in Hispanic and Asian Indian adolescents. Although in 2011, the National Heart, Blood and Lung Institute and the American Academy of Pediatrics (AAP) introduced universal lipid screening for children and adolescents, practicing universal lipid screening by primary care pediatricians is limited [12]. Even though nearly 60% of the pediatricians agreed with the overall idea regarding universal lipid screening, most prescribed lipid profile testing in obese adolescents and those with a family history of CV diseases, which restricts the investigation of the role of cultural diversity in the prevalence of dyslipidemias in the pediatric population [13]. To our knowledge, only one study that used data on selective lipid screening of children aged 3 to 19 revealed an increased prevalence of elevated TC and reduced HDL-C in Hispanics compared to white adolescents [14]. The proposed study provides analyses of new data concerning agebased probability for dyslipidemias across two screened ethnic groups of Hispanic and Asian Indian adolescents from a pediatric practice during preventive care pediatric visits. The primary purpose was to identify if there is a variation in rates of lipid profile abnormalities between Hispanic and Asian Indian adolescents and to define the role of essential health determinants, such as age stages, gender, and childhood obesity on the obtained findings [15].
Materials and Methods
In this retrospective study, our previously collected and published data on universal lipid screening of Asian Indian adolescents were compared to those in Hispanic pediatric patients that also underwent universal lipid screening at the same primary care pediatric practice, but in another location [16]. This location provides care mostly for Hispanic children because of the predominance of Hispanic population in the region. The procedure for identifying potential study subjects and the type of collected data were uniformly applied because the same electronic system connects two locations. We used the Current Procedural Terminology (CPT) codes for preventive care office visits (99393, 99394, 99395, 99383, 99384, and 99385) to identify medical records of patients aged 10 to 20-year-old who underwent lipid screening. The selected medical records were reviewed to collect demographic and clinical data, including age (years), gender, health insurance coverage (government, commercial), and anthropometric parameters (weight, height) at the time of lipid screening. The laboratory reports of blood sugar and lipid profile measurements, including Total Cholesterol (TC), Low-Density Lipoprotein (LDL-C), Triglyceride (TG), and High-Density Lipoprotein (HDL-C), were collected.
Definition of types of dyslipidemia, age-stages, and Body Mass Index (BMI)
We used cutoff points of TC, LDL-C, TG, and HDL-C to categorize acceptable, borderline, or high levels. We identified adolescents with normal lipid profiles if all measures were at acceptable levels. Borderline dyslipidemia was classified if a single or combination of TC was from 170 to 199 mg/dL, LDL-C from 110 to 129 mg/dL, or TG from 90 to129 mg/dL. High dyslipidemia was classified if a single or combination of TC ≥ 200 mg/dL, or LDL-C ≥ 130 mg/dL, or TG ≥ 130 mg/dL or HDL-C<40 mg/dL were detected. The threshold points represented 95th and 75th percentiles for high and borderline and 10th percentile for low threshold points for HDL-C. We also calculated the TG/HDL-C ratio to classify Combined
Dyslipidemia (CD) using the cutoff point of 3, which suggested the definition of CD in whites. In addition, patients with multifactorial dyslipidemia were identified if TC level was ≥ 200 mg/dL and/or LDL-C level was ≥ 130 mg/dL. Stages of adolescence life 15 were classified as follows: Early (10 to 13 years), middle (14 to 17 years), and late (18-21 years) stages. Sex-age based percentile for Body Mass Index (BMI) from 85th to below 95th and 95th and above percentile categorized overweight and obese adolescents.
Statistical analysis
The univariate analysis compared gender, BMI-defined abnormalities, average blood lipid quantities, and classified dyslipidemia categories between Asian Indians (group 1) and Hispanics (group 2) adolescents based on age stage using chi square and Analysis of Variance (ANOVA). We constructed a stepwise logistic regression model to define the independent association of different types of dyslipidemias with ethnicity (Hispanic vs. Asian Indian) after controlling for age, gender, and overweight/obesity. Data presented as a rate (%), mean with standard deviation (+/- SD), and Odds Ratios (OR) with a 95% Confidence Interval (95% CI). We used STATISTICA 13.3 (StatSoft Inc., Tulsa, OK, USA). All statistical tests were 2-sided, with the significance level set at a P-value of <.05.
Results
Overall, 428 adolescents, including 177 (41.4%) in early, 196 (45.8%) in the middle, and 55 (12.8%) in late age stages, were studied. Group 1 and group 2 constituted 244 Asian Indians and 184 Hispanic adolescents. Because of difference in social economic status, all Asian Indian patients in our study were covered by commercial and Hispanic by government health insurance. Group 1 included more likely early age stage adolescents and less likely in the middle age stage than group 2 (Table 1). The gender in group 1 and 2 were comparable in the adolescents of early and late stages, but the increased proportion of the middle age males in group 2. A significantly higher proportion of adolescents of any age stage in group 2 had abnormal BMI than in group 1. The average blood lipid concentrations of TC, LDL-C, and HDL-C were higher in group 1 than in group 2 adolescents in early and middle age stages. The average fasting glucose levels were normal in groups 1 and 2. Only 5.5% (13/236) adolescents in group 1 and 7.6% (14/184) in group 2 had glucose levels between 101 to 128 mg/dL, respectively (P=0.36).
| Factors | Early age stage (n=177) | Middle age stage (n=196) | Late age stage (n=55) | |||
| G1 (n=133) | G2 (n=44) | G1 (n=89) | G2 (n=107) | G1 (n=22) | G2 (n=33) | |
| Male sex (%) | 45.9% | 54.5% | 41.6% | 57.9%* | 45.6% | 54.6% |
| Proportion in age stage (%) | 54.5% | 23.7%*** | 36.5% | 75.55** | 9.0% | 17.7% |
| Normal weight | 56.4% | 36.4% | 68.5% | 45.8% | 76.2% | 45.4% |
| Overweight | 31.6% | 18.2% | 16.9% | 29.0% | 23.8% | 27.3% |
| Obese | 12.0% | 45.4%** | 14.6% | 25.2%** | 0% | 27.3%* |
| TC (mg/dL) | 159.8 ± 26.1 | 148.6 ± 25.3* | 158.8 ± 30.4 | 144.1 ± 25.2** | 165.8 ± 39.5 | 156.8 ± 34.1 |
| LDL-C (mg/dL) | 88.4 ± 23.1 | 79.9 ± 27.2* | 87.7 ± 26.3 | 77.7 ± 21.9** | 95.4 ± 33.9 | 87.1 ± 29.5 |
| HDL-C (mg/dL) | 53.8 ± 12.8 | 48.3 ± 11.6** | 51.8 ± 11.3 | 46.6 ± 10.2** | 49.3 ± 10.9 | 49.2 ± 12.7 |
| TG (mg/dL) | 88.1 ± 43.1 | 97.7 ± 46.1 | 92.5 ± 42.2 | 99.9 ± 54.8 | 99.6 ± 47.1 | 104.9 ± 58.7 |
| Glucose (mg/dL) | 89.1 ± 7.5 | 91.4 ± 5.6 | 89.3 ± 7.6 | 90.0 ± 6.8 | 85.2 ± 9.6 | 88.8 ± 9.5 |
| Note: *P<0.05-P<0.02; **P<0.01-P<0.0001 (P value based on Chi-square for comparison categorical and ANOVA for comparison continuous data). G1: Asian Indian; G2: Hispanic | ||||||
Table 1. Ethnic groups and age stage based comparison of study participants (%, Mean ± SD).
Group-based comparison of acceptable lipid levels
Asian Indians were less likely than Hispanic adolescents to have had acceptable values of TC (66.0% vs. 82.6%, P<0.001) and LDL-C (79.9% vs. 89.7%, P<0.01) and more likely to have had HDL >40 mg/dL than Hispanic adolescents (69.8% vs. 53.3%, P<0.01). We recorded a comparable rate of acceptable concentration of TG between group 1 and 2 (57.4% vs. 50.5%, P=0.33). Age stage analysis showed a lower acceptable TC and LDL-C rate in Asian Indian adolescents in their middle age than in Hispanics. The acceptable TG and HDL rates between Asian Indians and Hispanics of different ages were not statistically significant (Table 2).
| Lipid category | Early age stage (n=177) | Middle age stage (n=196) | Late age stage (n=55) | |||
| G1 (n=133) | G2 (n=44) | G1 (n=89) | G2 (n=107) | G1 (n=22) | G2 (n=33) | |
| TC | ** | |||||
| High | 6.0% | 6.8% | 7.9% | 2.8% | 18.2% | 6.1% |
| Borderline | 26.3% | 13.6% | 27.0% | 9.4% | 22.7% | 24.2% |
| Acceptable | 67.7% | 79.6% | 65.1% | 87.8% | 59.1% | 69.7% |
| LDL-C | * | |||||
| High | 4.5% | 4.6% | 3.4% | 1.9% | 13.6% | 12.1% |
| Borderline | 13.5% | 11.4% | 16.8% | 5.6% | 13.6% | 0% |
| Acceptable | 82.0% | 84.0% | 79.8% | 92.5% | 72.0% | 87.9% |
| TG | ||||||
| High | 18.0% | 18.2% | 20.2% | 22.4% | 22.7% | 36.4% |
| Borderline | 24.1% | 34.1% | 22.5% | 24.3% | 18.2% | 18.2% |
| Acceptable | 57.9% | 47.7% | 57.3% | 53.3% | 54.6% | 45.4% |
| HDL-C | ||||||
| Low | 9.0% | 20.5% | 16.9% | 27.1% | 13.6% | 15.2% |
| Borderline | 20.3% | 25.0% | 15.7% | 22.4% | 13.6% | 24.2% |
| High | 70.7% | 54.5% | 67.4% | 50.5% | 72.7% | 60.6% |
| Note: *P<0.05; **P<0.01 (P value based on Chi-square). | ||||||
Table 2. Ethnic group and age stage analysis of classified lipid profile abnormalities.
Group-based comparison of dyslipidemia rates
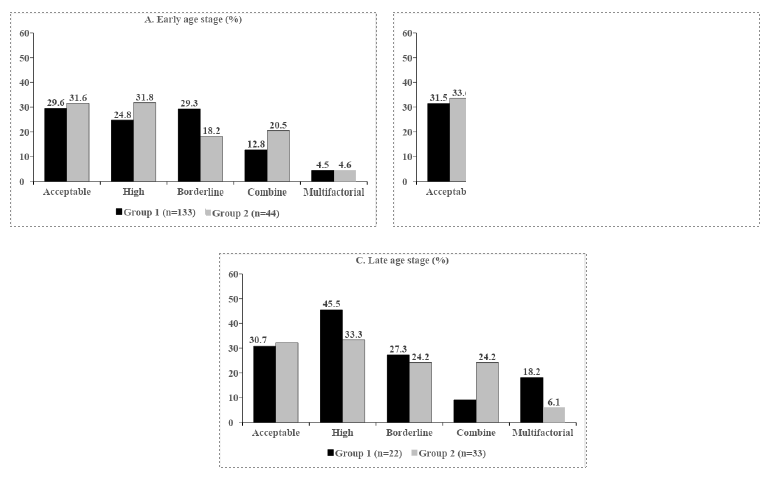
Acceptable concentration of parameters in lipid profile (TC, LDL-C, and TG and HDL-C>40 mg/dL) had 31.6% (n=134) of studied children, which were comparable in group 1 (30.75, n=75) and 2 (32.1%, n=59), P=0.74. The difference in rates of high (30.7% vs. 35.9%, P=0.71), borderline (26.6% vs. 18.3%, P=0.09), and multifactorial (7.0% vs. 3.3%, P=0.09) dyslipidemias did not reach statistical significance. Combined dyslipidemia had 12.9% in group 1 and 21.2% in group 2 (P<0.03). Figure 1 (A, B, C) illustrates the age stage comparison of acceptable, high, borderline, combined, and multifactorial dyslipidemias between groups 1 and 2. The rates of all dyslipidemias were comparable in the early age stage (Figure 1A). Multifactorial dyslipidemia increased in middle age adolescents in group 1 (Figure 1B). Combined data of adolescents in middle and late age stages identified a higher rate of multifactorial dyslipidemia in group 1 than in group 2 (10.0% vs. 2.8%, P<0.02). Regression models showed an increased risk for borderline and multifactorial dyslipidemia in group 1 compared to group 2 (Table 3). Moreover, the risk for high, borderline, combined, and multifactorial dyslipidemias increased with overweight/obesity.
Figure 1. Group-based comparison of prevalence of dyslipidemia based on adolescents’ age stages as early (A), middle (B), and late (C). ***P<0.01; **Each study participant may have more than one abnormality.
| Factors | Dyslipidemia | |||
| High | Borderline | Combine | Multifactorial | |
| Age (years) | 1.09 (0.98, 1.20) | 1.01 (0.91, 1.13) | 1.08 (0.95, 1.24) | 1.19 (0.99, 1.42) |
| Female (1) vs. Male (0) | 1.18 (0.94, 1.49) | 1.2 (0.94, 1.54) | 1.16 (0.86, 1.55) | 1.18 (0.74, 1.87) |
| Overweight/obesity (1) vs. Normal (0) | 1.52** (1.22, 1.93) | 1.31* (1.07, 1.53) | 1.99** (1.48, 2.72) | 1.60** (1.16, 3.35) |
| G1 (1) vs. G2 (0) | 1.14 (0.89, 1.46) | 1.34* (1.01, 1.79) | 0.99 (0.72, 1.37) | 2.14** (1.24, 3.70) |
| Note: *P<0.05; **P<0.01-0.001 | ||||
Table 3. Factors associated with different types of dyslipidemias (OR, 95% CI).
Discussion
In our study, nearly one-third of Asian Indian and Hispanic adolescents in each age stage had an acceptable serum concentration for all lipid tests, which is lower than the nearly 50% rate of ideal lipid levels identified in White, Black, and Mexican US youth in the 1999-2016 National Health and Nutrition Examination Survey (NHANES). We recorded no difference in borderline and high dyslipidemias proportions across age stages in Asian Indian and Hispanic adolescents. The overall frequency of multifactorial dyslipidemia in Asian Indian adolescents was 2-fold higher than in Hispanics, who had a comparable rate to 5% of the national estimate. The increased likelihood for the development of multifactorial dyslipidemia in Asian Indians was independent of adolescents’ age, gender, and overweight/obesity. No other studies categorized multifactorial dyslipidemia in the pediatric population but provide the rates of abnormal LDL-C or TC levels. Such as, surveillance of lipid levels during well-child visits conducted more than 30 years ago identified 8.5% of children with TC levels of more than 200 mg/dl [17].The NHANES (1999-2006) showed elevated LDL-C in up to 6.6% and TC in 10.7% of 12-17 years old adolescents in the U.S., more likely among black than white participants [18].
In the present study, overweight/obesity predicted all types of dyslipidemias, irrespective of ethnicity, gender, and age. The most common components of lipid measurements related to overweight/obesity are high TG and low HDL [19,20]. The rate of combined dyslipidemia defined by a TG/HDL-C ratio of 3 or more was also more likely prevalent in overweight/ obese than in average weight Hispanic (26.9% vs. 13.8%, P<0.04) and Asian Indian (23.6% vs. 6.6%, P<0.001) adolescents. Studies highlighted the importance of increased TG/HDL-C ratio as a metabolic marker of insulin resistance in the adult population, including Hispanic men and women. The negative role of overweight/obesity has also been highlighted in developing a multifactorial type of dyslipidemia. In our study, the rates of multifactorial dyslipidemia in Hispanic adolescents with and without overweight/obesity were comparable (3.9% vs. 2.5%, P=0.86) but increased in Asian Indians with abnormal BMI (12.1% i. 4.0%, P<0.02). Possible genetic variations with incomplete penetrance and dietary practice differences that restrict consumption of polyunsaturated fatty acids could contribute to dissimilarity in magnitude of BMI abnormality in multifactorial dyslipidemia occurrence between Hispanic and Asian Indian adolescents in our study. Because of the significant role of abnormal LDL-C in atherogenesis and the development of CV diseases, more data will be needed to assess the cultural variation in the association of overweight/obesity with multifactorial Mehrotra/Mehrotra/Petrova/ References dyslipidemia. Unfortunately, the longitudinal study did not account for race/ethnicity and BMI while reporting the predictive value of elevated LDL-C in childhood for the LDL C abnormality 15-20 years later. The US Preventive Services Task Force identified the insufficiency of existing evidence to support direct benefits of screening for multifactorial dyslipidemia during childhood. However, strategies to prevent CV diseases in adults should be initiated in childhood. Therefore, further studies will be needed to understand the modifiable risk factors for the development of dyslipidemias in a culturally diverse population of American adolescents.
We recognize the limitations of our study. The study used data from universal lipid screening performed for Asian Indian and Hispanic children at two locations of a single pediatric practice, which could limit the external validity of obtained findings. Moreover, the generalizability of study results could be restricted by the homogeneity of health insurance coverage of Hispanic (government based) and Asian Indian (commercial) adolescents that, by proxy, characterized the difference in the socioeconomic status of adolescents' families. In addition, the racial diversity of adolescents of Hispanic ethnicity and dietary intake, which is one of the critical correlates of dyslipidemia, have not been accounted for.
Conclusion
Universal lipid screening identified acceptable levels of all of the tested lipid parameters in only one-third of adolescents of either Asian Indian or Hispanic origin, irrespective of their age stage. Asian Indian are at higher than Hispanic adolescents risk for development of multifactorial but comparable for combined type of dyslipidemia, which risk was found to be associated with being overweight/obese in both ethnic groups of studied children. We believe that large multicenter studies and extensive dietary surveys will be needed to identify ethnicity related behavior factors in alteration of lipid profiles in the culturally diverse pediatric population.
Ethical Consideration
This research study maintained the rules for ethical compliance. There was no external source of funding used to conduct the research. The authors declare that they have no conflict of interest. Informed consent was not needed for retrospective data collection. This study was conducted in accordance with the 1964 declaration of Helsinki and its subsequent amendments and was approved by the IRB at Saint Peter's University Hospital in New Jersey.
Acknowledgments
The authors would like to acknowledge all of the adolescents who underwent lipid screening in the pediatric practice.
References
- Pu J, Romanelli R, Zhao B, et al. Dyslipidemia in special ethnic populations. Endocrinol Metab Clin North Am. 2016;45(1):205-16.
[Crossref] [Google Scholar] [PubMed]
- Frank ATH, Zhao B, Jose PO, et al. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129(5):570-9.
[Crossref] [Google Scholar] [PubMed]
- Singh V, Deedwania P. Dyslipidemia in special populations: Asian Indians, African Americans, and Hispanics. Curr Atheroscler Rep. 2006;8(1):32-40.
[Crossref] [Google Scholar] [PubMed]
- Hong YM. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ J 2010;40(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Kit BK, Carroll MD, Lacher DA, et al. Trends in serum lipids among US youths aged 6 to 19 years, 1988-2010. JAMA. 2012;308(6):591-600.
[Crossref] [Google Scholar] [PubMed]
- Perak AM, Ning H, Kit BK, et al. Trends in levels of lipids and Apolipoprotein B in US youths aged 6 to 19 years, 1999-2016. JAMA. 2019;321(19):1895.
[Crossref] [Google Scholar] [PubMed]
- Kit BK, Kuklina E, Carroll MD, et al. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 2015;169(3):272-9.
[Crossref] [Google Scholar] [PubMed]
- Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586-613.
[Crossref] [Google Scholar] [PubMed]
- Steinberger J, Daniels SR, Hagberg N, et al. Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation. 2016;134(12):e236-55.
[Crossref] [Google Scholar] [PubMed]
- Lozano P, Henrikson NB, Morrison CC, et al. Lipid screening in childhood and adolescence for detection of multifactorial dyslipidemia: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316(6):634-44.
[Crossref] [Google Scholar] [PubMed]
- Rodriguez CJ, Daviglus ML, Swett K, et al. Dyslipidemia patterns among Hispanics/Latinos of diverse background in the United States. Am J Med. 2014;127(12):1186-94.
[Crossref] [Google Scholar] [PubMed]
- FOR EP, CHILDREN RR. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213.
- de Ferranti SD, Rodday AM, Parsons SK, et al. Cholesterol screening and treatment practices and preferences: a survey of United States pediatricians. J Pediatr. 2017;185:99-105.
[Crossref] [Google Scholar] [PubMed]
- Margolis KL, Greenspan LC, Trower NK, et al. Lipid screening in children and adolescents in community practice: 2007 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7(5):718-26.
[Crossref] [Google Scholar] [PubMed]
- Elmaogullari S, Tepe D, Ucakturk SA, et al. Prevalence of dyslipidemia and associated factors in obese children and adolescents. J Clin Res Pediatr Endocrinol. 2015;7(3):228-34.
[Crossref] [Google Scholar] [PubMed]
- Mehrotra N, Mehrotra N, Petrova A. Prevalence and factors associated with dyslipidemia in otherwise healthy Asian Indian American Adolescents. Int J Child Adolesc Health. 2021;14(3):253-60.
- Garcia RE, Moodie DS. Routine cholesterol surveillance in childhood. Pediatrics. 1989;84(5):751-5.
[Google Scholar] [PubMed]
- Ford ES, Li C, Zhao G, et al. Concentrations of low-density lipoprotein cholesterol and total cholesterol among children and adolescents in the United States. Circulation. 2009;119(8):1108-15.
[Crossref] [Google Scholar] [PubMed]
- Parray IA, Parry MA, Latief M. Prevalence of dyslipidemia in school children of Kashmir valley. Diabetes Metab Syndr. 2016;10(2):S47-54.
[Crossref] [Google Scholar] [PubMed]
- Kwiterovich Jr PO. Recognition and management of dyslipidemia in children and adolescents. J Clin Endocrinol Metab. 2008;93(11):4200-9.
[Crossref] [Google Scholar] [PubMed]