Research Article - Archives of General Internal Medicine (2023) Volume 7, Issue 4
Demographic and clinical features of snakebites among adults in Mukalla, Hadhramout
Ahmed Mubarak Daakeek*Department of Medical, Faculty of medicine and health sciences, Hadhramout University, Mukalla, Yemen
- *Corresponding Author:
- Ahmed Mubarak Daakeek
Department of Medical
Faculty of medicine and health sciences
Hadhramout University, Mukalla, Yemen
E-mail: daakeek@gmail.com
Received: 25-Jul-2023, Manuscript No. AAAGIM-23-110705; Editor assigned: 28-Jul-2023, PreQC No. AAAGIM-23-110705(PQ); Reviewed: 11-Aug-2023, QC No. AAAGIM-23-110705; Revised: 16-Aug-2023, Manuscript No. AAAGIM-23-110705(R); Published: 23-Aug-2023, DOI:10.35841/aaagim-7.4.185
Citation: Daakeek AM. Demographic and clinical features of snakebites among adults in Mukalla, Hadhramout. Arch Gen Intern Med. 2023;7(4):185
Abstract
Background: Snakebite is a common medical emergency and an occupational hazard. The available data on the epidemiology of snakebite in the Hadhramout are sparse. It is a neglected disease afflicts the most impoverished inhabitants of the rural areas in the tropical countries. Objectives: To study demographic characteristics, clinical manifestations, severity, and management of snakebite patients admitted to Ibn-Sina general hospital in Mukalla, Hadhramout. Methods: This retrospective study includes sixty-four of snakebite patients admitting in Ibn Sina general hospital from January 2022 to December 2022. The data included were demographic factors, clinical features, complication, severity grading, treatment and the outcome. Age is further sub grouped into decades and severity classify into three grades mild, moderate and severe envenomation. Results: The majority of patients were male (79.7% versus 20.3%), and the average age was 28.8 SD14.233 years. 15–35-year-olds are the most frequently affected age group (84.4%). 75% of the cases were located in Hadhramout coastal rural areas, 50% of which were in Mukalla rural areas. A bite is most frequently observed from April to September (76.5%). 51.6% of patients arrive at the hospital within 5 hours, and 68.8% stay for 2 days. The lower leg (71.9%) was the most frequently seen area of the bite. The severity of the illness and delay in hospital presentation were significantly correlated (p value = 0.00). Common presentations were local pain (97%), redness (62.5%), and swelling (60.9%), while bleeding, renal, and neurological manifestations are uncommon. No fatal cases have been reported, and 57.8% of cases are classified as mild envenomation. In all cases, the type of snake is unidentified. Anti-snake venom was administered in varying doses in almost all cases. Conclusion: Snakebite is a common occurrence in Hadhramout’s rural areas among adolescent males, which is similar to what has been observed in Southeast Asian and Arab countries, although there is little knowledge of the snake species there and no treatment guidelines. Public health education and efficient healthcare worker training are essential.
Keywords
Snakebites, Envenomenation, Hadhramout.
Introduction
Venomous snakebite is a significant cause of morbidity and mortality in many countries in worlds especially in South-East Asia and sub-Saharan Africa, mainly in the rural hinterlands where facilities are lacking, it is most often an occupational, domestic or environmental hazard [1].
The estimated number of snakebites worldwide has been put as 5.4 million, resulting in 2.5 million envenomation and 20,000 to 94,000 deaths annually [2-4]. M´edecins Sans Frontières (MSF) routine reports revealed that 6469 patients were admitted in 2019 throughout all of its projects in 17 countries. South Sudan, Ethiopia, the Central African Republic, and our country were the four countries most severely impacted by humanitarian crises, and several hospitals there saw more than 1,000 annual admissions.
Snakebite was re-designated as a Neglected Tropical Disease (NTD) in 2017, which was removed from the list in 2013, and in 2019, it released a strategic road map focused on halving disability and mortality by 2030. Reconsidering the problem of snakebite in developing and tropical countries, which contributes 95 per cent of the total snakebites of the world, it was re-designated as a Category A of the NTD by the WHO with the hope that this declaration would provide an ample opportunity to attract investment and research funding for further improvement of snakebite management in developing countries. One of the major reasons cited for snakebite being removed off the NTD list was that there were not enough data from developing countries [5].
Snake bite is one of the most important NTDs in terms of both incidence and severity, and its clinical characteristics readily served as a basis for advocacy. Snakebites disproportionately involve the poorest the poor, mostly in rural areas. Although very expensive, provision of treatment for the majority of cases does bring sustainable profit to manufacturers – and this the main reason for the current antivenom shortage [6].
Venomous snake bites can present with local symptoms like pain, swelling, redness, or local infections like cellulitis and compartment syndrome or systemic symptoms like neurological, haematological, myotoxic, organ failure, and some other nonspecific symptoms.The victim of a snake bite suffers a frightening experience[7].
There are eight species of dangerous poisonous snakes in Yemen. They include all members of the families: Atractaspididae, Elapidae and Viperidae. Arabian (Egyptian) cobra (naja haje arabica) from elapidae family, and Puff adder (Bitis arietans), Burton's carpets viber (Echis coloratus), Saw scalded viber (Echis pyramidum), and Sand viper or horned viber (cerastes gaspereitti) from viperidae are common in Hadhramout [8].
Snakebites are a neglected emergency in Yemen, due to low public awareness of snakebites and a lack of attention from the health ministry and no governmental policy. As a result, the purpose of this study is to emphasize the demographic and clinical characteristics, as well as the severity assessment and management of snake bites in Hadhramuot, particularly in Mukalla and coastal regions where this study was conducted.
Materials and Methods
This one-year retrospective study was conducted from January to December 2022 at Ibn-Sina General Hospital in Mukalla city, capital of Hadhramout Governorate, Yemen. Approximately 3000,000 inhabitants are served by this hospital, a referral and larger hospital in the eastern governments of the country.
The medical files of adult snakebite victims admitted to the department of internal medicine were recognized and recorded in the statistics department. The patient's selection criteria were based on the final diagnosis of snake bite in medical records. Every other insect bite or uncertain bite in which the victims did not observe the snake during the bite or could not be proven as a snake bite was excluded from the study.
The files were examined for demographic criteria such as age, gender, residence, and month of bite. The review includes clinical profiles such as symptoms, bite site, period of hospitalization, and treatment offered in the hospital, particularly polyvalent anti-snake venom, which was used to manage the majority of the patients. The investigation was not located in almost all cases documented, thus we had to rely on what the treating physician noted in the files.
Age further divide by decades to three groups: 15-35 year, 36-55 years, and more than 55-year groups. According to the patient condition at the time of admission, we classified as follows: mild envenomation include pain and mild swelling and redness without systemic manifestation, moderate envenomation include local swelling and or redness extended beyond joint, systemic manifestations and local bleeding or mild neurological affection or nephrological involvement, and severe envenomation include severe swelling, shock, systemic bleeding, bulbar or respiratory paralysis and renal failure.
Statistical Package for the Social Sciences Software (SPSS) Mac version 23.0 and Excel Microsoft 13 were used for all statically analysis. The frequencies of different categorical variables were calculated. The median and range were calculated for continuous variables. Patient characteristics were compared using the Chi-square test or Fisher’s exact test for categorical variables.
Results
We report 70 patients with snake envenomation presented to Ibn Sina general Hospital in Mukall between January and December 2022. Six patients were excluded due to unconfirmed bites. The total number of patients underwent this study were 64 patents.
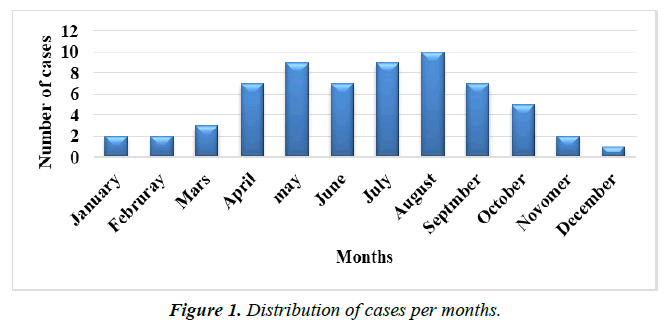
The demographics of the cases are displayed in Table 1. The mean patient age was 28.8 (14.233) years old. The age group of 15 to 35 years was where the majority of snakebite cases were reported. They comprised 84.4% of all reported snakebites, in contrast to substantially lower numbers for other age groups. The male to female ratio was 3.9:1, with male cases greater than female cases (79.7 and 20.3%, respectively), in the most common age group (15-35 years) and equally in the 36-55 years group. There were no female cases in the age group above 55 years. The majority of patients (75%) came from rural areas of Mukalla city and coastal regions of Hadhramout governorates. The hottest months of the year, from April to September, saw the majority of envenoming (76.5%). The monthly number of cases is depicted in Figure 1, with August having the maximum.
| Variable | Number | % | |
|---|---|---|---|
| Age | Range | 15-71 year | |
| Mean &SD | 28.8 (±14.233) | ||
| Age groups | 15-35 years | 54 | 84.40% |
| 36-55 years | 4 | 6.30% | |
| >55 years | 6 | 9.40% | |
| Sex | Male | 51 | 79.70% |
| Female | 13 | 20.30% | |
| ratio | 3.9:1 | ||
| Residence | Mukall city | 12 | 18.80% |
| Mukalla rural areas | 32 | 50% | |
| Hadhramout coastal rural areas | 16 | 25% | |
| Shabowa | 3 | 4.70% | |
| Other area | 1 | 1.60% | |
| Month of bite | January- Mars | 7 | 10.90% |
| April – June | 23 | 35.90% | |
| July- September | 26 | 40.60% | |
| October- December | 8 | 12.50% |
Table 1. Demographic characters of snakebite cases studied in Hadhramout.
Table 2 shows that lower limbs were the most frequently bitten areas in 46 cases (71.9%). The average amount of time from the bite to hospital attendance was (8.086, SD 6.521), with 48.4% of patients arriving within 1 to 5 hours and 51.6% after 5 hours. Arrival delays are associated with serious snakebite complications like hematological, neurological and renal damages (p value = 0.00). The average duration of hospital stay for patients (68.8%) was 2 days or less. The longest stay involved three patients, who were admitted for a week. In almost all cases, the type of snake was not identified.
| Items | Number | % | |
|---|---|---|---|
| Site of bite | Lower limb | 46 | 71.9 |
| Upper limb | 18 | 28.1 | |
| Time between bite and admission | 0-5 hours | 31 | 4840.00% |
| 6-12 hours | 20 | 3130.00% | |
| 13-24 hours | 11 | 1720.00% | |
| > 24 hours | 2 | 310.00% | |
| Hospital duration | 1-2 days | 44 | 6880.00% |
| 3-4 days | 11 | 17.2 | |
| 5-7 days | 9 | 1410.00% | |
| Type of snake | Not identified | ||
Table 2. Character of snakebite in cases.
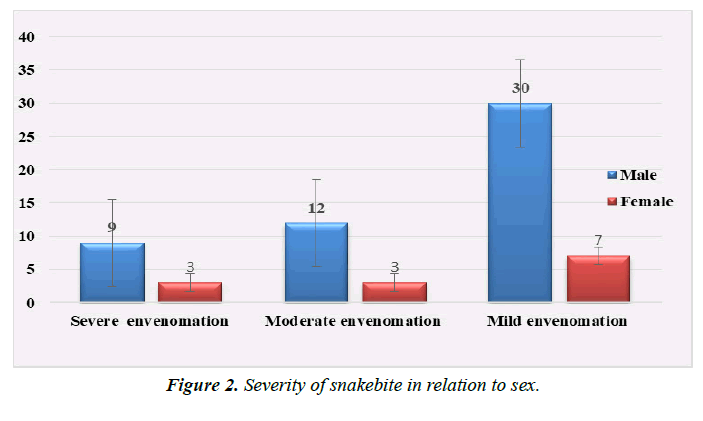
The majority of patients had mild envenomation (57.8%), followed by moderate envenomation (23.4%), and severe envenomation (18.75%) (Figure 2) . All patients survived and were discharged from the hospital in good condition.
Clinical symptoms of snake bites are shown in Table 3. Localized pain, redness, and swollen were the most frequent symptoms in (97%, 62.5%, and 60.9%, respectively). Less frequently, the neurological, renal, and hematological systems are affected. 16 (25%) patients had bite marks.
| Symptoms | Number | % | |
|---|---|---|---|
| Local pain | 62 | 97 | |
| Local Redness | 40 | 62.5 | |
| local swelling | 39 | 60.9 | |
| General weakness | 36 | 56.2 | |
| Nausea &Vomiting | 35 | 54.7 | |
| Dizziness | 31 | 48.4 | |
| Renal affection | 17 | 26.6 | |
| Bite mark | 16 | 25 | |
| Ptosis & Diplopia | 12 | 18.8 | |
| Bleeding | Local | 8 | 12.5 |
| Systemic | 6 | 940.00% | |
| Cellulitis | 8 | 1250.00% | |
| Shock | 8 | 1250.00% | |
| Ischemia | 3 | 470.00% |
Table 3. Symptoms of snake bite case.
Before going to the hospital, the majority of cases are treated using traditional means. The data shows that 51 patients (79.7%) received a tourniquet, 11 patients (17.2%) had incisions, and 5 patients (708%) had the venom suctioned from the bite site.
According to the medical records, investigations were requested for the following tests: complete blood count (CBC), renal function test, blood sugar, liver function test, prothrombin and activated partial thromboplastin time, chest x-ray, ECG, and urine analysis. Vital signs charts and the usual assessment of urine output have been recommended. The 20-minute whole blood clot was not done. The patient's medical records did not contain the investigation results.
Antibiotics, Tetanus antitoxin, and steroids were administered to all patients. In 63 cases (98.4%), polyvalent snake antivenom was administered. As there is no specific protocol for the patients in the hospital or the country as a whole, the dose of antivenom varies depending on the attending physician and the severity of the condition. The dose usually includes two to eight vials.
Discussion
In Yemen, there are several venomous snakes. Eight of the 54 species of snakes that have been recognized are venomous snakes [8]. Data on snake bites in Hadhramout and Yemen in general are scarce.
The Ibn Sina general hospital received 64 cases of snakebite envenomation during the course of a year, from January to December 2022, according to this study. This figure per year is larger than what was noted in research from Yemen's Hajja and Sadda [9, 10], as well as from Oman [11], Saudi Arabia [12, 13], Egypt [14], Jordan [15, 16], and Malaysia [17], but it is lower than what was observed in studies from the Saudi province of Riyadh [18], Kenya [19], and India [20]. Hadhramout's extensive land area, which includes both desert and agricultural areas, may help to explain the greater prevalence of snakebites. Additionally, the climate, which was extremely hot in the majority of the years, created a neutral environment for the spread of snakes.
The majority of study individuals were men (M:F ratio 3.9:1), which was similar to studies conducted in our country and some Arab countries, such as Haiiah Yemen where men make up 73.7%, Oman where men outnumber women 9:1, Saudi Arabia's Riyadh province where men outnumber women 81.70%, Egypt where men make up 85.7%, Jordan where men outnumber women 3.2:1, and Morocco where men make up 53% [21]. The majority of countries, including Bangladesh, Malaysia, Kenya, and India, saw the same result. The fact that males often engage in outside activities like farming while women spend the majority of their time indoors with their families.
The current finding showed that young adults and adolescents (84.4%) are more susceptible to snakebites. The majority of research in our country as well as in Oman, Jordan, Egypt, Saudi Arabia, Morocco, Bangladesh, Malaysia, Kenya, and India, all came to the same conclusion. Given that this age group is connected with the majority of activities performed outside of the home, the high risk of snakebites among individuals under the age of 35 may be explained.
According to our study, most snake bites were reported from April to September which were hottest months in Hadhramout with a maximum frequency in August, while the winter months (November through Mars) there were a limited cases. This may be because snakes hibernate and become very inactive due to lowered ambient temperatures. This result corroborates some studies in other regions of yemen (Hajja) and other countries like Oman, Saudi Arabia, Egypt, Jordan Morocco, Bangladesh India, Malaysia, and in Kenya, but differs from other studies in Gabon [22] , and in Brazil [23] in which snake bites were reported between November and April.
As the consequence of working without footwear and the fact that the exposed limbs are typically used in the majority of manual tasks, the present study has shown that the bite more frequently impacted the lower limbs. The results of this study are consistent with those from Oman, Egypt, Malaysia, Saudi Arabia, Kenya, and India.
As was to be expected, we discovered that the majority of cases in this study came from rural areas near Mukala city and other coastal Hadhramout regions, which are located far from urban centers and where there are deserts and agricultural areas (Hadramout is primarily composed of desert areas), as well as high temperatures, which are ideal settings for snake presence and reproduction, this finding has also been reported by other studies conducted in Oman [24] Saudi Arabia [25], Egypt and Morocco.
About (48.4%) of the patients reported to hospital, within1-5 hours of snakebite. (51.6%) of cases had delayed presentation may because they from a far place or the lack of transportation or they went for traditional therapy before they came to the hospital. This delay has strong correlation statically with severe manifestation (p value 000). Similar finding seen also in Saada Yemen study and low percent than our study 38.8% delay in reach hospital in India.
In every occurrence of snakebite, the snakes were never identified. This is due to the lack of information about snakes among the general public, physicians, and healthcare workers, as well as the lack of information regarding snake spices in medical records. In our country and governorate, there is a complete lack of instruction, written materials, or images of common dangerous snakes.
In the current study, the most frequent clinical manifestations were pain (97%), redness and swelling at the bite site (62.5%, 60.9%). This conclusion is larger compared to the findings in Saada and Hajjah in Yemen and in Egypt, where swelling and pain have a smaller percentage. It is also relatively similar to a study that took place in Oman. Snakebite can typically be identified by the presence of fang marks, although this mark was only present in 25% of cases, which is greater than the Hajja study's and lower than Oman's findings.
In addition to these local symptoms, bleeding, whether local or systemic, accounts for 21.9% and renal disease for approximately 26.6%. This conclusion is higher than those of the studies conducted in Hajja, Yemen, Egypt and Oman, but lower than those from India. Ptosis was discovered in (18.8%), a value that was higher than that in Hajja and lower than that observed in Bangladesh, Egypt and India, as well as in Oman, where there were no cases documented.
In our study, most patients (68.8%) spent no more than two days in the hospital. Researchers observed a similar pattern in Hajja and Kuala Lumpur, Malaysia, with slightly higher durations in Oman. The maximum hospital stay is 7 days, and it depends on the severity and complications of the illness, the outcomes of the laboratory investigation, and other factors. The majority of patients had mild (57.8%) versus moderate or severe envenomation. As opposed to Morocco study, where moderate envenomed is more common, and Egypt study where 57.1% are severe envenomed. This may be attributed to dry bites from snakes and early hospital admissions in a number of cases, as delays in Anti-Snake Venom (ASV) administration increase the risk of severity, complications, and mortality.
A Complete Blood Count (CBC), renal function test, Prothrombin Time (PT), and Partial Thromboplastin Time (PTT) are among the investigations that are typically asked to identify bleeding tendencies and screen for Disseminated Intravascular Coagulation (DIC). Because the investigations were not found in the patients' medical records, perhaps because they were given to patients upon discharge, this study has limited ability to evaluate the cases paraclinically. Due to a lack of knowledge, the 20-minute whole blood clotting test (20WBCT), which is easy to perform and extremely helpful and informative, was not performed in our institution.
Nearly all cases (63, 98.4%) had anti-snake venom administered. Since the antivenom should only be administered to patients in whom it is believed that the benefits will likely outweigh the risks, this practice is not supported by evidence. Antivenom shouldn't be used carelessly because it is frequently in limited supply and is relatively expensive. All of the cases were given a subcutaneous test dose of antivenom, which is not generally advised in such circumstances because antivenom reactions are caused by direct dose-related complement activation rather than by indirect dosage-related IgE-mediated hypersensitivity, and these tests are not reliable. This practice at our hospital might be a result of malpractice.
Prior to receiving antivenom in our study, there was no premedication with adrenaline. Prior to antivenom therapy, it is generally advised to take prophylactic adrenaline, with the exception of elderly patients who have an underlying cerebrovascular disease, and where the specific antivenom being used has a documented low incidence of reactions (5%), [26, 27].
Four vials were the median dose of anti-snake venom. This dose of ASV does not depend on the type of snake or the severity of the bite; rather, it is routine in hospitals in the lack of national or regional guidelines, protocols, or policies for the administration of ASV and snakebites management in general.
In all cases, tetanus antitoxin and prophylactic antibiotics were administered. Although there has been no confirmation of local or systemic infections, routine prophylactic use of antibiotics is frequent in our hospital. However, according to WHO guidelines, this practice is not routinely recommended for the therapy of snakebite. This because there is no clear policy about the exact role of antibiotics in the treatment of snakebite.
This study has various limitations, the first of which is that it is a retrospective study. There is a lot of unfounded and unstudied data, like laboratory parameters that were overlooked because they didn't exist in patient records or collected from them. The identification of the snakes wasn't carried out and wasn't documented in the medical records, which was the second limitation. Finally, this study only includes the coastal regions of the Hadhramout Governorate. Future research must take into account other regions of the governorate, particularly a Hadhramout valley, which has a larger area of desert and several farms.
Conclusion
This is, as far as we are aware, the first study on snake bites in Hadhramout. This study comes to the conclusion that snakebites are among the neglected diseases in Yemen, spreading in rural and urban areas along the Hadhramout coast, especially in young men between the ages of 15 and 35. They also spread during the hot months of April to September and may cause complications in the hematological, renal, and neurological systems.
Lack of scientific and practical training for health care providers and physicians about snake species and how to deal and treat the venomous snakebites results in insufficient and inadequate medical treatment that is recommended in such cases. Additionally, there is no management policy that has been approved by the official health authorities.
In addition to educating the public about poisonous snakes, particularly the high-risk population in regions where bites are common, we advised instituting training programs, educational programs, and practical health policies. After learning about the various types of venomous snakes in the whole country, the government should also act quickly to assure the ongoing availability of the proper sort of antivenom.
References
- Chakma JK, Menon JC, Dhaliwal RS. White paper on venomous snakebite in India. Indian J Med Res. 2020;152(6):568.
- Chippaux JP. Estimating the global burden of snakebite can help to improve management. PLoS Med. 2008;5(11):e221.
- Kasturiratne A, Wickremasinghe AR, de Silva N, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5(11):e218.
- Alcoba G, Potet J, Vatrinet R, et al. Snakebite envenoming in humanitarian crises and migration: a scoping review and the Médecins Sans Frontières experience. Toxicon: X. 2022;13:100089.
- Chippaux JP. Snakebite envenomation turns again into a neglected tropical disease!. J Venom Anim Toxins Incl Trop Dis. 2017;23.
- Chippaux JP, Massougbodji A, Diouf A, et al. Snake bites and antivenom shortage in Africa. Lancet. 2015;386(10010):2252-3.
- Miah MT, Hoque AA, Tarafder BK, et al. Epidemiology, clinical profile and outcome of patients of snake bite in Mymensingh Medical College Hospital. J Bangladesh Coll Phys Surg. 2009;27(2):70-5.
- Busais S.M.,Al-Jumaily M.M, A contribution to the Herpetofauna of Yemen: Distribution study of dangerous snakes in Yemen. J Appl Nat Sci.2005.9:(3).
- Haidar NA, Emran MY, Al Muslemani EA. Snakebites in Hajjah, Yemen Republic: Epidemiology, management and the relation of the degree of acuity at presentation with outcome. J Emerg Med Trauma Acute Care. 2012;2012(1):2.
- Abohassan AM, Borham MM, Barshomy S. Snake bite: clinical presentation, complication and outcome in relation to time of polyvalent snake antivenin in Yemen. J Egypt Soc Parasitol. 2012;240(1411):1-8.
- Al-Lawati A, Al-Abri SS, Lalloo DG. Epidemiology and outcome of snake bite cases evaluated at a Tertiary Care Hospital in Oman. J Infect Public Health. 2009;2(4):167-70.
- Al Harbi N. Epidemiological and clinical differences of snake bites among children and adults in south western Saudi Arabia. J Emerg Med. 1999;16(6):428-30.
- Malik GM. Snake bites in adults from the Asir region of southern Saudi Arabia. Am J Trop. Med Hyg. 1995;52(4):314-7.
- Saleh AA. Clinical profile and outcomes of snakebite envenomation in fayoum governorate, Egypt. Egypt J Forensic Appl. Toxicol. 2023;23(1):79-92.
- Baker MA, Al-Saraireh M, Amr Z, et al. Snakebites in Jordan: A clinical and epidemiological study. Toxicon. 2022;208:18-30.
- Maid TA J, Faris K. Snake bites, scorpion and insect stings in Balqa: An epidemiological study.
- Jamaiah I, Rohela M, Ng TK, et al. Retrospective prevalence of snakebites from Hospital Kuala Lumpur (HKL)(1999-2003). Southeast Asian J Trop Med Public Health. 2006;37(1):200.
- Al-Sadoon MK. Snake bite envenomation in Riyadh province of Saudi Arabia over the period (2005–2010). Saudi J Biol Sci. 2015;22(2):198-203.
- Ochola FO, Okumu MO, Muchemi GM, et al. Epidemiology of snake bites in selected areas of Kenya. Pan Afr Med J. 2018;29(1):1-4.
- Halesha BR, Harshavardhan L, Channaveerappa PK, et al. A study on the clinico-epidemiological profile and the outcome of snake bite victims in a tertiary care centre in southern India. J Clin Diagnostic Res. 2013;7(1):122.
- Arfaoui A, Hmimou R, Ouammi L, et al. Epidemiological profile of snakebites in Morocco. J Venom Anim Toxins Incl Trop Dis. 2009;15:653-66.
- Tchoua R, Raouf AO, Ogandaga A, et al. Analysis of snake bite envenomations in Gabon. Bull Soc Pathol Exot. 2002;95(3):188-90.
- Pacheco UP, Zortéa M. Snakebites in southwestern Goiás state, Brazil. J Venom Anim Toxins Incl Trop Dis. 2008;14:141-51.
- Khan YM, Fatema N, Shekeili NA. Snake bite envenomation: experience in a regional hospital, Oman: a retrospective observational study. SM Trop Med J. 2017;2(1):1015.
- Al-Sadoon MK, Albeshr MF, Paray BA, et al. Envenomation and the bite rate by venomous snakes in the kingdom of Saudi Arabia over the period (2015–2018). Saudi J Biol Sci. 2021;28(1):582-6.
- World Health Organization. Guidelines for the management of snakebites. World Health Organization(2016).79-80.
- Premawardhena AP, De Silva CE, Fonseka MM, et al. Low dose subcutaneous adrenaline to prevent acute adverse reactions to antivenom serum in people bitten by snakes: randomised, placebo controlled trial. Br Med J. 1999;318(7190):1041-3.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref