Research Article - Current Pediatric Research (2018) Volume 22, Issue 1
Clinical presentations, glycemic control, complications, and associated autoimmune diseases among children and adolescents with type 1 diabetes in the western region of Saudi Arabia.
Sarah M Alshawi, Abdulmoein E Al-Agha, Ghadah A Althibiti, Amjaad M Almotairi, Marwa Z Rambo*, Maram K Alnabulsi, Yam O IsmaielPediatric Endocrinology, Pediatric Department, Faculty of Medicine, King Abdulaziz University Hospital, Saudi Arabia.
- Corresponding Author:
- Marwa Z Rambo
Pediatric Endocrinology
Pediatric Department, Faculty of Medicine
King Abdulaziz University Hospital, Saudi Arabia
Tel: +966 50 559 0459
E-mail: marwa.rambo@hotmail.com
Accepted date: January 27th, 2018
Abstract
Objective: To study the correlation between initial presentation, metabolic control, longterm complication and the concomitant autoimmune diseases. In addition to exploring the various risk factors that can impact the glycemic control in children and adolescents with type 1 diabetes (T1DM). Methods: A retrospective cross-sectional study was conducted on 461 patients including children and adolescents with T1DM, who were followed up at the pediatric clinic at King Abdul-Aziz University Hospital from January 2004 to December 2016. The medical records and laboratory findings in the hospital’s electronic system of all patients were reviewed. Collected data comprised of the primary disease presentation including hyperglycemic and diabetic ketoacidosis (DKA) symptoms, associated autoimmune diseases and consequent chronic complications. Results: The mean patient age was 10.4 ± 4.8 years. A total of 62.1% and 27.9% initially presented with hyperglycemia and DKA, respectively. Glycemic control did not significantly differ between the pubertal and the pre-pubertal groups, although the glycated hemoglobin A1c levels were higher in the pre-pubertal group (62.3%) than in the pubertal group (37.7%). Chronic complications were observed as follows: steatohepatitis (11.1%), microalbuminuria (11%), dyslipidemia (10.3%) and retinopathy (5.7%). Regarding the associated comorbidities, vitamin D deficiency was present in 58.9% of children and was significantly associated with gender (68.4% females and 51.9% males), whereas autoimmune thyroiditis and celiac disease were present in 20% and 8.2% of children, respectively. Conclusion: Pre-pubertal children exhibited less glycemic control as compared to adolescents. The most common presentation at diagnosis included signs of hyperglycemia rather than those of DKA. The co-morbidities showed a significant relationship with gender. Vitamin D deficiency is the most common associated medical condition in children with diabetes.
Keywords
Diabetes mellitus, Presentation, Associations, Complications.
Introduction
Type 1 diabetes mellitus (T1DM) is considered to be one of the most common endocrine diseases in children. Approximately 50% of patients with T1DM are diagnosed during the first 15 years of their lives [1]. The incidence rate of T1DM is gradually increasing, with a prevalence of 109.5 per 100,000, among both children and adolescents in Saudi Arabia [2,3]. Based on the recent report in 2013 by the International Diabetes Federation, Saudi Arabia was among the top 10 countries in terms of diabetes prevalence with a percentage of 24 [4].
The most common initial presentations of T1DM include hyperglycemic symptoms or acute diabetic ketoacidosis (DKA). Hyperglycemic symptoms include polyuria, polydipsia, weight loss, nocturia, nocturnal enuresis and glycosuria, whereas acute DKA symptoms include abdominal pain, vomiting, ketone smell, ketonuria, Kussmaul breathing, and confusion [5]. Children with T1DM are at a high risk of developing autoimmune diseases and other chronic complications. In fact, studies have shown that children with diabetes could develop other autoimmune diseases such as autoimmune thyroiditis (AIT) and celiac disease (CD) [6,7]. In addition, studies also showed an association between T1DM and vitamin D deficiency. Moreover, chronic complications, including retinopathy, nephropathy, dyslipidemia and liver disease, are reported to be the most common chronic complications in pediatric patients with T1DM [8]. Several factors contribute to the progression of diabetes complications, including diabetes duration, age, pubertal stage, and glycemic control [9]. Improved glycemic control in children and adolescents with T1DM helps to reduce and even prevent potential chronic complications [10-12]. Such good glycemic control can be achieved via frequent home monitoring of blood glucose levels and regular daily insulin injections, or via insulin pump use. Furthermore, patients are recommended to follow up with regular HbA1c tests, healthy diet, and routine physical exercise. Moreover, intensified insulin therapy has been shown to enhance glycemic control and thus reduces diabetic complications to a greater extent, as compared to conventional insulin therapy [13].
In this study, we intend to evaluate the interrelationship linking the initial presentation, metabolic control, longterm complication and the accompanying autoimmune diseases. Additionally, to investigate the various risk factors that can influence the glycemic control in children and adolescents with type 1 diabetes (T1DM), who visited the pediatric endocrine clinic at King Abdul-Aziz University Hospital (KAUH) in Jeddah, Saudi Arabia.
Methods
This retrospective cross-sectional study was conducted among children and adolescents with T1DM. Patients were followed up at the pediatric clinic at KAUH from January 2004 to December 2016. The study population comprised of 461 children and adolescents aged 1-18 years. The data were obtained by reviewing the medical records and laboratory findings from the hospital’s electronic system of all patients. Puberty was defined according to Tanner’s staging criteria, which defined puberty based on testes enlargement of >4 ml in volume in males and based on breast development in females. In the present study, the mean age of males and females was 13 and 11 years, respectively. Ethical approval for this study was obtained from the Research Ethics Committee of KAUH.
The data collected included initial disease presentation, hyperglycemia symptoms, DKA symptoms, associated autoimmune diseases, and chronic complications. Glycemic control was determined by measuring the HbA1c levels; with a target of ≤ 7.5%. The average HbA1c level over the last year was recorded. All the patients were allocated to 3 subgroups based on the glycemic control. The good glycemic control group had an HbA1c of <7.5%, the moderate glycemic control group had an HbA1c of 7.5- 9% and the poor glycemic control group had an HbA1c of >9% [14].
With regard to the laboratory findings and autoimmune comorbidities, serum levels of free thyroxine (fT4; Normal range, 12-22 pmol/L) and thyroid stimulating hormone (TSH; Normal range, 0.27-5 mIU/L) were measured. Thyroid antibody titers were also reviewed, as they were considered essential for the diagnosis of autoimmune thyroiditis. Moreover, high TSH levels with low fT4 levels were used to confirm hypothyroidism, whereas high TSH levels with normal fT4 levels were considered to reflect subclinical hypothyroidism. Celiac disease was diagnosed based on the presence of a high titer of IgA antitissue transglutaminase (≥ 20 IU/L) and was confirmed via Jejunal biopsy. However, a high antibody titer with a negative biopsy result was considered to indicate latent celiac disease. The presence of microalbuminuria was screened via spot urine samples and confirmed using 24 h urine samples. Microalbuminuria was defined as urinary albumin excretion of 20 200 μs/min (30-300 mg/day) or an albumin/creatinine ratio of 2.5-25 mg/mmol in boys and 3.5-25 mg/mmol in girls in the morning urine sample.
Retinopathy was identified by the presence of microaneurysm, exudates, microvascular abnormalities, hemorrhages, or macular edema. An experienced ophthalmologist carried out the assessment for evidence of cataract development, retinopathies, or refraction errors.
Dyslipidemia was diagnosed via abnormal lipid profile measurements based on the following criteria: low-density lipoprotein (LDL) >100 mg/dl, high-density lipoprotein (HDL) <35 mg/dL and/or triglycerides (TG) >150 mg/dL.
Vitamin D deficiency was detected by measuring the level of 25-hydroxyvitamin D (25(OH) D) in serum; a normal vitamin D level was defined as a 25(OH) D concentration of >30 ng/mL. If the serum 25(OH) D concentrations was between 20 and 30 ng/mL, the patient was labeled as vitamin D insufficient and when the concentration was <20 ng/mL, the patient was labeled as vitamin D deficient.
To assess for the presence of steatohepatitis, liver enzymes levels were measured, including aspartate aminotransferase (AST; normal value, 0-60 IU/L), alanine aminotransferase (ALT; normal value, 0-50 IU/L), and gamma-glutamyltransferase (GGT; normal value, 0-50 IU/L).
Statistical Analysis
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS) software version 16.0. Continuous variables, including age and mean HbA1c levels, are presented as a mean ± standard deviation, whereas categorical variables are presented as percentages. The analysis was performed by comparing the differences in HbA1c levels among pubertal & prepubertal age groups via independent-sample t-tests. Pearson correlation for continuous data was used to test the correlation between HbA1c levels with TG and LDL levels. Chi-square test was used to determine the relationship between vitamin D deficiency and gender. A p value of <0.05 was considered statistically significant for individual variables.
Results
A total of 461 children and adolescents with T1DM were enrolled, including 214 (46.4%) male patients and 247 (53.6%) female patients (mean age, 10.3 ± 4.7 years). A total of 146 (70.2%) male patients were at the prepubertal stage, whereas 62 (29.8%) male patients were at the pubertal stage. Moreover, a total of 121 (51.7%) female patients were at the prepubertal stage, whereas 113 (48.3%) female patients were at the pubertal stage.
The most common initial presentation of T1DM included hyperglycemic symptoms without DKA in 251 of 404 (62.1%) patients. Polyuria was the most common presenting symptom in 86.2% of cases. The other symptoms included polydipsia (79.4%), weight loss (42.2%), nocturia (11.1%), nocturnal enuresis (8%) and glycosuria (5%). With regard to DKA, a total of 153 (37.9%) diabetic children initially presented with DKA. Abdominal pain was the most common symptom (20.1%), followed by vomiting (18.6%). CNS changes, in the form of drowsiness and decreasing alertness were also observed in 6.5% patients. Kussmaul breathing, acetone breath, and ketonuria were observed in 3%, 2.3% and 1.8% of diabetic children, respectively.
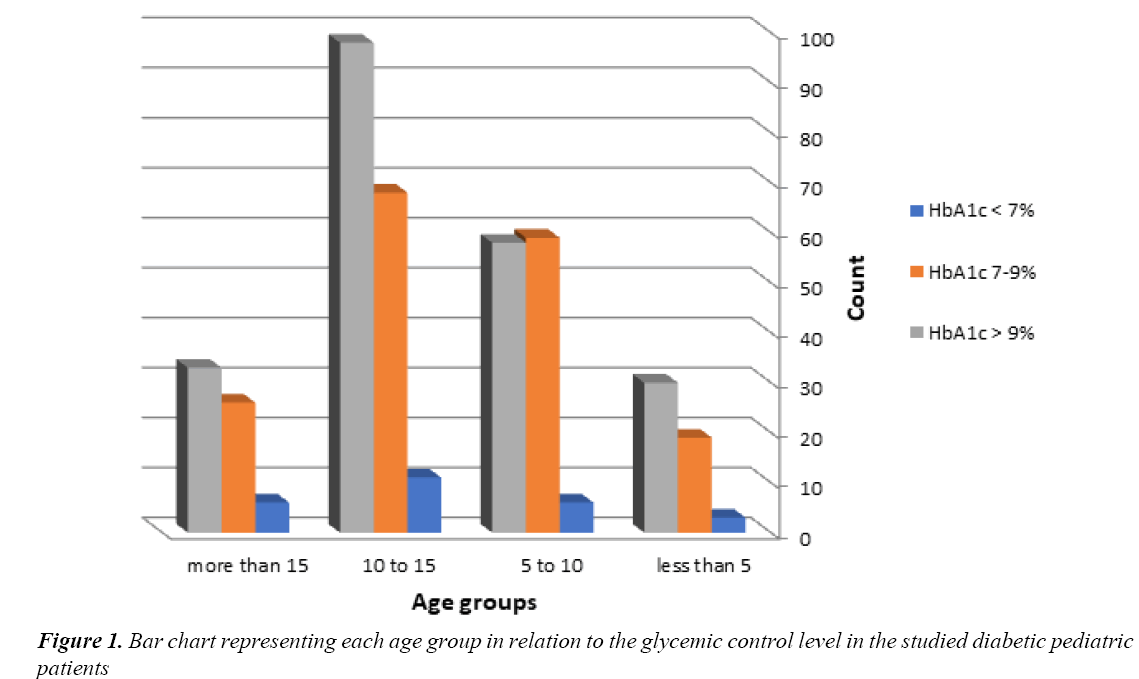
None of the cases presented with coma, seizures, or arrhythmia during the course of management. No reports of death due to diabetes were noted in this study. Regarding glycemic control, 123 (49.0%) had poor glycemic control, 113 (45.0%) had moderate glycemic control and 15 (6%) had good glycemic control in the prepubertal group. Moreover, 94 (57.0%) had poor glycemic control, 61 (37.0%) had moderate glycemic control and 10 (6.1%) had good glycemic control in the pubertal group (Figure 1 and Table 1).
| Variable | HbA1c<7% | HbA1c 7-9% | HbA1c>9% | p value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age | ||||
| <5 | (5.8) 3 | (36.5) 19 | (57.7) 30 | 0.601 |
| 5-10 | (4.9) 6 | (48) 59 | (47.2) 58 | |
| 10-15 | (6.2) 11 | (38.4) 86 | (55.4) 98 | |
| >15 | (9.2) 6 | 26 (40) | 33 (50.8) | |
| Gender | ||||
| Male | (8) 16 | (42) 84 | (50) 100 | 0.390 |
| Female | (5.1) 12 | (40.4) 95 | (54.5) 128 | |
Table 1: Demographic data of pediatric T1DM patients classified by glycemic control
The HbA1c level was 62.3% in the prepubertal group and 37.7% in the pubertal group. There was no significant relationship between glycemic control and gender, as 50% of male patients and 54.5% of female patients had poor metabolic control (p=0.390). Moreover, there was no significant relationship between HbA1c levels and age (p=0.840).
Vitamin D deficiency was observed in 208 (97.7%) diabetic patients and exhibited a significant relationship with gender (68.4% females and 51.9% males; p=0.001). In particular, 42.9% of children with established T1DM were vitamin D deficient, as compared to 57.1% of children with recent-onset diabetes. There was a strong relationship between poor glycemic control and vitamin D deficiency. In fact, 123 (58.9%) patients with poor metabolic control also had a low vitamin D level.
Most patients (83.4%) had normal TSH levels, whereas the others (16.6%) had high TSH levels. Moreover, approximately 89.5% of the studied population had normal fT4 levels, whereas the remaining (6.2%) had high fT4 levels. With regard to autoimmune thyroiditis, most cases (78.5%) had subclinical thyroiditis and 20% had clinical thyroiditis. The celiac antibody titer was positive in 8.2% of the studied patients, including 1.5% who were confirmed via biopsy and 6.7% who had latent celiac disease. The majority of cases (91.8%) showed normal biopsy findings.
Long-term Complications
Steatohepatitis was detected in 13.7% of male patients and 9% of female patients, as they had high levels of AST. Moreover, ALT levels were high in 5.4% male patients and 3.4% female patients, whereas GGT levels were high in 0.6% male patients and 2% female patients. Dyslipidemia was detected in 28 of 272 patients (10.3%) due to the high total cholesterol (TC) levels. Of these patients, 57.1% have reached puberty and 42.9% have not, including 18 female patients (12.6%) and 10 male patients (7.8%). Moreover, an increase in TG levels was detected in 8 of 28 patients (3%).
As for the ophthalmological complications, in the routine screening of 442 children, 25 (5.7%) were found to be affected; in fact, both male and female patients were found to be equally affected. Moreover, 12 (9.1%) patients who had reached puberty and 9 (3.4%) patients who had not yet reached puberty had eye complications. Refraction errors, retinopathy, glaucoma and cataract were detected in 20 (4.5%), 2 (0.5%) and 1 (0.2%) patients, respectively. Furthermore, 4 out of 28 (14.3%) affected children had good glycemic control, 9 out of 179 (5.1%) had moderate glycemic control and 13 out of 228 (5.7%) had poor glycemic control. Refraction errors were noted in only 1 child aged <5 years and in 3 children aged 5-10 years; ophthalmological complications were most commonly observed in children aged 10-15 years (n=14). Only 8 patients aged >15 years had ophthalmological complications.
Discussion
Approximately 65,000 children aged <15 years develop T1DM annually worldwide. Between 13% and 80% of these children present with DKA at the time of diagnosis. A study conducted between 2011 and 2013 reported that the highest frequencies for DKA at presentation of T1DM are noted in Saudi Arabia (44.9%), Taiwan (65%), Romania (67%) and the United Arab Emirates (80%), whereas the lowest such frequencies are noted in Hungary (23%), Finland (22%), Canada (18.6%) and Sweden (14%) [5]. Another study by Salman et al showed that DKA was the most common clinical presentation among children, and was observed in 67.3% of these patients [15]. However, in the present study, DKA was observed in only 37.9% of patients, although the DKA incidence did not significantly differ between Saudi and non-Saudi children (47.7% vs. 52.3%). The most common clinical presentations were polyuria followed by polydipsia. Thus, DKA was less common in the present study than in other local studies. This reduction in DKA incidence may be attributed to the high level of awareness among parents, the improved health services provided and early detection of the disease.
Caring for pediatric T1DM patients is a major challenge. Good glycemic control is essential for the prevention of long-term diabetes complications, such as retinopathy, nephropathy, and neuropathy. Moreover, good glycemic control decreases the frequency of complications and limits the progression of the current complications [16]. In the present study, we found that 6.4% of children had good glycemic control, 41.1% had average glycemic control and 52.4% had poor glycemic control. As the age of children increased, glycemic control became more challenging. In fact, glycemic control was found to be worse in adolescents than in younger children [17,18]. In the present study, the HbA1c level was higher in the prepubertal group. Similarly, a previous observational study in 2011, did not show a significant relationship between gender and glycemic control in children and adolescents with T1DM, which was confirmed in the present study. Cases of T1DM were more frequently associated with autoimmune diseases as compared to the general population, particularly with celiac disease and autoimmune thyroid disease. The latter is the most prevalent endocrine disease among diabetic patients [19]. A study was conducted on 17,749 children with T1DM in 118 diabetes centers in both Germany and Austria showed that 63% of patients had positive thyroid antibody test results [20]. In the present study, 326 had normal TSH levels and 65 had high TSH levels, whereas 348 had normal fT4 levels and 24 had high fT4 levels. Moreover, 51 exhibited sub-clinical disease and 13 exhibited clinical disease. There was no significant relationship between gender and TSH levels and most males and females had normal TSH levels.
Celiac disease is another autoimmune disease associated with T1DM. The prevalence of celiac disease in T1DM patients varies from 3% to 16% [21]. Another study conducted in 2001 showed that 11 of 158 patients with T1DM had celiac disease, as indicated via biopsy [22]. In the present study, 7 patients had celiac disease, 31 had latent celiac disease and 424 were normal. Gender was not a factor affecting the findings of celiac biopsy, and most males and females had normal biopsy findings.
Vitamin D plays a significant role in bone regulation and calcium metabolism. Vitamin D has recently been proven to be important in the pathogenesis of autoimmune diseases, such as T1DM. The compounds of vitamin D are known to inhibit T-cell activation by binding to the vitamin D receptor (VDR). Thus, VDR gene polymorphisms may play a role in T-cell-mediated autoimmune diseases [23]. In the Iranian population, VDR gene polymorphisms were found to be associated with T1DM [24,25]. Moreover, several studies indicated that T1DM is associated with vitamin D deficiency [26,27] consistent with our finding that vitamin D deficiency was associated with T1DM in 208 (97.7%) patients. Bin Abbas et al. [28] showed that the prevalence of vitamin D deficiency is 84% in T1DM children as compared to 59% in healthy children. In the present study, there was a significant relationship between gender and vitamin D levels (p=0.001). Most males and females had low vitamin D, although the proportion of females was larger.
In Saudi Arabia, vitamin D deficiency is highly predominant among T1DM children [29]. Based on the present study, children with recent onset diabetes had a higher incidence of vitamin D deficiency in comparison to children with established T1DM. Moreover, Borkar in 2010 [27], showed that 86% of patients with recent-onset diabetes were vitamin D deficient. Hence, the intake of vitamin D supplements in early childhood may protect against the development of T1DM [30]. In the present study, we found a significant relationship between poor glycemic control and vitamin D deficiency. Moreover, the HbA1c levels were inversely related to the vitamin D levels, thus indicating a possible connection between glycemic control and vitamin D metabolism.
Long-term uncontrolled glycemia is associated with risks of many life-threatening diseases and could have undesirable effects on various body organs. Hepatic involvement is common in diabetic patients and is an important cause of death in this population. Fatty liver is a well-known complication of diabetes, with a reported frequency of 40-70% [31]. In another study conducted in Egypt on 692 children, elevated ALT levels were found in 27 (3.9%), hepatomegaly on physical examination was noted in 13 (1.9%) and abnormal ultrasonographic findings were noted in 31 (4.5%) children [32]. Diabetic patients are at a higher risk of developing fatty liver than a normal person. In the present study, we found that 23 (13.7%) males had high AST levels and 18 (9%) females had high AST levels. Moreover, ALT levels were high in 9 (5.4%) males and 7 (3.4%) females. The level of the liver enzyme GGT was above normal in 1 (0.6%) male and 4 (2%) females.
Dyslipidemia was associated with poor glycemic control and was more common in children with diabetes [33]. A Korean study showed that 37.9% of 29 patients were classified as having dyslipidemia, including an increase in TC levels (27.6%) or increase in TG levels (14.3%). The authors concluded that 33% adolescents with T1DM had dyslipidemia. This finding may have been largely associated with high HbA1c levels [34]. In the present study, no significant associations were observed among HbA1c, LDL and TG levels. Dyslipidemia was detected in 28 patients (10.3%), due to high TC levels. Most of the patients were females who had reached puberty, and an increase in TG levels was noted in 8 of 28 patients (3%). Another study reported a high prevalence of dyslipidemia in young patients with T1D, particularly in pubertal females [35].
Diabetic nephropathy is a major late complication of T1DM. It is associated with significant morbidity and mortality. Microalbuminuria is considered to be an early sign of diabetic renal disease. In South America, 11.2% of the 205 patients admitted to the Pediatric Endocrinology Division were found to have microalbuminuria [36]. In Turkey, 155 children were shown to have a mean HbA1c of 8.4%, and 16.1% were found to have microalbuminuria [37]. In the present study, the frequency of microalbuminuria was 11%, including 57% at the pubertal stage (8.4% males and 13.5% females). The mean age of the cases of microalbuminuria was 12.75 ± 4.758 years. A significant association was observed between the occurrence of microalbuminuria and poor glycemic control.
Chronic ophthalmological complications as a result of diabetes occur in children with diabetes duration of at least 5 years. In 2015, the Children's Hospital of Pennsylvania conducted a study on the prevalence of ocular pathology in T1DM children. A total of 370 children were examined, and none of the children had diabetic retinopathy; however, 12 children had cataract and 41 children had high refractive errors [38]. In Tikur Anbesa Specialized Hospital in Ethiopia, the endocrine clinic examined diabetic children between 9 and 17 years of age. Of 86 children with a mean age of 13.7 years who were examined for retinopathy, only 4.7% had retinopathy (mean age, 14.25 ± 1.89 years) [39]. In Westmead Children’s Hospital in Australia, diabetic children aged 12-20 years were clinically examined for retinopathy; of the 944 patients, 9.0% had signs of retinopathy [40]. In Muhimbili National Hospital Clinic in Italy, 99 children aged 5-18 years were surveyed in for diabetic control, and 22.68% were found to have retinopathy [41]. In the present study, a total of 442 patients underwent an ophthalmological examination to determine the prevalence of ophthalmological complications. Such complications were noted in 25 patients (5.7%). No gender differences were observed for any disease types. However, there were significant differences in pubertal age and HbA1c levels among these patients. In particular, we found that children who reached pubertal age were more likely to have eye disease, as compared to children who had not yet reached pubertal age. Moreover, eye diseases were observed in children with high HbA1c levels.
Conclusion
The occurrence rate of DKA was lower than that reported in previous studies. In addition, unlike previous studies, DKA was not the most common clinical presentation. This difference may be related to the better awareness of patients and early diagnosis. Hence, regular screening for microalbuminuria is highly recommended for the early detection of diabetic nephropathy. Early detection of abnormal liver enzyme levels will also help prevent future complications. Moreover, early screening of vitamin D deficiency in children may protect against the development of T1DM. Hence, we recommend more educational sessions concerning diabetes care for both children and their families in order to achieve a tight glycemic control to further reduce the risk of complications.
References
- Vandewalle CL, Coeckelberghs MI, De Leeuw IH, et al. Epidemiology, clinical aspects and biology of IDDM patients under age 40 years: Comparison of data from Antwerp with complete ascertainment with data from Belgium with 40% ascertainment. The Belgian Diabetes Registry. Diabetes Care 1997; 20: 1556-1561.
- Al-Herbish AS, El-Mouzan MI, Al-Salloum AA, et al. Prevalence of type 1 diabetes mellitus in Saudi Arabian children and adolescents. Saudi Med J 2008; 29: 1285-1288.
- Cherian MP, Al-Kanani KA, Al Qahtani SS, et al. The rising incidence of type 1 diabetes mellitus and the role of environmental factors - Three decade experience in a primary care health center in Saudi Arabia. J Pediatr Endocrinol Metab 2010; 23: 685-696.
- Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137-149.
- Shaltout AA, Channanath AM, Thanaraj TA, et al. Ketoacidosis at first presentation of type 1 diabetes mellitus among children: A study from Kuwait. Sci Rep 2016; 6: 27519.
- Barker JM, Yu J, Yu L, et al. Autoantibody “sub specificity” in type 1 diabetes. Diabetes Care 2005; 28: 850-855.
- Hummel S, Hummel M, Banholzer J, et al. Development of autoimmunity to transglutaminase C in children of patients with type 1 diabetes: Relationship to islet autoantibodies and infant feeding. Diabetologia 2007; 50: 390-394.
- Al-Agha AE, Alafif M, Abd-Elhameed IA. Glycemic control, complications and associated autoimmune diseases in children and adolescents with type 1 diabetes in Jeddah, Saudi Arabia. Saudi Med J 2015; 36: 26.
- Al-Agha A, Ocheltree A, Hakeem A. Metabolic control in children and adolescents with insulin-dependent diabetes mellitus. J Clin Res Pediatr Endocrinol 2011; 3: 202.
- Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes control and complication trial. J Pediatr 1994; 125: 177-188.
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977-986.
- Nordwall M, Arnqvist HJ, Bojestig M, et al. Good glycemic control remains crucial in prevention of late diabetic complications – The Linköping Diabetes Complications Study. Pediatr Diabetes 2009; 10: 168-176.
- Diabetes Control and Complications Trial. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005; 353: 2643.
- Rewers M, Pihoker C, Donaghue K, et al. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes 2009; 10: 71-81.
- Salman H, Abanamy A, Ghassan B, et al. Insulin-dependent diabetes mellitus in children: Familial and clinical patterns in Riyadh. Ann Saudi Med 1991; 11: 302-306.
- Donaghue KC, Chiarelli F, Trotta D, et al. Microvascular and macrovascular complications associated with diabetes in children and adolescents. Pediatr Diabetes 2009; 10: 195-203.
- Flück CE, Kuhlmann BV, Mullis PE. Metabolic control in children and adolescents with diabetes mellitus type I in Berne: A cross-sectional study. Schweizerische Medizinische Wochenschrift 1999; 129: 1650-1655.
- Tonella P, Fluck CE, Mullis PE. Metabolic control of type 1 diabetic patients followed at the University Children’s Hospital in Berne: Have we reached the goal. Swiss Med Wkly 2010; 140: 44.
- Van den Driessche A, Eenkhoorn V, Van Gaal L, et al. Type 1 diabetes and autoimmune polyglandular syndrome: A clinical review. Neth J Med 2009; 67: 376-387.
- Kordonouri O, Klinghammer A, Lang EB, et al. Thyroid autoimmunity in children and adolescents with type 1 diabetes. Diabetes Care 2002; 25: 1346-1350.
- Volta U, Tovoli F, Caio G. Clinical and immunological features of celiac disease in patients with type 1 diabetes mellitus. Expert Rev Gastroenterol Hepatol 2011; 5: 479-487.
- Mahmud FH, Murray JA, Kudva YC, et al. Celiac disease in type 1 diabetes mellitus in a North American community: Prevalence, serologic screening and clinical features. Mayo Clin Proc 2005; 80: 1429-1434.
- Motohashi Y, Yamada S, Yanagawa T, et al. Vitamin D receptor gene polymorphism affects onset pattern of type 1 diabetes. J Clin Endocrinol Metab 2003; 88: 3137-3140.
- Mohammadnejad Z, Ghanbari M, Ganjali R, et al. Association between vitamin D receptor gene polymorphisms and type 1 diabetes mellitus in Iranian population. Mol Biol Rep 2012; 39: 831-837.
- Bonakdaran S, Abbaszadegan MR, Dadkhah E, et al. Vitamin D receptor gene polymorphisms in type 1 diabetes mellitus: A new pattern from Khorasan province, Islamic Republic of Iran. East Mediterr Health J 2012; 18: 614.
- Pozzilli P, Manfrini S, Crino A, et al. Low levels of 25-hydroxyvitamin D3 and 1, 25-dihydroxyvitamin D3 in patients with newly diagnosed type 1 diabetes. Hormone Metab Res 2005; 37: 680-683.
- Borkar VV, Verma S, Bhalla AK. Low levels of vitamin D in North Indian children with newly diagnosed type 1 diabetes. Pediatr Diabetes 2010; 11: 345-350.
- Bin-Abbas BS, Jabari MA, Issa SD, et al. Vitamin D levels in Saudi children with type 1 diabetes. Saudi Med J 2011; 32: 589-592.
- Al-Daghri NM, Al-Attas OS, Alokail MS, et al. Lower vitamin D status is more common among Saudi adults with diabetes mellitus type 1 than in non-diabetics. BMC Public Health 2014; 14: 153.
- Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: A systematic review and meta-analysis. Arch Dis Childhood 2008; 93: 512-517.
- Levinthal GN, Tavill AS. Liver disease and diabetes mellitus. Clin Diabetes 1999; 17: 73.
- El-Karaksy HM, Anwar G, Esmat G, et al. Prevalence of hepatic abnormalities in a cohort of Egyptian children with type 1 diabetes mellitus. Pediatric Diabetes 2010; 11: 462-470.
- Maahs DM, Dabelea D, D'agostino RB, et al. Glucose control predicts 2 year change in lipid profile in youth with type 1 diabetes. J Pediatr 2013; 162: 101-107.
- Kim SH, Jung IA, Jeon YJ, et al. Serum lipid profiles and glycemic control in adolescents and young adults with type 1 diabetes mellitus. Ann Pediatr Endocrinol Metab 2014; 19: 191-196.
- Homma TK, Endo CM, Saruhashi T, et al. Dyslipidemia in young patients with type 1 diabetes mellitus. Arch Endocrinol Metab 2015; 59: 215-219.
- de Almeida Salgado PP, Silva IN, Vieira ÉC, et al. Risk factors for early onset of diabetic nephropathy in pediatric type 1 diabetes. J Pediatr Endocrinol Metab 2010; 23: 1311-1320.
- Demirel F, Tepe D, Kara Ö, et al. Microvascular complications in adolescents with type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol 2013; 5: 145.
- Geloneck MM, Forbes BJ, Shaffer J, et al. Ocular complications in children with diabetes mellitus. Ophthalmology 2015; 122: 2457-2464.
- Shibeshi MS, Fantahun B, Kebede T, et al. Pediatric diabetic retinopathy: Experience of a tertiary hospital in Ethiopia. BMC Res Notes 2016; 9: 116.
- Sasongko MB, Wong TY, Donaghue KC, et al. Retinal arteriolar tortuosity is associated with retinopathy and early kidney dysfunction in type 1 diabetes. Am J Ophthalmol 2012; 153: 176-183.
- Majaliwa ES, Munubhi E, Ramaiya K, et al. Survey on acute and chronic complications in children and adolescents with type 1 diabetes at Muhimbili National Hospital in Dar es Salaam, Tanzania. Diabetes Care 2007; 30: 2187-2192.