Research Article - Journal of Public Health and Nutrition (2022) Volume 5, Issue 6
Clinical characteristics of people living with HIV/AIDS on ART in 2014 at tertiary health institutions in Enugu, Nigeria
Matthew Chibunna Igwe1, Emmanuel Ifeanyi Obeagu2*, Alphonsus Ogbonna Ogbuabor1
1Department of Medical Laboratory Science, Enugu State University of Science and Technology, Enugu State, Nigeria
2Department of Medical Laboratory Science, Kampala International University, Western Campus, Ishaka, Uganda
- Corresponding Author:
- Emmanuel Ifeanyi Obeagu
Department of Medical Laboratory Science
Kampala International University
Western Campus, Uganda.
Email: emmanuelobeagu@yahoo.com
Received: 14-Sep-2022, Manuscript No. AAJPHN-22-74694; Editor assigned: 16-Sep-2022, PreQC No. AAJPHN-22-74694(PQ); Reviewed: 30-Sep-2022, QC No AAJPHN-22-74694; Revised: 31-Oct-2022, Manuscript No. AAJPHN-22-74694(R); Published: 07-Nov-2022, DOI:10.35841/aajphn-5.6.130
Citation: Igwe CM, Obeagu IE, Ogbuabor OA. Clinical characteristics of people living with HIV/AIDS on ART in 2014 at tertiary health institutions in Enugu, Nigeria. J Pub Health Nutri. 2022;5(6):130
Abstract
Background information: Survival of people living with HIV/AIDS (PLWHA) has increased since the emergency of High Active Antiretroviral Therapy (HAART) in 1996. HIV cascades have been constructed so that the final outcome is one that will have a positive effect on reducing HIV incidence, morbidity and mortality by suppressing the viral load and thereby increased the CD4 cell counts. The study was aimed to determine the Longitudinal Cascade and Survival analysis of people living with HIV/AIDS in tertiary health institutions in Enugu state. Methodology: This was a descriptive cross-sectional study design. The study population consisted of those diagnosed for HIV/AIDS at tertiary health institutions in Enugu State. The total numbers of clients enrolled were 793 and 249 clients were loss to follow up, majority was males. Those initiated on ART were 544. Clients of age <15 years were excluded and they were 31 clients. Finally, 500 clients were selected, males were 138 and female were 362 by simple random sampling techniques. Data was collected from HIV / AIDS patients ART record cards, registers and institutions data units for those initiated on ART in 2014 using a designed proforma. Those clients aged 15 years and above were retrospectively studied between 2014 and 2018 and some of them that survived after five years (60 months) on ART were interviewed by applying simple random sampling technique. Cohort inclusion begins at initiation on ART with follow-up clinical information collected year by year for five years. IBM SPSS statistics version 24.0 was used. Chi square test was used to assess association between categorical variables and the level of statistical significance of the proportions was determined by a P-value less than 0.05. Manual content analysis was used for the interview and probability of dying and surviving analysis. Results: The majority of the baseline CD4 cell count results presented by clients before initiated on ART were within 100-199 cell/mm3 106 (23.1%). This was followed by those within 200-299 cell/mm3 105 (22.9%). The least baseline results were those within the group ≤ 50 cell/mm3, 33 (7.17%). In all, 460 people presented their CD4 cell count baseline results before placed on ART. CD4 cell count results at 60 month indicate that those clients of CD4 cell count results group ≥ 500, 160 (51.1%) were highest, followed by group within 400- 499, 300-399 and 200-299 which while 92 (29.4%), 45 (14.4%) and 16 (5.1%) respectively. Conclusion: Based on the study, HIV prevalence in Nigeria now appears to have assumed a downward trend following the availability of ART and a relative stability from 2012 to 2018, yet a sustained and more effective intervention is still needed to avert increase incidence by mostat– risk subpopulations in the Enugu State.
Keywords
PLWHA, Adherence, ART, CD4 count, Clinical history, HIV, AIDS.
Introduction
The HIV epidemic continues to be a major global public health issue until is totally eradicated. In 2018, there were 37.9 million men, women, and children living with HIV/AIDS globally, while those newly infected with HIV in 2018 were 1.7 million men, women and children and there were 770,000 AIDS-related deaths in 2018 [1]. Cameroon, Cote d’Ivoire and Nigeria account for close to 60% of new HIV infections and 54% of AIDS-related deaths each year. Decisive improvements in their national HIV programmes would have a major impact on the region’s overall HIV response. The recent Nigeria AIDS Indicator and Impact Survey (NAIIS) found lower HIV prevalence than earlier surveys, which led to a revision of the country’s HIV estimate. The latest regional estimates reflect this additional information, with lower estimates of people living with HIV, AIDS-related deaths and HIV infections than previous estimates [1].
Nigeria is populous country, and so it has a very high number of people living with HIV/AIDS despite a relatively low HIV prevalence. Introducing Antiretroviral Treatment (ART) for all people living with HIV not only benefits those already living with HIV, but also drastically reduces the chance of onwards HIV transmission to others, by reducing the viral load and increasing the CD4 cell counts. In a country such as Nigeria, where so many people are not on treatment, it is hard to tackle the HIV epidemic [2].
Life expectancy of people living with HIV/AIDS (PLWHA) has increased considerably since the introduction of the highly active antiretroviral therapy (HAART) in the mid-1990s due to the reconstitution of immune response [3-7]. HIV/AIDS has gradually been considered as a chronic disease with life expectancy almost comparable to non-HIV chronic illnesses [8].
Survival of people living with HIV/AIDS (PLWHA) has increased since the emergency of High active antiretroviral therapy (HAART) in 1996. Fewer HIV/AIDS-related deaths and cohort have resulted in an increase in the proportion of HIV/AIDS patients dying from non-HIV/AIDS-related disorders. Low level of access to antiretroviral treatment, inadequate laboratory facilities (for monitoring their viral load, CD4 cell counts etc), knowledge and attitude of some patients, cultural believe, punitive laws against homosexual, and increase in HIV and TB co-infection remain an issue for PLWHA, meaning that there are still many HIV / AIDS related deaths in Nigeria [9].
Materials and Methods
Study area
The study was conducted in Enugu state, Nigeria.
Study design
A descriptive cross-sectional study design was adopted.
Study population and health facilities
The study population consisted of those diagnosed for HIV / AIDS at two tertiary health institutions in Enugu State; Enugu State University of Science and Technology Teaching Hospital, Parklane (ESUTHP) and University of Nigeria Teaching Hospital (UNTH). These tertiary health facilities are where most persons diagnosed with HIV/AIDS are referred to. This is because they are very equipped with all the necessary services. And they are located in both urban (ESUTHP) and rural area (UNTH) of the State. Baselines for clinical and laboratory investigations such as; viral load, CD4 cell counts, haematological and biochemical parameters and general management are carried out there. Those clients aged 15 years and above were followed-up between 2014 and 2018 and some of those survived after five years (60 months) on ART were interviewed by applying simple random sampling selection.
Inclusion criteria: all PLWHA aged 15 years and above that were initiated on ART in the year 2014 at both health institutions. Exclusion criteria: all PLWHA less than 15 years of age that were initiated on ART in the year 2014 at both health institutions.
Sample size determination
The minimum sample size was determined by using a Fisher’s formula.
N = Z 2 pq / d 2
Where:
n=Desired sample size
Z=The standard normal deviate set at 1.96 which correspond to 95% confidence level.
P=Estimated proportion of the attribute present in the population. And q=1- P
d = degree of precision desired set at 0.05 (error margin of 5%)
Therefore
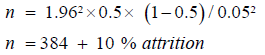
Therefore, a minimum sample (n)=384+38=422.
A total of 500 PLWHA aged 15 years and above were studied.
Sampling technique
A multistage sampling technique was adopted.
Selection of participants
A simple random sampling technique was used to select PLWHA that were 15 years of age and above from clinic records, registers and data units.
Data collection tools
Data was collected from HIV/AIDS patients ART record cards, registers and institutions data units at UNTH and ESUTH for those initiated on ART in 2014 using a designed proforma and one-on-one structured interview of those survived after five years on ART. Data collected include; socio-demographic variables, clinical and immunological characteristics (CD4 cell counts, Viral Load). Microsoft Excel, 2013 was used to clean those collected data to ensure missing variables will be re-collected and confirmed using paper-based patient ART records and registers. Socio-demographic and clinical characteristics were considered as the independent variables, and three trained graduates research assistants were involved.
Statistical analysis
Cohort inclusion begins at initiation on ART with follow-up clinical information collected year by year for five years. The Excel dataset was imported into IBM SPSS statistics version 24.0 (IBM Corp; Amonk, NY, USA). Socio-demographic and clinical characteristics were described using the frequency and proportion for categorical variables. Chi square test was used to assess association between categorical variables and statistical significance of the proportions was set at P-value less than 0.05. Manual content analysis was used based on the topic guide of the interview. Probability of dying and surviving was done using Manual content analysis also.
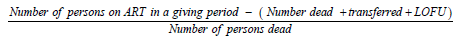
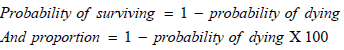
Manual content analysis was used for both interview and probability of dying.
Formular for probability of dying
Ethical considerations
Ethical clearances were obtained from Enugu State University of science and technology teaching hospital, Parklane (ESUTHP) with reference number: ESUTHP/C-MAC/ RA/034/100 and University of Nigeria teaching hospital (UNTH) with reference number: UNTH/CSA/329/VOL.5 through their Ethics and Research committees. Confidentiality was maintained at all stages of the data collections.
In Tables 1A and Tables 1B, majority of the baseline CD4 cell count results presented by clients before initiated on ART were within 100-199 cell/mm3 106 (23.1%). This was followed by those within 200-299 cell/mm3 105 (22.9%). The least baseline results were those within the group ≤ 50 cell/ mm3, 33 (7.17%). In all, 460 people presented their CD4 cell count baseline results before placed on ART.
| Variable | Frequency n=500 |
Gender | |
|---|---|---|---|
| MALE | FEMALE | ||
| Infections Herpes zoster |
38 | 12 (31.6%) | 26 (68.4%) |
| Tb | 8 | 3 (37.5%) | 5 (62.5%) |
| Oral/virginal thrush | 6 | 0.0 (0.0%) | 6 (100.0%) |
| Sti | 9 | 2 (22.2%) | 7 (77.8%) |
| Others | 29 | 10 (34.5%) | 19 (65.5%) |
| Total | 90 | 27 (30.0%) | 63 (70.0%) |
| Cd4 cell count baseline (cells/mm3) | |||
| ≤ 50 | 76 | 22 (28.9%) | 54 (71.1%) |
| 50-99 | 56 | 11 (19.6%) | 45 (80.4%) |
| 100-199 | 106 | 33 (31.1%) | 73 (68.9%) |
| 200-299 | 105 | 27 (25.7%) | 78 (74.3%) |
| 300-399 | 49 | 14 (28.6%) | 35 (71.4%) |
| 400-499 | 35 | 11 (31.4%) | 24 (68.6%) |
| ≥ 500 | 33 | 11 (33.3%) | 22 (66.7%) |
| Total | 460 | 129 (28.0%) | 331 (72.0%) |
| Out come of art | |||
| Under care | 374 | 90 (24.1%) | 284 (75.9%) |
| Death | 29 | 11 (37.9%) | 18 (62.1%) |
| Loss of follow up | 66 | 26 (39.4%) | 40 (60.6%) |
| Transferred | 31 | 11 (35.5%) | 20 (64.5%) |
| Total | 500 | 138 (27.6%) | 362 (72.4%) |
| Who clinical stage baseline | |||
| Stage 1 | 393 | 110 (28.0%) | 283 (72.0%) |
| Stage 2 | 66 | 15 (22.7%) | 51 (77.3%) |
| Stage 3 | 38 | 12 (31.6%) | 26 (68.4%) |
| Stage 4 | 3 | 1 (33.3%) | 2 (66.7%) |
| Total | 500 | 138 (27.6%) | 362 (72.4%) |
| ART REGIMEN | |||
| Azt-3tc-efv | 17 | 4 (23.5%) | 13 (76.5%) |
| Azt-3tc-nvc | 26 | 10 (38.5%) | 16 (61.5%) |
| Tdf-3tc-efv | 352 | 97 (27.6%) | 255 (572.4%) |
| Tdf-3tc-nvp | 93 | 25 (26.9%) | 68 (73.1%) |
| Second line art | 6 | 1 (16.7%) | 6 (83.3%) |
| Others | 5 | 1 (20.0%) | 4 (80.0%) |
| Total | 500 | 138 (27.6%) | 362 (72.4%) |
Table 1A: Clinical characteristics of PLWHA initiated on ART in 2014 at tertiary health institutions in Enugu.
| Variable | Frequency N=500 |
Gender | |
|---|---|---|---|
| MALE | FEMALE | ||
| Infections Cd4 cell count at 60 Month (cells/mm3) | |||
| 300-499 | 36 | 15 (41.7%) | 21(58.3%) |
| 500-699 | 65 | 22 (33.8%) | 43(66.2%) |
| 700-899 | 82 | 25 (30.5%) | 57 (69.5%) |
| ≥ 900 | 130 | 37 (28.5%) | 93 (71.5%) |
| Total | 313 | 99 (31.6%) | 214(68.4%) |
Table 1b: Clinical characteristics of PLWHA initiated on ART in 2014 at tertiary health institutions in Enugu.
On outcome of ART, 374 (74.8%) were under care. Those loss to follow up were 66 (13.2 %), 29 (5.8%) died within the period of study and 31 (6.2%) were transferred out.
Stage 1 of baseline WHO clinical stage was the highest, 393, while males and females were 110 (28.0%) and 283 (72.0%) respectively. It was followed by stage 2 and down the line.
The most common co-morbidities of the clients was Herpes zoster, 38 (42.2%), STI, 9 (10.0%) and TB, 8 (8.9%), and others was 29 (32.2%).
TDF-3TC-EFV, 362 (70.4%) is the most ART used during the period of the study, followed by TDF-3TC-NVP, 94 (18.8%), they were only 6 (1.2%) that used the second line ART.
CD4 cell count results at 60 month indicate that those clients of CD4 cell count results group ≥ 500, 160 (51.1%) were highest, followed by group within 400-499, 300-399 and 200-299 which while 92 (29.4%), 45 (14.4%) and 16 (5.1%) respectively.
Discussion
More than half of the clients had a low CD4 cell counts (≤199.0 cells/ml) at the baseline assessment. Delayed access to HIV services for patients with low CD4 counts led to a higher death rate. Even though those on the second-line ART regimen of this study were low, 7 (1.4%) when compared with others, 493 (98.6 %), it was still a strong predictor of mortality among the clients. Some clients still die despite the fact that they on ART regimen, a possible reason might be the low CD4 counts at the baseline assessment. This is in line with those of multi-cohort studies in the Asian and African regions [10]. Predictors of death include being illiterate, bedridden, with a low baseline CD4 cell counts, and on the second-line ART regimen [11]. CD4 cell counts at first presentation in our clients steadily increased with time, consistent with the findings of other studies in South Africa [12].
As in table above, there are significant increases in CD4 cell count at 5th year (60 month) when compared with those of baseline. Increase in CD4 cell count up to ≥ 900 cell/ml is an indicator that there is suppressor in viral load. Improvements in survival during the second, third and other years of ART are probably caused by increased viral suppression, declining rates of viral failure, and increasing treatment options [13]. Simpler regimens might have contributed to improvements in both might encourage patients to engage in risk reduction programmes, to cease smoking, and to increase adherence to ART [14].
Conclusion
Based on the study, HIV prevalence in Nigeria now appears to have assumed a downward trend following the availability of ART and a relative stability from 2012 to 2018, yet a sustained and more effective intervention is still needed to avert increase incidence by most-at–risk subpopulations in the Enugu State.
References
- UNAIDS Data. 2019.
- Awoyemi AA, Olusegun EO. HIV epidemiology in Nigeria. Saudi J Biol Sci. 2018;25(4):697-703.
- Odo M, Ochei K.C, Obeagu EI, et al. TB Infection Control in TB/HIV Settings in Cross River State, Nigeria: Policy Vs Practice.J Pharm Res Int. 2020;32(22):101-9.
- Offie DC, Obeagu EI, Akueshi C, et al. Facilitators and Barriers to Retention in HIV Care among HIV Infected MSM Attending Community Health Center Yaba, Lagos Nigeria.J Pharm Res Int. 2021;33(52B):10-9.
- Ezeoru VC, Enweani IB, Ochiabuto O, et al. Prevalence of Malaria with Anaemia and HIV Status in Women of Reproductive Age in Onitsha. J Pharm Res Int. 2021;33(4):10-19.
- Ifeanyi OE, Uzoma, OG, Ejike FC, et al. Evaluation of Some Cytokines, CD4, Hepcidin, Iron Profile and Some Haematological Parameters of Pulmonary Tuberculosis Patients Coinfected with HIV in Southeast of Nigeria.J Pharm Res Int. 2020;32(13):118-30.
- Obeagu EI. Comparative Analysis of Interferon-Gamma, IL-6, IL-10, CD4, Hepcidin, Iron Status and Some Haematological Parameters of Control and Non ART HIV Positive Subjects. Sch J App Med Sci. 2019;7(7):2383-91.
- Etard JF, Ndiaye I, Thierry-Mieg M, et al. Mortality and causes of death in adults receiving highly active antiretroviral therapy in Senegal: a 7- year cohort study. AIDS Lond Engl. 2006;20(8):1181-9.
- Avert. HIV AND AIDS in Nigeria. 2018.
- PujadesRodringuez M, Balkan S, Arnould L, et al. Treatment failurelity factors in patients receiving second-line HIV therapy in resource-limited Countries. JAMA. 2010;304:303-12.
- Zaw Zaw Aung, Yu Mon Saw, Thu Nandar Saw, et al. Survival rate and mortality risk factors among TB-HIV co-infected patients at an HIV specialist hospital in Myanmar: A 12-years retrospective follow-up study. Int J Infect Dis. 2019;80:10-15.
- Peltzer K, Friend-du Preez N, Ramlagan S, et al. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, SouthAfrica. BMC Public Health. 2010;10:111.
- Gill VS, Lima VD, Zhang W. Improved virological outcomes in British Columbia concomitant with decreasing incidence of HIV type 1 drug resistance detection. Clin Infect Dis. 2010;50(1):98-105.
- Rockstroh JK, Gatell J, Landman R, et al. Management of late-presenting patients with HIV infection. Antivir Ther. 2010;15(1):25-30.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref