Research Article - Biomedical Research (2017) Volume 28, Issue 17
Changes of immune function and its correlation with biliary tract infection before and after biliary stent in malignant obstructive jaundice
Chengli Liu1*, Cheng Wang1, Hui Zhang1, Xiaoxia Zang2, Gang Zhao1, Yalin Kong1, Yingjie Wang3 and Hongqi Li3
1Department of Hepatobiliary Surgery, Air Force General Hospital of Chinese People’s Liberation Army, Haidian, Beijing, PR China
2Department of Stomatology, Air Force General Hospital of Chinese People’s Liberation Army, Haidian, Beijing, PR China
3Department of Oncological Radiotherapy, Air Force General Hospital of Chinese People’s Liberation Army, Haidian, Beijing, PR China
- *Corresponding Author:
- Chengli Liu
Department of Hepatobiliary Surgery
Air Force General Hospital of Chinese People’s Liberation Army
Haidian, Beijing, PR China
Accepted date: August 03, 2017
Abstract
Objective: To investigate the changes of immune function and its correlation with biliary tract infection before and after biliary stent in malignant obstructive jaundice.
Methods: A total of 148 patients from September 2014 to 2016 were collected in our hospital, the level of glycosylated haemoglobin, white blood cells, CD4+ T cell count, CD8+ T cell count and CD4+/CD8+ ratio, neutrophil count and percentage of neutrophil etc., total bilirubin, alanine aminotransferase, plasma hs-CRP, TNF-α, IL-1β, IL-6, IL-8 were recorded and compared before and after surgery.
Results: After a follow-up of 6 weeks, the CD4+ T lymphocytes count was significantly increased than that of before surgery (F=10.23, P=0.02). After follow-up of 6 weeks, the proportion of CD4+/CD8+ increased to 2.37 ± 1.09%, compared with that of before biliary stent implantation 0.71 ± 0.21%, the difference was statistically significant (F=21.74, P=0.02). 3 weeks after operation, hs-CRP, TNF-α, IL-1β, IL-6, IL-8, the levels of total bilirubin, alanine aminotransferase were significantly lower than that before operation (F=12.83, 18.45, 29.4, 12.8, 10.6, 9.29, 10.08; P=0.03, 0.01, 0.01, 0.02, 0.02, 0.00, 0.01, respectively). High risk factors for increasing CD4+/CD8+ ratio were investigated with patients of malignant obstructive jaundice, which includes blood glucose, glycosylated hemoglobin, ALT, AST, LDL-C, HDL-C and triglycerides, hs-CRP, neutrophil count, neutrophil percentage, T lymphocyte count, ratio of CD4+/CD8+ and biliary tumor size.
Conclusion: For patients with malignant obstructive jaundice, biliary stent could improve cholestasis by increasing the proportion of CD4+/CD8+ T lymphocytes, which can improve immune system, function for patients with malignant obstructive jaundice.
Keywords
Malignant obstructive jaundice (MOJ), Biliary tract infection, Immune function, Biliary stent
Introduction
Malignant Obstructive Jaundice (MOJ), is a series of clinical signs caused by bile duct obstruction due to hepatic and external bile duct obstruction, which will result in growth, invasion, or metastasis of tumors [1,2]. At present, percutaneous biliary stent implantation is a mainly surgery characterized by minimally invasion, higher efficiency and success rate of reducing jaundice [3]. However, postoperative complications such as infection, bleeding, bile leakage, pancreatitis and so on are more common, especially the postoperative infection [4,5]. According to statistics, the incidence of complications can be as high as 30-50%, while the endotoxin was as high as 50-80% [6]. After injury of the intestinal mucosal barrier, jaundice will probably cause the imbalance of intestinal flora. If infection occurs at the same time, it can easily cause liver failure and multiple organ dysfunction syndrome [7,8]. In this condition, the efficiency of anti-infection treatment is very low. If the MOJ induced enterogenous endotoxin and got into the circulation, it will further cause sepsis, MODS and even death during the perioperative period [9,10].
In this study, 148 patients with malignant obstructive jaundice were enrolled. Logistic regression analysis was performed on the patients with CD4+/CD8+ ratio and biliary tract infection, and the related factors were also investigated. In addition, we performed the biliary stent procedures for the enrolled patients and observed its effect on immune function changes after surgery. Finally, we evaluated the clinical efficacy of biliary stent implantation in the treatment of jaundice.
Materials and Methods
Clinical data
148 cases of patients with malignant obstructive jaundice were collected from September 2014 to 2016, including 78 males and 70 females with an average age of 61.8 ± 4.6 y old. The course of the disease varied from 3 months to 5 y, and the average course was 2.7 ± 1.3 y. Average operation time was 65.2 ± 12.6 min. Average blood loss was 56.4 ± 4.7 ml. Average hospital stay was 6.8 ± 1.3 d. All the patients in this research group were informed and signed the informed consent. This study has been approved by the Ethics Committee of our hospital.
Inclusion and exclusion criteria
Diagnostic criteria: Biochemical indicators: total bilirubin exceeds the upper limit of the normal value; direct bilirubin/ total bilirubin>50%; Radiographic parameters: Intrahepatic tumor, with or without extra hepatic bile duct dilatation, clinical manifestation of invasion or compression in extra hepatic bile duct caused by malignant tumor. Other indicators: Positive urine bilirubin and clay colored stools.
Inclusion criteria: (A) The clinical or pathological examination identified as malignant obstructive jaundice; (B) No surgical indications; (C) Patients agreed to perform percutaneous biliary stent implantation and had signed informed consent prior to surgery.
Exclusion criteria: (A) Accompanied with duodenal obstruction, patients are unable to take food orally preoperatively; (B) Unsuccessful biliary stent implantation; (C) Hemorrhage and other non-infectious causes leads to exacerbations; (D) Before biliary obstruction, liver dysfunction caused by primary liver diseases such as viral hepatitis; (E) Comorbidities such as serious diseases of heart, lung and kidney; (F) After surgery, patients are unwilling to cooperate to continue the examination and treatment.
Methods
Observational parameters
Venous sterile whole blood 4-6 ml was extracted, peripheral blood leukocyte and neutrophil were detected. Quantification of T lymphocyte subsets by monoclonal antibody assay. Detection method: HbA1c detection, with fasting, peripheral blood 4-6 ml of patients was detected by Variant II hemoglobin detector (Bio-Rad Company, United States). Fasting Blood Glucose (FBG): Medtronic (Medtronic, USA) portable blood glucose meter was applied to detect FBG. Other biochemical indicators: Blood lipid, aminotransferase and other biochemical indicators were detected by Roche Modular automatic biochemical analyzer. CRP was determined to use the immune assay (Zhongshan golden bridge, China). The determination of TNF-α, IL-1 beta, IL-6, IL-8, etc., were detected by enzyme-linked immunosorbent assay (Cenzyme Kit).
Biliary stent implantation
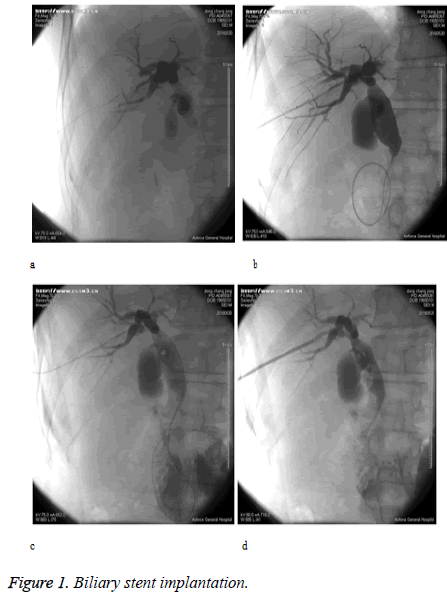
(1) Take the eighth intercostal space of right midaxillary line as puncture point, inject the 37% iopromide injection to reveal intrahepatic bile duct dilatation through percutaneous transhepatic. (2) Exit the stylet then intubate the guide wire, adjust the guide wire to get it through the stricture bile duct. (3) Implant the puncture trocar through the fine guide wire. (4) Implant the stiff type guide wire to get it through the stricture bile duct then into the duodenum. (5) Use the stiff type guide wire to reach biliary stenting, and then reveal that the contrast agent passed successfully and got into the duodenum. (6) Indwell the external drainage catheter through the guide wire, implant the end of the guide wire in common bile duct, exit the guide wire, then fix the external drainage catheter to skin (Figures 1a-d).
Statistics
SPSS19.0 software was used for statistical analysis in this study, quantitative data were compared by analysis of variance (ANOVA), fisher exact method. Correlation between postoperative lymphocyte changes and biliary tract infection were evaluated by Pearson's correlation, , the difference was statistically significant when P<0.05.
Results
Comparison of results of T cell subsets
After operation, the total number of leukocytes, neutrophils and lymphocytes, CD4+ T cell count, percentage of CD4+ T cells, CD8+ T cell counts, the percentage of CD8+ T cells were all recorded and statistically analyzed. 6 weeks after operation, the CD4+ T cell count and percentage, ratio of CD4+/CD8+ showed significantly difference (P<0.05) compared with the preoperative records (Table 1).
| Items | Cases (n) | Before treatment | 3 weeks after operation | 6 weeks after operation | F value | P value |
|---|---|---|---|---|---|---|
| CD4+ T cell count (cells/μL) | 148 | 421.7 ± 102.5 | 512.6 ± 79.3* | 669.4 ± 102.4*# | 10.23 | 0.02 |
| Percentage of CD4+ T cells (%) | 148 | 37.4 ± 14.3 | 55.6 ± 14.7* | 58.9 ± 12.6*# | 2.24 | 0.02 |
| CD8+ T cell count (cells /μL) | 148 | 337.3 ± 64.5 | 435.7 ± 35.8* | 473.2 ± 56.4*# | 0.87 | 0.39 |
| Percentage of CD8+ T cells (%) | 148 | 430.4 ± 102.4 | 521.7 ± 111.2* | 1489.4 ± 148.4*# | 0.97 | 0.33 |
| CD4+/CD8+ (%) | 148 | 0.71 ± 0.21 | 0.89 ± 0.24* | 2.37 ± 1 .09*# | 21.74 | 0.02 |
Table 1. Comparison of results of T cell subsets (͞x ± s).
Comparison of percentage of white blood cell count, neutrophil count and percentage of neutrophil
White blood cell count, neutrophil count and percentage of neutrophil after biliary stent implantation were analyzed statistically, and there was no significant difference (P>0.05) (Table 2).
| Items | Cases (n) | Before treatment | 3 weeks after operation | 6 weeks after operation | F value | P value |
|---|---|---|---|---|---|---|
| White blood cell count (× 109/L) | 148 | 17.65 ± 11.16 | 8.87 ± 2.32* | 7.85 ± 1.13* | 28.23 | 0 |
| Neutrophil count (× 109/L) | 148 | 12.23 ± 1.39 | 7.12 ± 1.21* | 6.87 ± 0.86* | 18.38 | 0 |
| Percentage of neutrophil (%) | 148 | 82.43 ± 7.59 | 73.23 ± 6.32* | 72.40 ± 6.64* | 9.14 | 0 |
Table 2. Comparison of percentage of white blood cell count, neutrophil count and percentage of neutrophil (͞x ± s).
Comparison of inflammatory cytokines and biochemical indexes (͞x ± s)
We recorded and statistically analyzed the inflammatory factors and the level of serum biochemical indexes in patients after operation. 6 weeks after treatment, the hs-CRP, TNF-α, IL-1β, IL-6,IL-8 and other indicators were significantly lower than that before treatment, the difference was statistically significant (P<0.05), which is specifically shown in Table 3. Serum creatinine, blood urea nitrogen, serum total bilirubin, alanine aminotransferase, serum amylase, etc., were significantly lower than that before treatment (P<0.05) (Table 4).
| Items | Cases (n) | Before treatment | 3 weeks after treatment | 6 weeks after treatment | F value | P value |
|---|---|---|---|---|---|---|
| Hs-CRP (mg/L) | 148 | 217.6 ± 23.4 | 168.7 ± 10.8* | 91.2 ± 3.1*# | 12.83 | 0.03 |
| TNF-α (pg/mL) | 148 | 647.9 ± 201.3 | 1004.5 ± 121.7* | 921.7 ± 22.8*# | 18.45 | 0.01 |
| IL-1β (pg/mL) | 148 | 728.4 ± 21.8 | 403.4 ± 22.8* | 271.6 ± 12.7*# | 29.4 | 0.01 |
| IL-6 (pg/mL) | 148 | 602.4 ± 31.7 | 315.4 ± 12.9* | 104.7 ± 21.7*# | 12.81 | 0.02 |
| IL-8 (pg/mL) | 148 | 602.3 ± 22.3 | 366.4 ± 12.7* | 217.3 ± 8.2*# | 10.6 | 0.02 |
Table 3. Comparison of inflammatory cytokines (͞x ± s).
| Items | Cases (n) | Before treatment | 3 weeks after treatment | 6 weeks after treatment | F value | P value |
|---|---|---|---|---|---|---|
| Scr (μmol/L) | 32 | 439.4 ± 38.6 | 377.3 ± 32.4* | 236.5 ± 50.7*# | 3.89 | 0.02 |
| BUN (mmol/L) | 32 | 27.4 ± 13.4 | 18.3 ± 3.4* | 14.4 ± 23.5*# | 17.65 | 0.01 |
| TBIL (μmol/L) | 32 | 56.4 ± 21.8 | 77.8 ± 23.5* | 68.4 ± 12.7*# | 9.29 | 0 |
| ALT (U/L) | 32 | 91.4 ± 21.5 | 69.4 ± 13.3* | 47.3 ± 12.8*# | 10.08 | 0.01 |
| AMS (U/L) | 32 | 817.8 ± 212.5 | 611.3 ± 1.4* | 510.3 ± 1.3*# | 10.87 | 0.02 |
Table 4. Comparison of biochemical indexes (͞x ± s).
Correlation analysis of risk factors of postoperative infection
Logistic regression analysis of relationship between multiple risk factors and the CD4+/CD8+ ratio were analyzed after biliary stent implantation. The risk factors included gender, age (y), SBP (mmHg), DBP (mmHg), AST (U/L), ALT (U/L), logGGT (U/L), FPG (mmol/L), BMI (kg/m2), WBC (× 109/L), Scr (μmol/L), BUN (mmol/L), TBIL (μmol/L), AMS (U/L), Hs-CRP (mg/L), TNF-α (pg/mL), IL-1β (pg/mL), IL-8 (pg/ mL), IL-6 (pg/mL), Neutrophil count (× 109/L), neutrophil percentage (%), CD4+ T cell count (cells/μL), percentage of CD4+ T cells (%), CD8+ T cell count (cells/μL) and percentage of CD8+ T cells (%) (Tables 5-7).
| Items | Age | SBP (mmHg) | DBP (mmHg) | AST (U/L) | ALT (U/L) | Log GGT (U/L) | FPG (mmol/L) | BMI (kg/m2) | |
|---|---|---|---|---|---|---|---|---|---|
| CD4+/CD8+ | r | 0.351 | 0.116 | 0.328 | 0.124 | 0.415 | 0.106 | 0.238 | 0.114 |
| P | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
Table 5. Correlation between CD4+/CD8+ and Age, SBP, DBP, etc.
| Items | WBC (× 109/L) | Scr (μmol/L) | BUN (mmol/L) | TBIL (μmol/L) | AMS (U/L) | Hs-CRP (mg/L) | TNF-α (pg/mL) | IL-1β (pg/mL) | IL-8 (pg/mL) | IL-6 (pg/mL) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CD4+/CD8+ | r | -0.021 | -0.351 | -0.161 | -0.482 | -0.283 | -1.027 | 1.063 | -0.381 | -0.191 | -0.141 |
| P | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | <0.05 | <0.05 | >0.05 | >0.05 | >0.05 |
Table 6. Correlation between CD4+/CD8+ and WBC, Scr, BUN, TBIL, etc.
| Items | Neutrophil count (109/L) | The neutrophil percentage (%) | CD4+ T cell count (cells/μL) | Percentage of CD4+ T cells (%) | CD8+ T cell count (cells/μL) | The percentage of CD8+ T cells (%) | |
|---|---|---|---|---|---|---|---|
| CD4+/CD8+ | r | 0.02 | 0.35 | 0.16 | 0.28 | 0.24 | 0.15 |
| P | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
Table 7. Correlation between CD4+/CD8+ and neutrophil count, neutrophil percentage, etc.
Discussion
Previous studies have indicated that MOJ may increase the risk of infection after biliary stent implantation. The reasons can be categorized as follows [11,12]: Retrograde infection of biliary tract, low immunity, disruption of intestinal mucosal barrier, etc. In this study, we found various indicators of postoperative infection 3 weeks after surgery, the absolute value of CD4+ T lymphocytes in patients significantly increased (P<0.05). After 6 weeks of follow-up, the proportion of CD4+/CD8+ increased compared with that before biliary stent implantation, the difference was statistically significant (P<0.05), while the white blood cells, neutrophils were not significantly improved (P>0.05). As a good medium of bile bacteria, when the intestinal juice reflux, it becomes extremely easy to break out retrograde infection from biliary tract [13] .The characteristics of tumor, malnutrition, hyperbilirubinemia, endotoxemia and preoperative radiotherapy and chemotherapy had complicated effects on the immune function of patients. We speculated that the bile deficiency in the gut when bile duct obstruction occurs, the CD4+, CD8+ T lymphocytes and IgA were significantly decreased in the intestinal mucosa [14,15]. It decreased concentration of intestinal secretory IgA and reduced the intestinal immune function, leading to bacterial translocation [16,17]. It has been reported that cytokines also play an important role in this process. Endotoxin stimulates the production of Tumor Necrosis Factor (TNF), which inhibits the immune function of the host cells [18].
In addition, we found in our study, 6 weeks later, hs-CRP, TNF-α, IL-1β, IL-6, IL-8 and other indicators were significantly lower than that before treatment, the difference was statistically significant (P<0.05). Serum creatinine, blood urea nitrogen, serum total bilirubin, alanine aminotransferase, serum amylase and so on were significantly lower than that of before treatment (P<0.05). Many studies have indicated that the inflammatory mediators play an important role in malignant obstructive jaundice [19]. Prostaglandin E (PGE) [20] inhibited T lymphocyte to produce Interferon (INF) and Interleukin-2 (IL-2), which inhibits the activation of T lymphocyte proliferation and the T lymphocyte subsets, so that the activity of NK cells was decreased consequently. In addition, endotoxin could damage the function of mononuclear phagocytic system, and the activity of Kupfer cells in liver was inhibited. Phagocytosis and killing activity of liver cells decreased, which inhibits the immune function [21]. It has been indicated that both inflammatory response and immune dysfunction are the key steps in the development of traumatic (including surgery) sepsis and MODS.
In our study, we found that the risk factors of postoperative infection included gender, age (y), SBP (mmHg), DBP (mmHg), AST (U/L), ALT (U/L), logGGT (U/L), FPG (mmol/L), BMI (kg/m2), WBC (× 109/L), Scr (μmol/L), BUN (mmol/L), TBIL (μmol/L), AMS (U/L), Hs-CRP (mg/L), TNF- α (pg/mL), IL-1β (pg/mL), IL-8 (pg/mL), IL-6 (pg/mL), neutrophil count (× 109/L), neutrophil percentage (%), CD4+ T cell count (cells/μL), percentage of CD4+ T cells (%), CD8+ T cell count (cells/μL) and percentage of CD8+ T cells (%) [22-25]. In MOJ, due to the lack of bile, intestinal mucosal chemical barrier is easily impaired [26]. Bile salt deficiency is a reason of nutrient absorption, intestinal mucosal atrophy, changes of intestinal mucosal morphology and decreased electrical activity of smooth muscle [27]. In MOJ, under the light microscope, the thin ileum mucosa, blunt and sparse villi, edematous epithelium, and the separated epithelial layer from laminae propria of the mucosa can be seen. Under the electron microscope, it characterized as the shed partial epithelial tissue, vacuole cytoplasm, formation of phagocytosis of dissolved body, broken tight junctions between cells, swollen mitochondria and ridge fracture, which caused damage to the mechanical barrier [28].
In summary, we believe that biliary stent implantation in patients with malignant obstructive jaundice will significantly improve the cholestasis. The proportion of CD4+/CD8+ T lymphocytes was increased, by which induced and improved the immune system function, thus reducing the incidence of infection of patients with malignant obstructive jaundice, and will significantly improve their quality of life.
Acknowledgement
This study was supported by Capital Citizen Health Project Nurture of Beijing (clinical research of preoperative intraintestinal immune nutrition intervention for biliary stent implantation in malignant obstructive jaundice, Z131100006813010).
References
- Yamamoto R, Takahashi M, Osafune Y. Comparison of endoscopic stenting for malignant biliary obstruction: A single-center study. World J Gastrointest Endosc 2015; 7: 889-894.
- Andruszkow H, Fischer J, Sasse M. Interleukin-6 as inflammatory marker referring to multiple organ dysfunction syndromes in severely injured children. Scand J Trauma Resusc Emerg Med 2014; 22: 16.
- Phillipo LC, Emmanuel SK, Mabula M. Etiological spectrum and treatment outcome of Obstructive jaundice at a University teaching Hospital in North-western Tanzania: A diagnostic and therapeutic challenges. BMC Res Notes 2011; 4: 1-7.
- Kallis Y, Phillips N, Steel A. Analysis of endoscopic radiofrequency ablation of biliary malignant strictures in pancreatic cancer suggests potential survival benefit. Dig Dis Sci 2015; 60: 3449-3455.
- Wang SB, Wu HB, Wang QS. 18F-FDG PET/CT in differentiating malignant from benign origins of obstructive jaundice. Hepatobiliary Pancreatic Dis Int 2015; 14: 5166-5222.
- Yu H, Wu S, Yu X. Single-incision laparoscopic biliary bypass for malignant obstructive jaundice. J Gastrointest Surg 2015; 19: 1132-1138.
- Fan WD, Nie HF, Chen YB. Influence of malignant severe obstructive jaundice on immune function and therapeutic effects of immunopotentiator. J Hepatopancreatobiliary Surg 2013; 25: 35-38.
- Patel P, Rangarajan B, Mangat K. Improved accuracy of percutaneous biopsy using “Cross and Push” technique for patients suspected with malignant biliary strictures. Cardiovasc Interventional Radiol 2015; 38: 1005-1010.
- Aswad MG, Dennison AR, Neal CP. Biliary stenting for benign and malignant obstructive jaundice: safe use of extended stent-change intervals. Surg Laparosc Endosc Percutan Tech 2014; 24: 385-390.
- Brunson BA, Hawes R, Hoffman B. Poor ‘real-life’ negative predictive value of cross-sectional imaging in obstructive jaundice. Can J Gastroenterol Hepatol 2014; 28: 385-390.
- Semi P, Jeong YP, Moon JC. The efficacy of endoscopic palliation of obstructive jaundice in hepatocellular carcinoma. Yonsei Med J 2014; 55: 1267-1272.
- Artifon EL, Otoch JP, Tchekmedyian AJ. A review on endoscopic palliation of obstructive jaundice before surgery. Rev Gastroenterol Perú 2014; 34: 225-228.
- Pan H, Liang Z, Yin TS. Hepato-biliary-enteric stent drainage as palliative treatment for proximal malignant obstructive jaundice. Med Oncol 2014; 31: 853.
- Li TF, Ren KW, Han XW. Percutaneous transhepatic cholangiobiopsy to determine the pathological cause of anastomotic stenosis after cholangiojejunostomy for malignant obstructive jaundice. Clin Radiol 2014; 69: 13-17.
- Xu C, Lv PH, Huang XE. Internal-external percutaneous transhepatic biliary drainage for patients with malignant obstructive jaundice. Asian Pac J Cancer Prev 2014; 15: 9391-9394.
- Javia SB, Patel R, Singhal S. Endoscopic closure with an over-the-scope clip of a duodenocolonic fistula caused by a migrated biliary stent. Gastrointest Endosc 2016; 83: 845-846.
- Moon JH, Rerknimitr R, Kogure H. Topic controversies in the endoscopic management of malignant hilar strictures using metal stent: side-by-side versus stent-in-stent techniques. J Hepatobiliary Pancreat Sci 2015; 22: 650-656.
- Matsumoto K, Kato H, Tsutsumi K. Successful biliary drainage using a metal stent through the gastric stoma. World J Gastroenterol 2015; 21: 7594-7597.
- Sejpal DV, Vamadevan AS, Trindade AJ. Removal of an embedded, migrated plastic biliary stent with the use of cholangioscopy. Gastrointest Endosc 2015; 81: 1482-1483.
- Sanaka MR, Wadhwa V, Patel M. Retrieval of proximally migrated biliary stent with direct peroral cholangioscopy with an ultraslim endoscope. Gastrointest Endosc 2015; 81: 1483-1484.
- Assimakopoulos SF, Tsamandas AC, Louvros E. Intestinal epithelial cell proliferation, apoptosis and expression of tight junction proteins in patients with obstructive jaundice. Eur J Clin Invest 2011; 41: 117-125.
- Miyazaki M, Shibuya K, Tokue H. Percutaneous transhepatic biliary drainage assisted by real-time virtual sonography: a retrospective study. BMC Gastroenterol 2013; 13: 127.
- Bun Teoh AY, Ning Chong CC, Wong Lau JY. Video of the month: eus-guided choledochoduodenstomy with a cautery-equipped lumen-apposing stent allows future biliary access in patients with type 2 duodenal obstruction. Am J Gastroenterol 2015; 110: 800.
- Zi-Kai W, Jian-Guo X, Xue-Fei H. Effect of biliary drainage on inducible nitric oxide synthase, CD14 and TGR5 expression in obstructive jaundice rats. World J Gastroenterol 2013; 19: 2319-2330.
- Lyon M, Menon S, Jain A. Use of biliary stent in laparoscopic common bile duct exploration. Surg Endosc 2015; 29: 1094-1098.
- Joseph PM, Joseph C. The changing pattern and implications of Multiple Organ Failure (MOF) after blunt injury with hemorrhagic shock. Crit Care Med 2012; 40: 1129-1135.
- Griffith M, Peter JV, Karthik G. Profile of organ dysfunction and predictors of mortality in severe scrub typhus infection requiring intensive care admission. Indian J Crit Care Med 2014; 18: 497-502.
- Naitoh I, Nakazawa T, Ban T. 8-mm versus 10-mm diameter self-expandable metallic stent in bilateral endoscopic stent-in-stent deployment for malignant hilar biliary obstruction. J Hepatobiliary Pancreat Sci 2015; 22: 396-401.